Looking for New Classes of Bronchodilators
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Identi®Cation and Role of Adenylyl Cyclase in Auxin Signalling in Higher
letters to nature + + + P.P. thank the Academy of Finland and the Deutsche Forschungsgemeinschaft, respectively, for ®nancial CO , 53), 77 (C6H5 , 60), 73 (TMSi , 84); 6-methyl-4-hydroxy-2-pyrone: RRt 0.35, 198 (M+, 18), 183 ([M-Me]+, 16), 170 ([M-CO]+, 54), 155 ([M-CO-Me]+, support. + + Correspondence and requests for materials should be addressed to J.S. (e-mail: [email protected] 15), 139 ([M-Me-CO2] , 10), 127 ([M-Me-2CO] , 13), 99 (12), 84 (13), 73 + + freiburg.de). (TMSi , 100), 43 (CH3CO , 55). The numbers show m/z values, and the key fragments and their relative intensities are indicated in parentheses. Received 4 August; accepted 14 October 1998. erratum 1. Helariutta, Y. et al. Chalcone synthase-like genes active during corolla development are differentially expressed and encode enzymes with different catalytic properties in Gerbera hybrida (Asteraceae). Plant Mol. Biol. 28, 47±60 (1995). 2. Helariutta, Y. et al. Duplication and functional divergence in the chalcone synthase gene family of 8 Asteraceae: evolution with substrate change and catalytic simpli®cation. Proc. Natl Acad. Sci. USA 93, Crystal structure of the complex 9033±9038 (1996). 3. Thaisrivongs, S. et al. Structure-based design of HIV protease inhibitors: 5,6-dihydro-4-hydroxy-2- of the cyclin D-dependent pyrones as effective, nonpeptidic inhibitors. J. Med. Chem. 39, 4630±4642 (1996). 4. Hagen, S. E. et al. Synthesis of 5,6-dihydro-4-hydroxy-2-pyrones as HIV-1 protease inhibitors: the kinase Cdk6 bound to the profound effect of polarity on antiviral activity. J. Med. Chem. -

Two Phase 3 Clinical Trials Comparing the Safety and Efficacy of Netarsudil to Timolol in Patients with Elevated Intraocular
Two Phase 3 Clinical Trials Comparing the Safety and Efficacy of Netarsudil to Timolol in Patients With Elevated Intraocular Pressure: Rho Kinase Elevated IOP Treatment Trial 1 and 2 (ROCKET-1 and ROCKET-2) JANET B. SERLE, L. JAY KATZ, EUGENE MCLAURIN, THERESA HEAH, NANCY RAMIREZ-DAVIS, DALE W. USNER, GARY D. NOVACK, AND CASEY C. KOPCZYNSKI, FOR THE ROCKET-1 AND ROCKET-2 STUDY GROUPS PURPOSE: To evaluate the efficacy and ocular and sys- ROCKET-2) for timolol (P < .0001 for netarsudil vs temic safety of netarsudil 0.02% ophthalmic solution, a timolol). rho-kinase inhibitor and norepinephrine transporter in- CONCLUSIONS: In 2 large, randomized, double-masked hibitor, in patients with open-angle glaucoma and ocular trials reported here, once-daily dosing of netarsudil hypertension. 0.02% was found to be effective and well tolerated for DESIGN: Double-masked, randomized noninferiority the treatment of patients with ocular hypertension and clinical trials: Rho Kinase Elevated IOP Treatment Trial open-angle glaucoma. The novel pharmacology and 1 and 2 (ROCKET-1 and ROCKET-2). aqueous humor dynamic effects of this molecule suggest METHODS: After a washout of all pre-study ocular hy- it may be a useful addition to the armamentarium of potensive medications, eligible patients were randomized ocular hypotensive medications. (Am J Ophthalmol to receive netarsudil 0.02% once daily (q.d.), timolol 2018;186:116–127. Ó 2017 The Authors. Published 0.5% twice a day (b.i.d.), and (ROCKET-2 only) netar- by Elsevier Inc. This is an open access article under the sudil 0.02% b.i.d. -
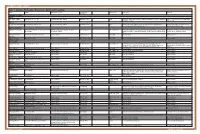
Table 1. Glaucoma Medications: Mechanisms, Dosing and Precautions Brand Generic Mechanism of Action Dosage/Avg
