A Harmonized Meta-Knowledgebase of Clinical Interpretations of Cancer Genomic Variants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protein Biomarkers Analysis Within Muscular Dystrophies
EXAMENSARBETE INOM BIOTEKNIK, AVANCERAD NIVÅ, 30 HP STOCKHOLM, SVERIGE 2017 Protein biomarkers analysis within muscular dystrophies SANDRA MENA KTH SKOLAN FÖR BIOTEKNOLOGI PROTEIN BIOMARKERS ANALYSIS WITHIN MUSCULAR DYSTROPHIES Master thesis Author: Sandra Carolina Mena Pérez Supervisor: Cristina Al-Khalili Szigyarto Stockholm 2017 Master’s program: Medical Biotechnology Kungliga Tekniska Högskolan Content Abstract .........................................................................................................................................................1 Abstrakt .........................................................................................................................................................1 Introduction .................................................................................................................................................1 Materials and Methods ............................................................................................................................ 3 Results and Discussion ............................................................................................................................ 4 Conclusion .................................................................................................................................................. 11 Future Perspectives ................................................................................................................................. 11 Aknowledgments .................................................................................................................................... -

Integration of the Drug-Gene Interaction Database (Dgidb) with Open Crowdsource Efforts
bioRxiv preprint doi: https://doi.org/10.1101/2020.09.18.301721; this version posted September 20, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Integration of the Drug-Gene Interaction Database (DGIdb) with open crowdsource efforts Sharon Freshour1,2,†, Susanna Kiwala2,†, Kelsy C. Cotto1,2,†, Adam C. Coffman2, Joshua F. McMichael2, Jonathan Song1,2, Malachi Griffith1,2,3,4,*, Obi L. Griffith1,2,3,4,*, Alex H. Wagner1,2,5,6,* 1 Department of Medicine, Division of Oncology, Washington University School of Medicine, St Louis, MO, 63110, USA 2 McDonnell Genome Institute, Washington University School of Medicine, St Louis, MO, 63108, USA 3 Department of Genetics, Washington University School of Medicine, St Louis, MO, 63110, USA 4 Siteman Cancer Center, Washington University School of Medicine, St Louis, MO, 63110, USA 5 The Steve and Cindy Rasmussen Institute for Genomic Medicine, Nationwide Children’s Hospital, Columbus, OH, 43215, USA 6 Department of Pediatrics, The Ohio State University College of Medicine, Columbus, OH, 43210, USA * To whom correspondence should be addressed. Tel: 1-614-355-1645; Fax: 1-614-355-6833; Email: [email protected] Correspondence may also be addressed to Obi L. Griffith. Tel: 1-314-747-9248; Fax: 1-314-286-1810; Email: [email protected] Correspondence may also be addressed to Malachi Griffith. Tel: 1-314-286-1274; Fax: 1-314-286-1810; Email: [email protected] † The authors wish it to be known that, in their opinion, the first three authors should be regarded as joint First Authors ABSTRACT The Drug-Gene Interaction Database (DGIdb, www.dgidb.org) is a web resource that provides information on drug-gene interactions and druggable genes from various sources including publications, databases, and other web-based sources in one resource. -
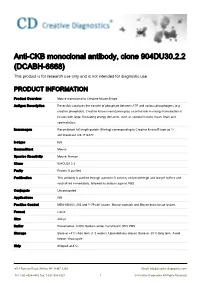
Anti-CKB Monoclonal Antibody, Clone 904DU30.2.2 (DCABH-6668) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-CKB monoclonal antibody, clone 904DU30.2.2 (DCABH-6668) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Mouse monoclonal to Creatine kinase B type Antigen Description Reversibly catalyzes the transfer of phosphate between ATP and various phosphogens (e.g. creatine phosphate). Creatine kinase isoenzymes play a central role in energy transduction in tissues with large, fluctuating energy demands, such as skeletal muscle, heart, brain and spermatozoa. Immunogen Recombinant full length protein (His-tag) corresponding to Creatine kinase B type aa 1- 381.Database link: P12277 Isotype IgG Source/Host Mouse Species Reactivity Mouse, Human Clone 904DU30.2.2 Purity Protein G purified Purification This antibody is purified through a protein G column, eluted with high and low pH buffers and neutralized immediately, followed by dialysis against PBS. Conjugate Unconjugated Applications WB Positive Control MDA-MB453; 293 and Y-79 cell lysates; Mouse stomach and Mouse brain tissue lysates Format Liquid Size 400 μl Buffer Preservative: 0.09% Sodium azide; Constituent: 99% PBS Storage Store at +4°C short term (1-2 weeks). Upon delivery aliquot. Store at -20°C long term. Avoid freeze / thaw cycle. Ship Shipped at 4°C. 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved GENE INFORMATION Gene Name CKB creatine kinase, brain [ Homo sapiens ] Official Symbol CKB Synonyms CKB; creatine -

