Prevalence and Antibiotic Resistance of Salmonella Spp. in South Punjab
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Production and Marketing of Camel Products in Semi-Desert and Desert Areas of Pakistan
Pakistan J. Agric. Res. Vol. 26 No. 2, 2013 PRODUCTION AND MARKETING OF CAMEL PRODUCTS IN SEMI- DESERT AND DESERT AREAS OF PAKISTAN Abid Hussain*, Khalid Mahmood Aujla* and Sonila Hassan** Abstract:- The study was designed to analyze the production and marketing of camel products in the semi-desert and desert areas of Pakistan. It is based on cross-sectional data collected through simple random sampling technique in April, 2011 from 220 camel farmers and 17 market intermediaries. It is found that both camel farmers and market intermediaries were less educated. It is observed that markets for camel milk, meat, hides and hair are less established in semi desert and desert areas of the country. Mean production of milk per farm household was 5.4 and 6.5 liters per day in summer and winter seasons, respectively; however, none of the surveyed farmers reported milk sale. During last one year, sales of camel hides and hair were reported by few farmers (6% each). Mean purchase price of camel hides reported by shopkeepers in nearby town markets were higher than village level prices by 74.6 % and even more in case of hair. This is an indicative of camel farmers' exploitation by the village dealers. Mean quantity of hair sales was about 20 kg per farm per annum. Camel hair are also used by the farmers for making ropes, rugs and blankets, but all these byproducts are not marketed. Shares of farmers in the consumer rupee for camel meat, milk, hides and hair were about 61%, 75%, 52% and 26%, respectively. -

Pakistan Provinces and Divisions Northerna Areas
PAKISTAN PROVINCES AND DIVISION C H I N A NORTHERrN4CHINA AREAS IA MM U KA; I I I I i 5 p,.,,., * ISLAMABAD If HHITO)lf . ^:,K,°/ • "' -. PUNJAB / 1, sK / "( i!ALUCHISTAN I RAN b SIND AR A B I A N SEA ,. ".. ri) o NATIONAL NUTRITION SURVEY 1985 - 87 REPORT NUTRITION DIVISION NATIONAL INSTITUTE OF HEALTH GOVERNMENT OF PAKISTAN 1988 REPORT OF THE NATIONAL NUTRITION SURVEY 1985-87, PAKISTAN TABLE OF CONTENTS 'FOREWORD ............................................ (i) PREFACE ............................................. (lii) ACKNOWLEDEGEMENT .................................... (iv) 1. EXECUTIVE SUMMARY ................................... (vi) 1.1 SUMMARY OF FINDINGS ............................ (viii) 2. INTRODUCTION 2.1 GENERAL INFORMATION .............................. .. 2.1.1. Geographical 2.1.2. Literacy 2.1.3. Agriculture 2.1.4. Trends In Agricultural Production 2.1.5. Health 2.1.6. Primary Health Care 2.2. NUTRITIONAL STATUS .............................. 6 2.2.1 General 2.2.2. Malnutrition in Children 2.2.3. Breast Feeding 2.2.4. Bottle Feeding 3. THE NATIONAL NUTRITION SURVEY 1985/87 3.1 BACKGROUND ..................................... 8 3.2 GOALS AND OBJECTIVES ................ ;.......... 8 3.3 SAMPLING ....................................... 9 3.3.1 Universe 3.3.2 Stratification Plan 3.3.3 Sampling Frame 3.3.4 Sample Design 3.3.5 Sample Size and its Allocation 3.4 WEIGHTING ....................... .............. 11 2.5 METHODOLOGY .................................... 13 3.r.1 Household Survey 3.5.2 Dietary Survey 3.5.3 Clinical Survey 3.5.4 Anthropometric Examination 3.5.5 Biochemical Survey 3.6 CLASSIFICATION OF NUTRITIONAL STATUS ............ 15 4. RESULTS 4.1. CHILDREN UNDER 5 4.1.1 Anthropometry of Children under 5 ...... 19 4.1.2 Age & Sex Distribution .................. 20 .... -