OPTOMETRIC STUDY CENTER Table 1. Glaucoma Medications: Mechanisms, Dosing and Precautions Brand Generic Mechanism of Action Dosage/Avg. % Product Sizes Side Effects Warnings Reduction CHOLINERGIC AGENTS Direct Pilocarpine (generic) Pilocarpine 1%, 2%, 4% Increases trabecular outflow BID-QID/15-25% 15ml Headache, blurred vision, myopia, retinal detachment, bronchiole constriction, Angle closure, shortness of breath, retinal narrowing of angle detachment Indirect Phospholine Iodide (Pfizer) Echothiophate iodide 0.125% Increases trabecular outflow QD-BID/15-25% 5ml Same as above plus cataractogenic iris cysts in children, pupillary block, Same as above, plus avoid prior to any increased paralysis with succinylcholine general anesthetic procedure ALPHA-2 AGONISTS Alphagan P (Allergan) Brimonidine tartrate 0.1%, 0.15% with Purite Decreases aqueous production, increases BID-TID/up to 26% 5ml, 10ml, 15ml Dry mouth, hypotension, bradycardia, follicular conjunctivitis, ocular irritation, Monitor for shortness of breath, dizziness, preservative uveoscleral outflow pruritus, dermatitis, conjunctival blanching, eyelid retraction, mydriasis, drug ocular redness and itching, fatigue allergy Brimonidine tartrate Brimonidine tartrate 0.15%, 0.2% Same as above Same as above 5ml, 10ml Same as above Same as above (generic) Iopidine (Novartis) Apraclonidine 0.5% Decreases aqueous production BID-TID/up to 25% 5ml, 10ml Same as above but higher drug allergy (40%) Same as above BETA-BLOCKERS Non-selective Betagan (Allergan) Levobunolol 0.25%, 0.5% Decreases -
Rhopressa™ Netarsudil Ophthalmic Solution 0.02%
Rhopressa™ Netarsudil ophthalmic solution 0.02% CDER Dermatologic and Ophthalmic Drugs Advisory Committee October 13, 2017 Aerie Pharmaceuticals, Inc. 1 Introduction Marvin Garrett Vice President, Regulatory Affairs and Quality Assurance Aerie Pharmaceuticals, Inc. 2 Aerie Pharmaceuticals • 2005: Aerie founded as a spin-out from Duke University: – Dr. Eric Toone – Dr. Casey Kopczynski – Dr. David Epstein – Dr. Epstein’s goal from the beginning: Develop a therapy that targeted the diseased tissue in glaucoma, the trabecular outflow pathway • 2006: Aerie discovered its first Rho kinase inhibitor • 2009: Aerie invented netarsudil • 2012: Netarsudil 1st clinical study • 2017: NDA filed 3 Netarsudil: A New Drug Class for Lowering IOP We are requesting a recommendation for approval of netarsudil ophthalmic solution 0.02% for reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension given one drop QD 4 Agenda Unmet Medical Needs Richard A. Lewis, MD Chief Medical Officer Aerie Pharmaceuticals, Inc. Past President, American Glaucoma Society Program Design and Efficacy Casey Kopczynski, PhD Chief Scientific Officer Aerie Pharmaceuticals, Inc. Safety Theresa Heah, MD, MBA VP Clinical Research and Medical Affairs Aerie Pharmaceuticals, Inc. Benefits and Risks Janet Serle, MD Professor of Ophthalmology Glaucoma Fellowship Director Icahn School of Medicine at Mount Sinai 5 List of Expert Responders • Cynthia Mattox, MD – Associate Professor of Ophthalmology, Tufts University School of Medicine – Current President, American Glaucoma Society • Mark Reasor, PhD – Professor of Physiology & Pharmacology, Robert C. Byrd Health Sciences Center, West Virginia University • Bennie H. Jeng, MD – Professor and Chair, Department of Ophthalmology & Visual Sciences, University of Maryland School of Medicine • Dale Usner, PhD – Biostatistics Consultant to Aerie Pharmaceuticals, Inc. -

Soluble Guanylate Cyclase and Cgmp-Dependent Protein Kinase I Expression in the Human Corpus Cavernosum
