Mal De Meleda in a Taiwanese
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Keratosis Circumscripta Revisited: a Case Report and Review of the Literature
CONTINUING MEDICAL EDUCATION Keratosis Circumscripta Revisited: A Case Report and Review of the Literature LCDR Eric P. Brumwell, MC, USN; LCDR Sean J. Murphy, MC, USN GOAL To understand keratosis circumscripta to better manage patients with the condition OBJECTIVES Upon completion of this activity, dermatologists and general practitioners should be able to: 1. Describe the clinical presentation of keratosis circumscripta. 2. Discuss the disorders often compared to keratosis circumscripta. 3. Identify treatment options for keratosis circumscripta. CME Test on page 378. This article has been peer reviewed and approved Einstein College of Medicine is accredited by by Michael Fisher, MD, Professor of Medicine, the ACCME to provide continuing medical edu- Albert Einstein College of Medicine. Review date: cation for physicians. April 2007. Albert Einstein College of Medicine designates This activity has been planned and imple- this educational activity for a maximum of 1 AMA mented in accordance with the Essential Areas PRA Category 1 CreditTM. Physicians should only and Policies of the Accreditation Council for claim credit commensurate with the extent of their Continuing Medical Education through the participation in the activity. joint sponsorship of Albert Einstein College of This activity has been planned and produced in Medicine and Quadrant HealthCom, Inc. Albert accordance with ACCME Essentials. Drs. Brumwell and Murphy report no conflict of interest. The authors report no discussion of off-label use. Dr. Fisher reports no conflict of interest. Keratosis circumscripta, also known as psoriasis been shown to improve, but not resolve, with kerat- circumscripta with palmoplantar keratosis, is a inolytic therapies. Some debate exists concern- rarely reported condition that manifests as well- ing the terminology used to identify this condition. -

WES Gene Package Multiple Congenital Anomalie.Xlsx
Whole Exome Sequencing Gene package Multiple congenital anomalie, version 5, 1‐2‐2018 Technical information DNA was enriched using Agilent SureSelect Clinical Research Exome V2 capture and paired‐end sequenced on the Illumina platform (outsourced). The aim is to obtain 8.1 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA‐MEM algorithm (reference: http://bio‐bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x A4GALT [Blood group, P1Pk system, P(2) phenotype], 111400 607922 101 100 100 99 [Blood group, P1Pk system, p phenotype], 111400 NOR polyagglutination syndrome, 111400 AAAS Achalasia‐addisonianism‐alacrimia syndrome, 231550 605378 73 100 100 100 AAGAB Keratoderma, palmoplantar, -
The First Reported Case of a Variant of Mal De Maleda of the Gamborg
Our Dermatology Online Case Report Th e fi rrstst rreportedeported ccasease ooff a vvariantariant ooff MMalal ddee MMaledaaleda ooff tthehe GGamborg-Nielsenamborg-Nielsen ttypeype iinn aann EEgyptiangyptian ooriginrigin ppatientatient Khalid M. Al-Husain1, Ahmed A. Al-Thubaiti1, Farah M. Alzahrani2, Iqbal A. Bukhari3, Mohammad El-Shawarby4 1College of Medicine, Imam Abdulrahman Bin Faisal University (IAU), Dammam, Kingdom of Saudi Arabia, 2College of Medicine, Arabian Gulf University (AGU), Bahrain, 3Dermatology Department, College of Medicine, Imam Abdulrahman Bin Faisal University (IAU) and King Fahd Hospital of the University, Dammam, Kingdom of Saudi Arabia, 4Pathology Department, College of Medicine, Imam Abdulrahman Bin Faisal University (IAU) and King Fahd Hospital of the University, Dammam, Kingdom of Saudi Arabia Corresponding author: Prof. Iqbal A. Bukhari, E-mail: [email protected] ABSTRACT Mal de Meleda is a rare genodermatosis with an autosomal recessive inheritance. Mutations in the SLURP1 gene are the cause of this disease. Clinically, it is characterized by progressive palmoplantar hyperkeratosis exhibiting a transgradiens pattern extending to the dorsal aspects of the hands and feet in a glove and stocking pattern. It is also associated with hyperhidrosis, nail changes, subungual hyperkeratosis and perioral erythema. Here we report the first case of Gamborg-Nielsen variant of Mal de Meleda disorder in a patient of an Egyptian origin. Key words: Mal de Meleda; Keratoderma; Genodermatosis; SLURP1 gene INTRODUCTION in -