JAX-CKB), Which Can Be Queried Readily to Access Comprehensive Data for Clinical Reporting Via Customized Reporting Queries
Patterson et al. Human Genomics (2016) 10:4 DOI 10.1186/s40246-016-0061-7 PRIMARY RESEARCH Open Access The clinical trial landscape in oncology and connectivity of somatic mutational profiles to targeted therapies Sara E. Patterson, Rangjiao Liu, Cara M. Statz, Daniel Durkin, Anuradha Lakshminarayana and Susan M. Mockus* Abstract Background: Precision medicine in oncology relies on rapid associations between patient-specific variations and targeted therapeutic efficacy. Due to the advancement of genomic analysis, a vast literature characterizing cancer- associated molecular aberrations and relative therapeutic relevance has been published. However, data are not uniformly reported or readily available, and accessing relevant information in a clinically acceptable time-frame is a daunting proposition, hampering connections between patients and appropriate therapeutic options. One important therapeutic avenue for oncology patients is through clinical trials. Accordingly, a global view into the availability of targeted clinical trials would provide insight into strengths and weaknesses and potentially enable research focus. However, data regarding the landscape of clinical trials in oncology is not readily available, and as a result, a comprehensive understanding of clinical trial availability is difficult. Results: To support clinical decision-making, we have developed a data loader and mapper that connects sequence information from oncology patients to data stored in an in-house database, the JAX Clinical Knowledgebase (JAX-CKB), which can be queried readily to access comprehensive data for clinical reporting via customized reporting queries. JAX-CKB functions as a repository to house expertly curated clinically relevant data surrounding our 358-gene panel, the JAX Cancer Treatment Profile (JAX CTP), and supports annotation of functional significance of molecular variants. -
Profiling Haplotype Specific Cpg and Cph Methylation Within A
www.nature.com/scientificreports OPEN Profling haplotype specifc CpG and CpH methylation within a schizophrenia GWAS locus on chromosome 14 in schizophrenia and healthy subjects Margarita Alfmova*, Nikolay Kondratyev, Arkadiy Golov & Vera Golimbet Interrogating DNA methylation within schizophrenia risk loci holds promise to identify mechanisms by which genes infuence the disease. Based on the hypothesis that allele specifc methylation (ASM) of a single CpG, or perhaps CpH, might mediate or mark the efects of genetic variants on disease risk and phenotypes, we explored haplotype specifc methylation levels of individual cytosines within a genomic region harbouring the BAG5, APOPT1 and KLC1 genes in peripheral blood of schizophrenia patients and healthy controls. Three DNA fragments located in promoter, intronic and intergenic areas were studied by single-molecule real-time bisulfte sequencing enabling the analysis of long reads of DNA with base-pair resolution and the determination of haplotypes directly from sequencing data. Among 1,012 cytosines studied, we did not fnd any site where methylation correlated with the disease or cognitive defcits after correction for multiple testing. At the same time, we determined the methylation profle associated with the schizophrenia risk haplotype within the KLC1 fourth intron and confrmed ASM for cytosines located in the vicinity of rs67899457. These genetically associated DNA methylation variations may be related to the pathophysiological mechanism diferentiating the risk and non-risk haplotypes and merit further investigation. Schizophrenia is a common, highly heritable disorder characterized by positive, negative, and cognitive symp- toms. Large genome-wide association studies (GWAS) of the Psychiatric Genomics Consortium (PGC) have identifed more than 100 genomic regions that are signifcantly associated with schizophrenia1,2. -