International Journal of Impotence Research (2000) 12, 157±164 ß 2000 Macmillan Publishers Ltd All rights reserved 0955-9930/00 $15.00 www.nature.com/ijir Soluble guanylate cyclase and cGMP-dependent protein kinase I expression in the human corpus cavernosum T Klotz1*, W Bloch2, J Zimmermann1, P Ruth3, U Engelmann1 and K Addicks2 1Department of Urology, University of Cologne; 2Institute I of Anatomy, University of Cologne; and 3Institute of Pharmacology, TU University of Munich, Germany Nitric oxide (NO) as a mediator in smooth muscle cells causes rapid and robust increases in cGMP levels. The cGMP-dependent protein kinase I has emerged as an important signal transduction mediator for smooth muscle relaxation. The purpose of this study was to examine the existence and distribution of two key enzymes of the NO=cGMP pathway, the cGMP-dependent kinase I (cGK I) and the soluble guanylate cyclase (sGC) in human cavernosal tissue. The expression of the enzymes were examined in corpus cavernosum specimens of 23 patients. Eleven potent patients suffered from penile deviations and were treated via Nesbit's surgical method. Nine long-term impotent patients underwent implantation of ¯exible hydraulic prothesis. Three potent patients underwent trans-sexual operations. Expression of the sGC and cGK I were examined immunohistochemically using speci®c antibodies. In all specimens of cavernosal tissue a distinct immunoreactivity was observed in different parts and structures. We found a high expression of sGC and cGK I in smooth muscle cells of vessels and in the ®bromuscular stroma. The endothelium of the cavernosal sinus, of the cavernosal arteries, and the cavernosal nerve ®bers showed an immunoreactivity against sGC. -

Soluble Guanylate Cyclase B1-Subunit Expression Is Increased in Mononuclear Cells from Patients with Erectile Dysfunction
International Journal of Impotence Research (2006) 18, 432–437 & 2006 Nature Publishing Group All rights reserved 0955-9930/06 $30.00 www.nature.com/ijir ORIGINAL ARTICLE Soluble guanylate cyclase b1-subunit expression is increased in mononuclear cells from patients with erectile dysfunction PJ Mateos-Ca´ceres1, J Garcia-Cardoso2, L Lapuente1, JJ Zamorano-Leo´n1, D Sacrista´n1, TP de Prada1, J Calahorra2, C Macaya1, R Vela-Navarrete2 and AJ Lo´pez-Farre´1 1Cardiovascular Research Unit, Cardiovascular Institute, Hospital Clı´nico San Carlos, Madrid, Spain and 2Urology Department, Fundacio´n Jime´nez Diaz, Madrid, Spain The aim was to determine in circulating mononuclear cells from patients with erectile dysfunction (ED), the level of expression of endothelial nitric oxide synthase (eNOS), soluble guanylate cyclase (sGC) b1-subunit and phosphodiesterase type-V (PDE-V). Peripheral mononuclear cells from nine patients with ED of vascular origin and nine patients with ED of neurological origin were obtained. Fourteen age-matched volunteers with normal erectile function were used as control. Reduction in eNOS protein was observed in the mononuclear cells from patients with ED of vascular origin but not in those from neurological origin. Although sGC b1-subunit expression was increased in mononuclear cells from patients with ED, the sGC activity was reduced. However, only the patients with ED of vascular origin showed an increased expression of PDE-V. This work shows for the first time that, independently of the aetiology of ED, the expression of sGC b1-subunit was increased in circulating mononuclear cells; however, the expression of both eNOS and PDE-V was only modified in the circulating mononuclear cells from patients with ED of vascular origin. -

Human Erythrocyte Acetylcholinesterase in Health and Disease