The Spectrum of Beta-Thalassemia Mutations in Couples Referred for Chorionic Villus Sampling at Bahawal Victoria Hospital, Bahawalpur
Open Access Original Article DOI: 10.7759/cureus.3265 The Spectrum of Beta-thalassemia Mutations in Couples Referred for Chorionic Villus Sampling at Bahawal Victoria Hospital, Bahawalpur Uffan Zafar 1 , Kamran Naseem 2 , Muhammad Usman Baig 3 , Zain Ali Khan 4 , Fariha Zafar 5 , Saba Akram 6 1. Radiology Department, Bahawal Victoria Hospital, Quaid-E-Azam Medical College, Bahawalpur, PAK 2. Radiology Department, Bahawal Victoria Hospital, Quaid-E-Azam Medical College, Bahawalpur , PAK 3. Medicine, Bahawal Victoria Hospital, Bahawalpur, PAK 4. Gastroenterology, Pakistan Kidney and Liver Institute and Research Centre, Okara, PAK 5. Community Medicine, Quaid E Azam Medical College, Bahawalpur, PAK 6. Medical Ward, Bahawal Victoria Hospital, Quaid-E-Azam Medical College, Bahawalpur, PAK Corresponding author: Uffan Zafar, [email protected] Abstract Introduction The prevalence of beta-thalassemia mutations is different in various castes, regions, and ethnic groups. By knowing this prevalence, we can conduct a targeted screening of only the high-risk population and only for the specific mutations that are prevalent in each group. Objective The purpose of this study was to determine the regional, caste-wise, and ethnic spectrum of beta- thalassemia mutations in couples referred for a prenatal diagnosis. Methods A cross-sectional analytical study was conducted at the thalassemia unit, Bahawal Victoria Hospital, Bahawalpur, from October 1, 2015, to May 15, 2018. After obtaining informed consent, chorionic villus sampling (CVS) was performed in 144 women having a gestational age of 12 to 16 weeks. We took blood samples of the couples. A chromosomal analysis for 13 mutations was done at Punjab Thalassaemia Prevention Programme (PTPP), Lahore. -

Situation Analysis of Reproductive Health of Adolescents and Youth in Pakistan
1 Situation Analysis of Reproductive Health of Adolescents and Youth in Pakistan December 2019 i The Population Council confronts critical health and development issues—from stopping the spread of HIV to improving reproductive health and ensuring that young people lead full and productive lives. Through biomedical, social science, and public health research in 50 countries, we work with our partners to deliver solutions that lead to more effective policies, programs, and technologies that improve lives around the world. Established in 1952 and headquartered in New York, the Council is a nongovernmental, nonprofit organization governed by an international board of trustees. Population Council 3rd Floor, NTC Building (North), Sector F-5/1 Islamabad, Pakistan Tel: +92 51 920 5566 Fax: +92 51 282 1401 Email: [email protected] http://www.popcouncil.org ii Table of Contents ACKNOWLEDGEMENTS ............................................................................................................................. VII ACRONYMS ............................................................................................................................................... VIII EXECUTIVE SUMMARY ................................................................................................................................ IX CHAPTER- 1 INTRODUCTION AND METHODOLOGY .................................................................................... 1 Background ................................................................................................................................................... -

MONSOON UPDATE Pakistan
MONSOON UPDATE Pakistan Issue 2 | 28 July - 2 August 2013 This report identifies the current trends, events, and short-term forecast associated with the 2013 monsoon season. OVERVIEW • Weather forecasts indicate a countrywide monsoon spell over the next week with potential heavy impacts between 1 and 4 August. There is a need to monitor the flood impact situation in regions traditionally prone to flash and riverine floods. • The Pakistan Metrological Department has issued flash flood warnings for rain affected areas of Balochistan and Dera Ghazi Khan Division in Punjab. Water channels in the catchments of rivers Chenab and Ravi in Punjab and Kabul in Khyber Pakhtunkhwa (KP) may attain medium to high flood levels. • The Space and Upper Atmospher e Research Commission (SUPARCO) indicates the snow cover in 2013 is higher compared with 2008 to 2012, with a corresponding impact on snowmelt. Higher temperatures could cause a rise in river flows. • Water reservoirs continue to fill up comparatively earlier than in previous years, thereby limiting flood impact mitigation options. • Rivers Indus, Chenab, Kabul and Swat are flowing at higher than normal flood levels. MONSOON EVENTS AND IMPACT summer months should be seen in the wider context of snowmelt Rainfall: Last week was characterized by hot and humid and precipitation. Experts estimate 10 per cent of the average conditions with scattered rains. The Pakistan Meteorological runoff is caused by rainfall along the Indus plains. Department (PMD) issued a flash warning for north-eastern River floods: Rivers Indus, Chenab, Kabul and Swat are in Punjab along rivers Chenab and Ravi catchments. low flood. -