Identification of Expression Qtls Targeting Candidate Genes For
ISSN: 2378-3648 Salleh et al. J Genet Genome Res 2018, 5:035 DOI: 10.23937/2378-3648/1410035 Volume 5 | Issue 1 Journal of Open Access Genetics and Genome Research RESEARCH ARTICLE Identification of Expression QTLs Targeting Candidate Genes for Residual Feed Intake in Dairy Cattle Using Systems Genomics Salleh MS1,2, Mazzoni G2, Nielsen MO1, Løvendahl P3 and Kadarmideen HN2,4* 1Department of Veterinary and Animal Sciences, Faculty of Health and Medical Sciences, University of Copenhagen, Denmark Check for 2Department of Bio and Health Informatics, Technical University of Denmark, Lyngby, Denmark updates 3Department of Molecular Biology and Genetics-Center for Quantitative Genetics and Genomics, Aarhus University, AU Foulum, Tjele, Denmark 4Department of Applied Mathematics and Computer Science, Technical University of Denmark, Lyngby, Denmark *Corresponding author: Kadarmideen HN, Department of Applied Mathematics and Computer Science, Technical University of Denmark, DK-2800, Kgs. Lyngby, Denmark, E-mail: [email protected] Abstract body weight gain and net merit). The eQTLs and biological pathways identified in this study improve our understanding Background: Residual feed intake (RFI) is the difference of the complex biological and genetic mechanisms that de- between actual and predicted feed intake and an important termine FE traits in dairy cattle. The identified eQTLs/genet- factor determining feed efficiency (FE). Recently, 170 can- ic variants can potentially be used in new genomic selection didate genes were associated with RFI, but no expression methods that include biological/functional information on quantitative trait loci (eQTL) mapping has hitherto been per- SNPs. formed on FE related genes in dairy cows. In this study, an integrative systems genetics approach was applied to map Keywords eQTLs in Holstein and Jersey cows fed two different diets to eQTL, RNA-seq, Genotype, Data integration, Systems improve identification of candidate genes for FE. -

Screening for the Proteins That Can Interact with Grouper Nervous Necrosis Virus Capsid Protein
viruses Article Screening for the Proteins That Can Interact with Grouper Nervous Necrosis Virus Capsid Protein 1, 2, 2 2 3 Po-Yu Huang y, Han-Chia Hsiao y, Szu-Wen Wang , Shao-Fu Lo , Ming-Wei Lu and Li-Li Chen 1,2,* 1 Center of Excellence for the Oceans, National Taiwan Ocean University, No. 2, Pei-Ning Road, Keelung 20224, Taiwan; [email protected] 2 Institute of Marine Biology, National Taiwan Ocean University, No. 2, Pei-Ning Road, Keelung 20224, Taiwan; [email protected] (H.-C.H.); [email protected] (S.-W.W.); [email protected] (S.-F.L.) 3 Department of Aquaculture, National Taiwan Ocean University, No. 2, Pei-Ning Road, Keelung 20224, Taiwan; [email protected] * Correspondence: [email protected] These authors contributed equally to this work. y Received: 17 August 2020; Accepted: 1 September 2020; Published: 4 September 2020 Abstract: Nervous necrosis virus (NNV) can infect many species of fish and has an 80–100% mortality rate. NNV capsid protein (NNVCP) is the only structural protein of NNV, but there are few studies on the protein–protein interaction between NNVCP and the host cell. To investigate NNV morphogenesis, native NNV capsid protein (NNVCP) was used to screen for protein–protein interactions in this study. The results identified that 49 grouper optic nerve proteins can interact with NNVCP and may function as putative receptor or co-receptor, cytoskeleton, glucose metabolism and ATP generation, immunity, mitochondrial ion regulation, and ribosomal proteins. Creatine kinase B-type (CKB) is one of those 49 optic nerve proteins. -