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Universidade de Lisboa: Repositório.UL molecules Review Human Erythrocyte Acetylcholinesterase in Health and Disease Carlota Saldanha Instituto de Bioquímica, Instituto de Medicina Molecular, Faculdade de Medicina, Universidade de Lisboa, Av. Professor Egas Moniz, 1649-028 Lisboa, Portugal; [email protected] Received: 10 August 2017; Accepted: 4 September 2017; Published: 8 September 2017 Abstract: The biochemical properties of erythrocyte or human red blood cell (RBC) membrane acetylcholinesterase (AChE) and its applications on laboratory class and on research are reviewed. Evidence of the biochemical and the pathophysiological properties like the association between the RBC AChE enzyme activity and the clinical and biophysical parameters implicated in several diseases are overviewed, and the achievement of RBC AChE as a biomarker and as a prognostic factor are presented. Beyond its function as an enzyme, a special focus is highlighted in this review for a new function of the RBC AChE, namely a component of the signal transduction pathway of nitric oxide. Keywords: acetylcholinesterase; red blood cells; nitric oxide 1. Introduction Erythrocytes or red blood cells (RBC) are more than sacks of oxyhemoglobin or deoxyhemoglobin during the semi-life of 120 days in blood circulation [1]. Erythrocytes comport different signaling pathways which includes the final stage of apoptosis, also called eryptosis [2,3]. Exovesicules enriched with acetylcholinesterase (AChE) originated from membranes of aged erythrocytes appear in plasma [4]. Kinetic changes of the AChE enzyme have been observed in old erythrocytes [5]. Previously, AChE in erythrocytes was evidenced as a biomarker of membrane integrity [6]. -

Nitric Oxide Activates Guanylate Cyclase and Increases Guanosine 3':5'
Proc. Natl. Acad. Sci. USA Vol. 74, No. 8, pp. 3203-3207, August 1977 Biochemistry Nitric oxide activates guanylate cyclase and increases guanosine 3':5'-cyclic monophosphate levels in various tissue preparations (nitro compounds/adenosine 3':5'-cyclic monophosphate/sodium nitroprusside/sodium azide/nitrogen oxides) WILLIAM P. ARNOLD, CHANDRA K. MITTAL, SHOJI KATSUKI, AND FERID MURAD Division of Clinical Pharmacology, Departments of Medicine, Pharmacology, and Anesthesiology, University of Virginia, Charlottesville, Virginia 22903 Communicated by Alfred Gilman, May 16, 1977 ABSTRACT Nitric oxide gas (NO) increased guanylate cy- tigation of this activation. NO activated all crude and partially clase [GTP pyrophosphate-yase (cyclizing), EC 4.6.1.21 activity purified guanylate cyclase preparations examined. It also in- in soluble and particulate preparations from various tissues. The effect was dose-dependent and was observed with all tissue creased cyclic GMP but not adenosine 3':5'-cyclic monophos- preparations examined. The extent of activation was variable phate (cyclic AMP) levels in incubations of minces from various among different tissue preparations and was greatest (19- to rat tissues. 33-fold) with supernatant fractions of homogenates from liver, lung, tracheal smooth muscle, heart, kidney, cerebral cortex, and MATERIALS AND METHODS cerebellum. Smaller effects (5- to 14-fold) were observed with supernatant fractions from skeletal muscle, spleen, intestinal Male Sprague-Dawley rats weighing 150-250 g were decapi- muscle, adrenal, and epididymal fat. Activation was also ob- tated. Tissues were rapidly removed, placed in cold 0.-25 M served with partially purified preparations of guanylate cyclase. sucrose/10 mM Tris-HCl buffer (pH 7.6), and homogenized Activation of rat liver supernatant preparations was augmented in nine volumes of this solution by using a glass homogenizer slightly with reducing agents, decreased with some oxidizing and Teflon pestle at 2-4°. -