4 Chronology of Disaster in Pakistan 2012 (25Th August-15Th October)
Strengthening Participatory Organization (SPO) SPO is one of the largest rights-based civil society organization in Pakistan. It is pursuing various program components presently being implemented in over 75 districts of the country. SPO seeks to address mainly governance, social and political issues in the country through its programmes focussing on democratic th governance, social justice, peace and harmony, institutional strengthening, conflict resolution, citizens engagement, gender, electoral reforms and political parties development. Parallel to these activities, SPO deals with humanitarian 15August - October) emergencies resulting from both natural and human-induced hazards. In th emergencies, it has been dealing to redress problems of disaster like (25 earthquakes, rain-fed floods, cyclones and rehabilitation of internally displaced communities affected by conflicts. Chronology of Disaster in Pakistan 2012 Protection and promotion of human rights is central to the program philosophy of SPO. Its various citizens voices and accountability initiatives seek to strengthen democratic processes through engagement with and building capacities of civil society and state institutions and harness mutual tolerance, peace and harmony between various political, ethnic and religious groups across rural and urban parts of the country. Various components of SPO's citizens voices and accountability initiatives are currently supported by Australian Agency for International Development (AusAid), British High Commission (BHC), Embassy for the Kingdom of Netherlands (EKN), DFID and USAID. SPO also acknowledges support from other donors for its various program components SPO National Center 30-A, Nazimuddin Road, F-10/4, Islamabad, Pakistan UAN: +92-51-111-357-111 Tel: +92-51-2104677, 2104679 Fax: +92-51-2112787 [email protected] www.spopk.org BALOCHISTAN KHYBER PAKHTUNKHWA PUNJAB SINDH AZAD JAMMU KASHMIR QUETTA PESHAWAR MULTAN HYDERABAD MUZAFFARABAD House 58-A, Near Pak Japan House 15, Street 1, Sector N-4 House 339-340, Block-D Plot 158/2, Behind M. -
Dera-Ghazi-Khan.Pdf
District Dera Ghazi Khan Human Development Report District Dera Ghazi Khan Human Development Report Addressing Vulnerabilities in Education and Health: Responding to Out-of-School Children and Out-of-Pocket Costs Faisal Buzdar AAWAZ Copyrights AAWAZ Programme @2015 AAWAZ Programme is funded by the UKAid through the Department for International Development (DFID), AAWAZ was conceived initially as a five-year programme, from 2012 to 2017. Development Alternatives Inc. (DAI) is the Management Organisation (MO) for implementing the AAWAZ programme, while Pakistan’s prime civil society organisations: Aurat Foundation (AF), South-Asia Partnership Pakistan (SAP-PK), Strengthening Participatory Organisation (SPO) and Sungi Development Foundation (SF) form the implementation consortium responsible for directly working with communities. All publications by AAWAZ are copyrighted, however, can be cited with reference. 2 District Dera Ghazi Khan Human Development Report Table of Contents Executive Summary ....................................................................................................................... 5 Chapter 1: Putting Human Development and Human Development Reports into Perspective ....... 7 1.1: Enlarging Choices: The Case for Human Development ....................................................... 7 1.2: Human Development Reports: An Overview ..................................................................... 8 1.3: Key Indicators .................................................................................................................. -
Form E SESE (Math)
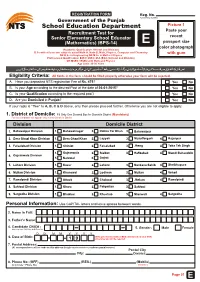
REGISTRATION FORM Reg. No. Government of the Punjab To be Filled by NTS NTS School Education Department Picture 1 Paste your Recruitment Test for Senior Elementary School Educator recent (Mathematics) (BPS-14) E passport size color photograph (Academic Qualification: At least 2nd Division) B.Sc with at least two subjects out of Math-A, Math-B, Math, Physics, Computer and Chemistry with gum OR B.Sc in Engineering OR M.Sc in Math or Physics Professional Qualification: B.Ed / M.Ed / M.A (Edu) (At least 2nd Division) OR MSED / BSED with Math and Physics Age Limit: 20-30 Years Eligibility Criteria: All fields in the form should be filled properly otherwise your form will be rejected. A. Have you deposited NTS registration Fee of Rs. 475? Yes No B. Is your Age according to the desired Post at the date of 26-01-2015? Yes No C. Is your Qualification according to the required post? Yes No D. Are you Domiciled in Punjab? Yes No If your reply is “Yes” to A, B, C & D above, only then please proceed further. Otherwise you are not eligible to apply. 1. District of Domicile: Fill Only One Desired Box for Domicile District (Mandatory) For test candidate will appear only in their Domicile District. Division Domicile District 1. Bahawalpur Division 1. Bahawalnagar 2. Rahim Yar Khan 3. Bahawalpur 2. Dera Ghazi Khan Division 1. Dera Ghazi Khan 2. Layyah 3. Muzaffargarh 4. Rajanpur 3. Faisalabad Division 1. Chiniot 2. Faisalabad 3. Jhang 4. Toba Tek Singh 1. Gujranwala 2. Sialkot 3. Hafizabad 4. -