Computational Simulations to Predict Creatine Kinase-Associated Factors: Protein-Protein Interaction Studies of Brain and Muscle Types of Creatine Kinases
SAGE-Hindawi Access to Research Enzyme Research Volume 2011, Article ID 328249, 12 pages doi:10.4061/2011/328249 Research Article Computational Simulations to Predict Creatine Kinase-Associated Factors: Protein-Protein Interaction Studies of Brain and Muscle Types of Creatine Kinases Wei-Jiang Hu,1 Sheng-Mei Zhou,2 Joshua SungWoo Yang,3, 4 and Fan-Guo Meng1 1 Zhejiang Provincial Key Laboratory of Applied Enzymology, Yangtze Delta Region Institute of Tsinghua University, Jiaxing 314006, China 2 College of Biology and Chemical Engineering, Jiaxing University, Jiaxing 314001, China 3 Korean Bioinformation Center (KOBIC), Korea Research Institute of Bioscience & Biotechnology (KRIBB), Daejeon 305-806, Republic of Korea 4 Department of Bioinformatics, University of Sciences & Technology, Daejeon 205-305, Republic of Korea Correspondence should be addressed to Fan-Guo Meng, [email protected] Received 17 May 2011; Accepted 26 May 2011 Academic Editor: Jun-Mo Yang Copyright © 2011 Wei-Jiang Hu et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Creatine kinase (CK; EC 2.7.3.2) is related to several skin diseases such as psoriasis and dermatomyositis. CK is important in skin energy homeostasis because it catalyzes the reversible transfer of a phosphoryl group from MgATP to creatine. In this study, we predicted CK binding proteins via the use of bioinformatic tools such as protein-protein interaction (PPI) mappings and suggest the putative hub proteins for CK interactions. We obtained 123 proteins for brain type CK and 85 proteins for muscle type CK in the interaction networks. -

High Levels of Brain-Type Creatine Kinase Activity in Human Platelets and Leukocytes: a Genetic Anomaly with Autosomal Dominant Inheritance
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by MPG.PuRe Blood Cells, Molecules, and Diseases 48 (2012) 62–67 Contents lists available at SciVerse ScienceDirect Blood Cells, Molecules, and Diseases journal homepage: www.elsevier.com/locate/ybcmd High levels of brain-type creatine kinase activity in human platelets and leukocytes: A genetic anomaly with autosomal dominant inheritance Heidwolf Arnold a, Thomas F. Wienker b, Michael M. Hoffmann c, Günter Scheuerbrandt d, Katharina Kemp e, Peter Bugert e,⁎ a University of Freiburg, Freiburg, Germany b Institute for Medical Biometry, Informatics and Epidemiology, University of Bonn, Bonn, Germany c University Medical Center, Division of Clinical Chemistry, Department of Medicine, Freiburg, Germany d CK-Testlaboratory, Breitnau, Germany e Institute of Transfusion Medicine and Immunology, Medical Faculty Mannheim, Heidelberg University, German Red Cross Blood Service of Baden-Württemberg-Hessen, Mannheim, Germany article info abstract Article history: The ectopic expression in peripheral blood cells of the brain-type creatine kinase (CKB) is an autosomal domi- Submitted 13 October 2011 nant inherited anomaly named CKBE (MIM ID 123270). Here, we characterized the CK activity in serum, platelets Revised 18 October 2011 (PLT) and leukocytes (WBC) of 22 probands (from 8 unrelated families) and 10 controls. CK activity was mea- Available online 16 November 2011 sured by standard UV-photometry. Expression of the CKB gene was analyzed by real-time PCR and Western blot- ting. DNA sequencing including bisulfite treatment was used for molecular analysis of the CKB gene. Serum CK (Communicated by M. Lichtman, M.D., fi 18 October 2011) levels were comparable between probands and controls. -

GSTCD and INTS12 Regulation and Expression in the Human Lung
GSTCD and INTS12 Regulation and Expression in the Human Lung Ma’en Obeidat1,4☯, Suzanne Miller1☯, Kelly Probert1, Charlotte K. Billington1, Amanda P. Henry1, Emily Hodge1, Carl P. Nelson1, Ceri E. Stewart1, Caroline Swan1, Louise V. Wain2, María Soler Artigas2, Erik Melén3, Kevin Ushey4, Ke Hao5, Maxime Lamontagne7, Yohan Bossé6,7, Dirkje S. Postma8, Martin D. Tobin2,9, Ian Sayers1, Ian P. Hall1* 1 Division of Respiratory Medicine, University of Nottingham, Queen’s Medical Center, Nottingham, United Kingdom, 2 Genetic Epidemiology Group, Department of Health Sciences, University of Leicester, Leicester, United Kingdom, 3 Institute of Environmental Medicine, Karolinska Institutet and Sachs’ Children’s Hospital, Stockholm, Sweden, 4 James Hogg Research Centre, Institute for Heart and Lung Health, University of British Columbia, Vancouver, British Columbia, Canada, 5 Department of Genetics and Genomic Sciences, Icahn Institute of Genomics and Multiscale Biology, Icahn School of Medicine at Mount Sinai, New York, United States of America, 6 Department of Molecular Medicine, Laval University, Québec City, Canada, 7 Institut Universitaire de Cardiologie et de Pneumologie de Québec, Laval University, Québec City, Canada, 8 Department of Pulmonology, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands, 9 National Institute for Health Research (NIHR) Leicester Respiratory Biomedical Research Unit, Glenfield Hospital, Leicester, United Kingdom Abstract Genome-Wide Association Study (GWAS) meta-analyses have identified a strong association signal for lung function, which maps to a region on 4q24 containing two oppositely transcribed genes: glutathione S-transferase, C- terminal domain containing (GSTCD) and integrator complex subunit 12 (INTS12). Both genes were found to be expressed in a range of human airway cell types. -