Cyclic Nucleotide Phosphodiesterases in Heart and Vessels
Cyclic nucleotide phosphodiesterases in heart and vessels: A therapeutic perspective Pierre Bobin, Milia Belacel-Ouari, Ibrahim Bedioune, Liang Zhang, Jérôme Leroy, Véronique Leblais, Rodolphe Fischmeister, Grégoire Vandecasteele To cite this version: Pierre Bobin, Milia Belacel-Ouari, Ibrahim Bedioune, Liang Zhang, Jérôme Leroy, et al.. Cyclic nucleotide phosphodiesterases in heart and vessels: A therapeutic perspective. Archives of cardiovascular diseases, Elsevier/French Society of Cardiology, 2016, 109 (6-7), pp.431-443. 10.1016/j.acvd.2016.02.004. hal-02482730 HAL Id: hal-02482730 https://hal.archives-ouvertes.fr/hal-02482730 Submitted on 23 Mar 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Cyclic nucleotide phosphodiesterases in heart and vessels: A therapeutic perspective Abbreviated title: Cyclic nucleotide phosphodiesterases in heart and vessels French title: Phosphodiestérases des nucléotides cycliques dans le cœur et les vaisseaux : une perspective thérapeutique. Pierre Bobin, Milia Belacel-Ouari, Ibrahim Bedioune, Liang Zhang, Jérôme Leroy, Véronique Leblais, Rodolphe Fischmeister*, Grégoire Vandecasteele* UMR-S 1180, INSERM, Université Paris-Sud, Université Paris-Saclay, Châtenay-Malabry, France * Corresponding authors. UMR-S1180, Faculté de Pharmacie, Université Paris-Sud, 5 rue J.-B. Clément, F-92296 Châtenay-Malabry Cedex, France. -

Interaction of Phosphodiesterase 3A with Brefeldin A-Inhibited Guanine Nucleotide-Exchange Proteins BIG1 and BIG2 and Effect on ARF1 Activity
Interaction of phosphodiesterase 3A with brefeldin A-inhibited guanine nucleotide-exchange proteins BIG1 and BIG2 and effect on ARF1 activity Ermanno Puxeddu, Marina Uhart, Chun-Chun Li, Faiyaz Ahmad, Gustavo Pacheco-Rodriguez, Vincent C. Manganiello, Joel Moss, and Martha Vaughan1 Translational Medicine Branch, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD 20892 Contributed by Martha Vaughan, February 11, 2009 (sent for review September 22, 2008) ADP-ribosylation factors (ARFs) have crucial roles in vesicular (11). Two-hybrid interaction of the BIG2 N-terminal region with trafficking. Brefeldin A-inhibited guanine nucleotide-exchange exocyst subunit Exo70 was confirmed by coimmunoprecipitation proteins (BIG)1 and BIG2 catalyze the activation of class I ARFs by (co-IP) of the in vitro-translated proteins; microscopically, the accelerating replacement of bound GDP with GTP. Several addi- endogenous proteins appeared together along microtubules tional and differing actions of BIG1 and BIG2 have been described. (12);3Akinase-anchoring protein (AKAP) sequences in the These include the presence in BIG2 of 3 A kinase-anchoring protein N-terminal region of BIG2, one of which is identical in BIG1, (AKAP) domains, one of which is identical in BIG1. Proteins that were identified in yeast 2-hybrid experiments with 4 different A contain AKAP sequences act as scaffolds for the assembly of PKA kinase R subunits and multiple peptide sequences representing with other enzymes, substrates, and regulators in complexes that positions 1 to 643 of BIG2 (13). Consistent with the presence of constitute molecular machines for the reception, transduction, and AKAP sequences for each of the 4 R subunits in BIG1 and BIG2, integration of signals from cAMP or other sources, which are both proteins were coimmunoprecipitated from HepG2 cell initiated, propagated, and transmitted by chemical, electrical, or cytosol with antibodies against RI or RII, although direct mechanical means. -