Chief Election Commissioner
CHIEF ELECTION COMMISSIONER AZAD JAMMU & KASHMIR ELECTION COMMISSION SECRETARIAT BLOCK NO.6 (LOWER GROUND)NEW SECRETARIAT COMPLEX CHATTER DELIMITATION COMMISSION AZAD JAMMU & KASHMIR MIRPUR DISTRICT S. No. Number and name of Extent of the Constituency Constituency 1. LA-I, MIRPUR – I. The Whole Tehsil of Dadyal 2. LA-II, MIRPUR – II. The following Patwar Circles of Mirpur Tehsil:- 1. Palak 2. Pind Khurd 3. Dheri Phali 4. Dheri Barwan. 5. Chakswari 6. Panyam 7. Boa 8. Tang Dew 9. Kaneli. 10. Mawah 11. Bajjar 12. Herdochi 13. Islam Garh. 14. Kalyal Bainsi 15. Potha Bainsi. 3. LA-III, MIRPUR – III. The following Patwar Circles of Mirpur Tehsil:- 1. Khanpur 2. Kharak 3. Rathoa Muhammad Ali. 4. Thothal 5. Sangot 6. Mirpur Muncipal area. 4. LA-IV, MIRPUR – IV. The following Patwar Circles of Mirpur Tehsil:- 1. Khari Khas 2. Aziz Pur 3. Lehri 4. Sonkia. 5. Bhalyala 6. Khurd 7. Pindi-Suberwal 8. Afzal Pur. 9. Samwal shrif 10. Pulmanda 11. Sahang 12. Bani. 13. Balwara 14. Jatlan 15. Jouian 16. Janian. 17. Pakharal 18. Naugran 19. Dhalmahmood 20. Raipur. BHIMBER DISTRICT 5. LA-V, BHIMBER – I. The Whole Tehsil of Barnala. 6. LA-VI, BHIMBER – II. The Whole Tehsil of Samahni. 7. LA-VII, BHIMBER – III. The Whole Tehsil of Bhimber. KOTLI DISTRICT 8. LA-VIII, KOTLI – I. The following Patwar Circles of Kotli Tehsil:- 1. Kotli Khas 2. Roli 3. Dhanwan 4. Goi 5.Kakanni Baghah. 6. Phagwari 7.Dhamol 8.Gulhar Shrif 9.ChowkiTeenda 10. Jhanjora 11.Dundli. 9. LA-IX, KOTLI – II. (i) The Whole Tehsil of Fatehpur (Nakyal). -

Endangered Species Voice, March 2015
Endangered Species Voice Vol: 11 NO: 111 March 2015 BY: DEVELOPMENT FOUNDATION SANGAT Endangered Species Voice: Sindh-Pakistan Fortnightly Monitoring Bulletin 2015 and were destined for Cheong House, 139-Des Bid to smuggle Voeux, West Hong Kong, China. ‘largest’ turtle parts shipment foiled FAIZA ILYAS — KARACHI: A Hong Kong-bound consignment of over 4,000 dried body parts of freshwater turtles, a protected species in the country, was confiscated last week by the customs authorities at Karachi port, it emerged on Thursday. The dried body parts were identified as those “A thorough examination, however, raised the of Indian narrow-headed softshell turtles, a suspicion that the consignment consisted of critically endangered and protected reptile in turtle meat, bones and skulls. This was verified the country. by the Sindh wildlife department staff that inspected the consignment on our request. “This is the largest seizure involving turtles in the country’s history that might involve “We were told that the consignment contained militant organisations.” dried turtle shells, plastrons, fringes of freshwater turtles that are protected under This information was shared with journalists international and national laws and exist in the at a press conference jointly addressed by a entire Indus river system,” he explained. customs official and a Sindh wildlife conservator at the Pakistan International During the question-answer session, it was Container Terminal on Thursday. pointed out most of these turtles might have been caught at the Taunsa barrage and Kalabagh “The value of a turtle is over Rs150,000 (in areas that had a good population of turtles, the black market). -