Correction of Chromosomal Instability and Sensitivity to Diverse
Proc. Natl. Acad. Sci. USA Vol. 92, pp. 6354-6358, July 1995 Genetics Correction of chromosomal instability and sensitivity to diverse mutagens by a cloned cDNA of the XRCC3 DNA repair gene (irslSF/crosslinking agents/genetic complementation/chromosomal aberrations) ROBERT S. TEBBS*t, YING ZHAOt, JAMES D. TUCKER*, JULIA B. SCHEERER*, MICHAEL J. SICILIANOt, MONA HWANG*, NAN LIU*, RANDY J. LEGERSKIt, AND LARRY H. THOMPSON*§ *Biology and Biotechnology Research Program, Lawrence Livermore National Laboratory, Livermore, CA 94551-0808; and tDepartment of Molecular Genetics, University of Texas Cancer Center, Houston, TX 77030 Communicated by Evelyn Witkin, Princeton, NJ, March 24, 1995 ABSTRACT The mutagen-sensitive CHO line irslSF was thecin (5-fold), and the cross-linking agents mitomycin C (MMC), previously isolated on the basis of hypersensitivity to ionizing cisplatin, nitrogen mustard, and melphalan (all 20- to 60-fold) radiation and was found to be chromosomally unstable as well (refs. 6 and 7 and results presented here). irslSFwas also reported as cross-sensitive to diverse kinds of DNA-damaging agents. to have '50% reduced efficiency of both single-strand break The analysis of somatic cell hybrids formed between irslSF rejoining and repair replication, elevated spontaneous chromo- and human lymphocytes implicated a human gene (defined as somal aberrations (10-24% abnormal cells), hypomutability in XRCC3; x-ray repair cross-complementing), which partially response to x-rays, but a normal baseline for sister chromatid restored mitomycin C resistance to the mutant. A functional exchange (6). We describe here the cloning of a cDNA sequence cDNA that confers mitomycin C resistance was transferred to that corrects x-ray and cross-linking sensitivities, as well as irslSF cells by transforming them with an expression cDNA spontaneous chromosomal aberrations of irslSF, and we have library and obtaining primary and secondary transformants. -

Identification of Type 2 Diabetes Loci in 433,540 East Asian Individuals
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Nature. Manuscript Author Author manuscript; Manuscript Author available in PMC 2020 November 06. Published in final edited form as: Nature. 2020 June ; 582(7811): 240–245. doi:10.1038/s41586-020-2263-3. Identification of type 2 diabetes loci in 433,540 East Asian individuals A full list of authors and affiliations appears at the end of the article. SUMMARY Meta-analyses of genome-wide association studies (GWAS) have identified >240 loci associated with type 2 diabetes (T2D)1,2, however most loci have been identified in analyses of European- ancestry individuals. To examine T2D risk in East Asian individuals, we meta-analyzed GWAS data in 77,418 cases and 356,122 controls. In the main analysis, we identified 301 distinct association signals at 183 loci, and across T2D association models with and without consideration of body mass index and sex, we identified 61 loci newly implicated in T2D predisposition. Common variants associated with T2D in both East Asian and European populations exhibited strongly correlated effect sizes. New associations include signals in/near GDAP1, PTF1A, SIX3, ALDH2, a microRNA cluster, and genes that affect muscle and adipose differentiation3. At another locus, eQTLs at two overlapping T2D signals affect two genes, NKX6-3 and ANK1, in Users may view, print, copy, and download text and data-mine the content in such documents, for the purposes of academic research, subject always to the full Conditions of use:http://www.nature.com/authors/editorial_policies/license.html#terms *CORRESPONDANCE AND REQUESTS: Correspondence and requests for materials should be addressed to Drs.