(12) Patent Application Publication (10) Pub. No.: US 2010/0210567 A1 Bevec (43) Pub
US 2010O2.10567A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/0210567 A1 Bevec (43) Pub. Date: Aug. 19, 2010 (54) USE OF ATUFTSINASATHERAPEUTIC Publication Classification AGENT (51) Int. Cl. A638/07 (2006.01) (76) Inventor: Dorian Bevec, Germering (DE) C07K 5/103 (2006.01) A6IP35/00 (2006.01) Correspondence Address: A6IPL/I6 (2006.01) WINSTEAD PC A6IP3L/20 (2006.01) i. 2O1 US (52) U.S. Cl. ........................................... 514/18: 530/330 9 (US) (57) ABSTRACT (21) Appl. No.: 12/677,311 The present invention is directed to the use of the peptide compound Thr-Lys-Pro-Arg-OH as a therapeutic agent for (22) PCT Filed: Sep. 9, 2008 the prophylaxis and/or treatment of cancer, autoimmune dis eases, fibrotic diseases, inflammatory diseases, neurodegen (86). PCT No.: PCT/EP2008/007470 erative diseases, infectious diseases, lung diseases, heart and vascular diseases and metabolic diseases. Moreover the S371 (c)(1), present invention relates to pharmaceutical compositions (2), (4) Date: Mar. 10, 2010 preferably inform of a lyophilisate or liquid buffersolution or artificial mother milk formulation or mother milk substitute (30) Foreign Application Priority Data containing the peptide Thr-Lys-Pro-Arg-OH optionally together with at least one pharmaceutically acceptable car Sep. 11, 2007 (EP) .................................. O7017754.8 rier, cryoprotectant, lyoprotectant, excipient and/or diluent. US 2010/0210567 A1 Aug. 19, 2010 USE OF ATUFTSNASATHERAPEUTIC ment of Hepatitis BVirus infection, diseases caused by Hepa AGENT titis B Virus infection, acute hepatitis, chronic hepatitis, full minant liver failure, liver cirrhosis, cancer associated with Hepatitis B Virus infection. 0001. The present invention is directed to the use of the Cancer, Tumors, Proliferative Diseases, Malignancies and peptide compound Thr-Lys-Pro-Arg-OH (Tuftsin) as a thera their Metastases peutic agent for the prophylaxis and/or treatment of cancer, 0008. -

Palmoplantar Keratoderma of the Gamborg-Nielsen Type Is Caused by Mutations in the SLURP1 Gene and Represents a Variant of Mal De Meleda
Acta Derm Venereol 2014; 94: 707–710 CLINICAL REPORT Palmoplantar Keratoderma of the Gamborg-Nielsen Type is Caused by Mutations in the SLURP1 Gene and Represents a Variant of Mal de Meleda Linshu ZHAO1, Anders VAHLQUIST2*, Marie VIRtanen2, Lena WENNERSTRAND3, Lisbet K. LIND3, Anita LUNDSTRÖM4 and Maritta HELLSTRÖM PIGG1 Departments of 1Immunology, Genetics and Pathology and 2Medical Sciences, Uppsala University, Uppsala, and 3Departments of Medical Biosciences, Medical and Clinical Genetics and 4Public Health and Clinical Medicine, Umeå University, Umeå, Sweden Palmoplantar keratoderma of the Gamborg-Nielsen also observed. Mal de Meleda (MDM; OMIM 248300) type (PPK-GN) is a rare autosomal recessive skin disor- or keratosis palmoplantaris transgradiens of Siemens der described in patients from Sweden. Mal de Meleda is an autosomal recessive skin disorder first described (MDM) is also a rare autosomal recessive inherited PPK in 1898 by Neumann (2) in patients from the island of first reported in 5 families from the island of Meleda. Mljet (Meleda) in Dalmatia, Croatia. MDM is clinically The 2 conditions phenotypically overlap and are charac- characterised by symmetric transgressive PPK, and so- terised by palmoplantar erythematous hyperkeratotic metimes associated with lichenoid or keratotic plaques plaques. The genetic background giving rise to PPK-GN over joints, redness in the palms and soles, brachydactyly, has hitherto been unknown, whereas MDM is known to cone-shaped fingers, pseudoainhum and nail abnorma- be caused by mutations in the gene encoding secreted lities with pachyonychia. The progressive lesions can Ly-6/uPAR-related protein 1, SLURP-1. In the present lead to reduced mobility of hands and feet because of study we scrutinised individuals affected by PPK-GN for contractions (2–8). -