Trail of Tragedy 5.Pdf
Trail of Tragedy-5 Chronology of Disaster in Pakistan 2014 Trail of Tragedy - 5 Chronology of Disaster in Pakistan 2014 Contents Acronyms iv Acknowledgment v Background vi News Items 2014 1 Editorials - Articles 99 Strengthening Participatory Organization (SPO) iii Trail of Tragedy - 5 Chronology of Disaster in Pakistan 2014 Acronyms FFC Federal Flood Commission IUCN International Union for Conservation of Nature LBOD Left Bank Outfall Drain MNV Main Nara Valley NADRA National Database and Registration Authority NDMA National Disaster Management Authority NNS National Nutrition Survey PDMA Provincial Disaster Management Authority PMD Pakistan Meteorological Department RBOD-I Right Bank Outfall Drain SIDA Sindh Irrigation and Drainage Authority SUPARCO Pakistan Space and Upper Atmosphere Research Commission UN United Nations UNESCO United Nations Educational, Scientific and Cultural Organization WFP World Food Programme Strengthening Participatory Organization (SPO) iv Trail of Tragedy - 5 Chronology of Disaster in Pakistan 2014 Acknowledgment It is acknowledged that this chronology of disaster related to the floods in Sindh in 2014 has been compiled using the online archives of major national newspapers: Dawn at www.dawn. com, The News at www. thenews.com.pk and Express Tribune. SPO presents this chronology through the courtesy of these two media outlets. However, this data does not represent a hundred percent coverage of the disaster and response that have been reported. Editorials, news items and letters to Editors, included in this chronology are related to heavy Rains, Floods, Human security, Vulnerable Groups, Food Security, Livelihood and Aid & Aid effectiveness. SPO does not take the responsibility either for the authenticity of contents of news stories included in this report, or for the treatment of the flood disaster by the media. -

A Case of Dera Ghazi Khan Duriing Elections 1982-1997 Pjaee, 17 (11) (2020)
ROLE OF ETHNICITY IN ELECTTORAL POLITICS OF PAKISTAN:A CASE OF DERA GHAZI KHAN DURIING ELECTIONS 1982-1997 PJAEE, 17 (11) (2020) ROLE OF ETHNICITY IN ELECTTORAL POLITICS OF PAKISTAN: A CASE OF DERA GHAZI KHAN DURIING ELECTIONS 1982-1997 Sohail Akhtar1 ,Sajid Hussain1 , Rafiq Akbar1 Muhammad Madni Asghar 2 1 Ghazi University, D. G. Khan 2The Islamia University of Bahawalpur. Sohail Akhtar ,Sajid Hussain , Rafiq Akbar, Muhammad Madni Asghar: ROLE OF ETHNICITY IN ELECTTORAL POLITICS OF PAKISTAN: A CASE OF DERA GHAZI KHAN DURIING ELECTIONS 1982-1997-- Palarch’s Journal of Archaeology Of Egypt/Egyptology 17 (11), 116-132. ISSN 1567-214x Keywords: Ethnicity, Politics, Reciprocal, Region, Elections, Dera Ghazi Khan etc. Abstract The last half of the twentieth century is marked by the rise of the concept of ethnicity in the world. The world War-II promoted ethnonational concept of polity and as a result many new ethnic states emerged on the world map by the end of the World War-II. Ethnicity is a major tool of electoral politics in plural societies especially in authoritarian democracy. In Pakistan as other post-colonial states of the world ethnicity is a deep rooted concept and has a strong impact on political development. Intra-ethnic differences lead the ethnic groups towards ethnic politics to get their representation. In modern democratic states ethnic groups try to pressurize the state for representation while state controlled them through forcefully or negotiate with them to establish its writ. The relation between ethnicity and politics is reciprocal. This research paper is an attempt to understand the nature of relationship between ethnicity and political development in Pakistan with a regional case study; Dera Ghazi Khan District is one of the regions of Pakistan, which has multi-ethnic, multi-cultural and multi- lingual formation of society.