Modulation of Food Intake by Differential TAS2R Stimulation In
nutrients Article Modulation of Food Intake by Differential TAS2R Stimulation in Rat Carme Grau-Bové 1, Alba Miguéns-Gómez 1 , Carlos González-Quilen 1 , José-Antonio Fernández-López 2,3 , Xavier Remesar 2,3 , Cristina Torres-Fuentes 4 , Javier Ávila-Román 4 , Esther Rodríguez-Gallego 1, Raúl Beltrán-Debón 1 , M Teresa Blay 1 , Ximena Terra 1 , Anna Ardévol 1,* and Montserrat Pinent 1 1 MoBioFood Research Group, Department of Biochemistry and Biotechnology, Universitat Rovira i Virgili, 43007 Tarragona, Spain; [email protected] (C.G.-B.); [email protected] (A.M.-G.); [email protected] (C.G.-Q.); [email protected] (E.R.-G.); [email protected] (R.B.-D.); [email protected] (M.T.B.); [email protected] (X.T.); [email protected] (M.P.) 2 Department of Biochemistry and Molecular Biomedicine, Faculty of Biology, University of Barcelona, Av. Diagonal 643, 08028 Barcelona, Spain; [email protected] (J.-A.F.-L.); [email protected] (X.R.) 3 CIBER Obesity and Nutrition, Institute of Health Carlos III, Av. Diagonal 643, 08028 Barcelona, Spain 4 Nutrigenomics Research Group, Department of Biochemistry and Biotechnology, Universitat Rovira i Virgili, 43007 Tarragona, Spain; [email protected] (C.T.-F.); [email protected] (J.Á.-R.) * Correspondence: [email protected]; Tel.: +34-977-559-566 Received: 31 October 2020; Accepted: 4 December 2020; Published: 10 December 2020 Abstract: Metabolic surgery modulates the enterohormone profile, which leads, among other effects, to changes in food intake. Bitter taste receptors (TAS2Rs) have been identified in the gastrointestinal tract and specific stimulation of these has been linked to the control of ghrelin secretion. -

G Protein-Coupled Receptors
S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2015/16: G protein-coupled receptors. British Journal of Pharmacology (2015) 172, 5744–5869 THE CONCISE GUIDE TO PHARMACOLOGY 2015/16: G protein-coupled receptors Stephen PH Alexander1, Anthony P Davenport2, Eamonn Kelly3, Neil Marrion3, John A Peters4, Helen E Benson5, Elena Faccenda5, Adam J Pawson5, Joanna L Sharman5, Christopher Southan5, Jamie A Davies5 and CGTP Collaborators 1School of Biomedical Sciences, University of Nottingham Medical School, Nottingham, NG7 2UH, UK, 2Clinical Pharmacology Unit, University of Cambridge, Cambridge, CB2 0QQ, UK, 3School of Physiology and Pharmacology, University of Bristol, Bristol, BS8 1TD, UK, 4Neuroscience Division, Medical Education Institute, Ninewells Hospital and Medical School, University of Dundee, Dundee, DD1 9SY, UK, 5Centre for Integrative Physiology, University of Edinburgh, Edinburgh, EH8 9XD, UK Abstract The Concise Guide to PHARMACOLOGY 2015/16 provides concise overviews of the key properties of over 1750 human drug targets with their pharmacology, plus links to an open access knowledgebase of drug targets and their ligands (www.guidetopharmacology.org), which provides more detailed views of target and ligand properties. The full contents can be found at http://onlinelibrary.wiley.com/doi/ 10.1111/bph.13348/full. G protein-coupled receptors are one of the eight major pharmacological targets into which the Guide is divided, with the others being: ligand-gated ion channels, voltage-gated ion channels, other ion channels, nuclear hormone receptors, catalytic receptors, enzymes and transporters. These are presented with nomenclature guidance and summary information on the best available pharmacological tools, alongside key references and suggestions for further reading.