Towards a Comprehensive Resource for Elucidating the Pathogenesis of Inherited Keratodermas
Towards a Comprehensive Resource for Elucidating the Pathogenesis of Inherited Keratodermas Dr Mozheh Zamiri BSc (Hons), MB ChB, MRCP Doctorate of Medicine University of Edinburgh 2009 Alan Lyell Centre for Dermatology, Glasgow & Section of Dermatology, University of Glasgow ABSTRACT Keratoderma – pathological hyperkeratosis of palms and soles - is a cause of disability in many clinical situations, including the rare and heterogeneous group of inherited palmoplantar keratodermas (PPKs). The aim of this study was to work towards better understanding of molecular mechanisms active in the pathogenesis of PPK by the creation of a cell and tissue culture resource and its initial application to laboratory studies. My study was based on a diverse group of autosomal dominant disorders, previously ascertained in families from Scotland, in whom the precise genetic aetiology was known. I established a tissue and cell culture resource of inherited keratodermas of known single-gene aetiology from patients with proven keratin 1, 9, 17, loricrin and mitochondrial mutations. An additional pedigree with striate keratoderma with an unknown mutation was recruited, and the causative mutation identified as a novel heterozygous A-to-T transversion in exon 5 (c.430A>T) of the desmoglein 1 gene, converting an arginine residue to a premature termination codon (p.Arg144stop). The keratinocyte culture resource was established from patients with keratin 1, 9, 17 and loricrin mutations, as well as controls. Due to the pain associated with direct infiltration of plantar skin, biopsies were obtained using peripheral nerve block for plantar biopsy. The effectiveness of this approach, which may be useful for future administration of treatment, was made the subject of an open clinical trial. -

Keratinization Disorders and Genetic Aspects in Palmar and Plantar Keratodermas
Acta Dermatovenerol Croat 2016;24(2):116-123 CLINICAL ARTICLE Keratinization Disorders and Genetic Aspects in Palmar and Plantar Keratodermas Ewa Stypczyńska1, Waldemar Placek2, Barbara Zegarska3, Rafał Czajkowski1 1Nicolaus Copernicus University in Toruń, Faculty of Medicine, Chair of Dermatology, Sexually Transmitted Diseases and Immunodermatology, Bydgoszcz, Poland; 2Depart- ment of Dermatology, Sexually Transmitted Diseases and Clinical Immunology, Univer- sity of Warmia and Mazury, Olsztyn, Poland; 3Nicolaus Copernicus University in Toruń, Faculty of Pharmacy, Department of Cosmetology and Esthetic Dermatology, Bydgo- szcz, Poland Corresponding author: ABSTRACT Palmoplantar keratoderma (PPK) is a heterogeneous group Rafal Czajkowski, MD, PhD of hereditary and acquired disorders characterized by abnormal thick- ening of the palms and soles. There are three clinical patterns: diffuse, Nicolaus Copernicus University in Toruń focal, and punctuate. Palmoplantar keratodermas can be divided into the Faculty of Medicine following functional subgroups: disturbed gene functions in structural Chair of Dermatology, Sexually Transmitted proteins (keratins), cornified envelope (loricrin, transglutaminase), cohe- Diseases and Immunodermatology sion (plakophilin, desmoplakin, desmoglein 1), cell-to-cell communica- tion (connexins) and transmembrane signal transduction (cathepsin C). Bydgoszcz Unna-Thost disease is the most common variety of hereditary PPK. Muta- Poland tions in keratin 1 have been reported in Unna-Thost disease. We report [email protected] -

Download CGT Exome V2.0
CGT Exome version 2. -

A CASE of MAL DE MELEDA DISEASE in CHITRADURGA - KARNATAKA Parvathi C
DOI: 10.14260/jemds/2014/3906 CASE REPORT A CASE OF MAL DE MELEDA DISEASE IN CHITRADURGA - KARNATAKA Parvathi C. N1, Yogendra M2, Raghu M. T3, Kavyashree K. L4, Thippareddy G. T5 HOW TO CITE THIS ARTICLE: Parvathi C. N, Yogendra M, Raghu M. T, Kavyashree K. L, Thippareddy G. T. “A Case of Mal De Meleda Disease in Chitradurga-Karnataka”. Journal of Evolution of Medical and Dental Sciences 2014; Vol. 3, Issue 65, November 27; Page: 14224-14229, DOI: 10.14260/jemds/2014/3906 ABSTRACT: Mal de Meleda is a rare autosomal recessive palmoplantar keratoderma characterized by transgradient keratoderma with associated scleroatrophy, knee changes and onychogryphosis. This case of a 20 year old girl born of second degree consanguineous marriage is reported for its uniqueness in conformity with criteria enunciated by Stulli associated with hyperkeratotic warty papules clinically fitting into Darier’s disease with lip involvement. Another interesting feature being black pigmentation of fingers and nails which was due to cashew nut shell paste application mistaken for dry gangrene. KEYWORDS: Mal de Meleda, palmoplantar keratoderma, Onychogryphosis. INTRODUCTION: Mal de Meleda disease was first described by Stulli of Ragusa in 1826, named after Croatian island of Meleda, with wide spectrum of skin manifestations characterized by1,2 clinical features such as autosomal recessive inheritance with onset of diffuse palmoplantar keratoderma soon after birth associated with transgradience and glove and stocking keratoderma involving dorsa of hands and fingers, feet, toes, flexor aspect of wrist with sharp margin. Globally there are four reports of this clinical condition.3,4,5 The other associated features are palmoplantar hyperhidrosis, pitting, lichenoid plaques on the elbows, knees and groins, subungual keratoderma, koilonychia, dystrophy of great toe nail, progressive conical tapering of the finger tips, perioral erythema., high arched palate and corneal lesion. -

NGS Oncology)
UNIVERSITY OF MINNESOTA PHYSICIANS OUTREACH LABS Submit this form along with the appropriate Molecular requisition (Molecular Diagnostics or MOLECULAR DIAGNOSTICS (612) 273-8445 DATE: TIME COLLECTED: PCU/CLINIC: Molecular NGS Oncology). AM PM PATIENT IDENTIFICATION DIAGNOSIS (Dx) / DIAGNOSIS CODES (ICD-9) - OUTPATIENTS ONLY SPECIMEN TYPE: o Blood (1) (2) (3) (4) PLEASE COLLECT 5-10CC IN ACD-A OR EDTA TUBE ORDERING PHYSICIAN NAME AND PHONE NUMBER: Tests can be ordered as a full panel, or by individual gene(s). Please contact the genetic counselor with any questions at 612-624-8948 or by pager at 612-899-3291. _______________________________________________ Test Ordered- EPIC: Next generation sequencing(Next Gen) Sunquest: NGS Ectodermal dysplasia epidermolysis bullosa simplex with Acne inversa muscular dystrophy Full panel PLEC Full panel EDA Epidermolytic hyperkeratosis NCSTN EDARADD Full panel PSENEN MSX1 KRT1 PSEN1 KRT85 KRT10 Acrodermatitis enteropathica PVRL4 Erythroderma, congenital, with NFKBIA palmoplantar keratoderma, SLC39A4 IKBKG hypotrichosis, and hyper IgE Amyloidosis, primary localized Ectodermal dysplasia/skin fragility DSG1 cutaneous, 1 syndrome Erythrokeratodermia variabilis with PKP1 erythema gyratum repens Full panel Ectrodactyly, ectodermal dysplasia, GJB4 OSMR and cleft lip/palate syndrome 3 Familial benign pemphigus IL31RA TP63 ATP2C1 Atrichia with papular lesions Focal facial dermal dysplasia 3 Focal dermal hypoplasia TWIST2 HR PORCN Epidermodysplasia verruciformis Autosomal recessive hypohidrotic Glomuvenous malformations -

Whole Exome Sequencing Gene Package Multiple Congenital Anomaly, Version 8.1, 31-1-2020
Whole Exome Sequencing Gene package Multiple congenital anomaly, version 8.1, 31-1-2020 Technical information DNA was enriched using Agilent SureSelect DNA + SureSelect OneSeq 300kb CNV Backbone + Human All Exon V7 capture and paired-end sequenced on the Illumina platform (outsourced). The aim is to obtain 10 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate and non-unique reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA-MEM algorithm (reference: http://bio-bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x A4GALT [Blood group, P1Pk system, P(2) phenotype], 111400 [Blood group, P1Pk system, p phenotype], 111400 NOR poly607922 146 100 100 99 AAAS Achalasia-addisonianism-alacrimia syndrome, 231550 605378 102 100 100 100 -
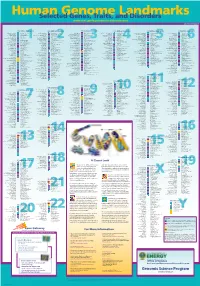
Genomeposter2009.Pdf
Fold HumanSelected Genome Genes, Traits, and Landmarks Disorders www.ornl.gov/hgmis/posters/chromosome genomics.energy.