Vitex Agnus-Castus Extracts for Female Reproductive Disorders: a Systematic Review of Clinical Trials
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Weed Risk Assessment for Vitex Rotundifolia L. F. (Lamiaceae)
Weed Risk Assessment for Vitex United States rotundifolia L. f. (Lamiaceae) – Beach Department of Agriculture vitex Animal and Plant Health Inspection Service June 4, 2013 Version 2 Left: Infestation in South Carolina growing down to water line and with runners and fruit stripped by major winter storm (Randy Westbrooks, U.S. Geological Survey, Bugwood.org). Right: A runner with flowering shoots (Forest and Kim Starr, Starr Environmental, Bugwood.org). Agency Contact: Plant Epidemiology and Risk Analysis Laboratory Center for Plant Health Science and Technology Plant Protection and Quarantine Animal and Plant Health Inspection Service United States Department of Agriculture 1730 Varsity Drive, Suite 300 Raleigh, NC 27606 Weed Risk Assessment for Vitex rotundifolia Introduction Plant Protection and Quarantine (PPQ) regulates noxious weeds under the authority of the Plant Protection Act (7 U.S.C. § 7701-7786, 2000) and the Federal Seed Act (7 U.S.C. § 1581-1610, 1939). A noxious weed is defined as “any plant or plant product that can directly or indirectly injure or cause damage to crops (including nursery stock or plant products), livestock, poultry, or other interests of agriculture, irrigation, navigation, the natural resources of the United States, the public health, or the environment” (7 U.S.C. § 7701-7786, 2000). We use weed risk assessment (WRA)—specifically, the PPQ WRA model (Koop et al., 2012)—to evaluate the risk potential of plants, including those newly detected in the United States, those proposed for import, and those emerging as weeds elsewhere in the world. Because the PPQ WRA model is geographically and climatically neutral, it can be used to evaluate the baseline invasive/weed potential of any plant species for the entire United States or for any area within it. -

Estrogen-Like Activities in Vitex Species from China Determined by a Cell Based Proliferation Assay
ORIGINAL ARTICLES Department of Pharmacognosy1, School of Pharmacy, Second Military Medical University, Shanghai, China; School of Biomo- lecular Science2, Faculty of Sciences, Liverpool John Moores University, Liverpool, UK Estrogen-like activities in Vitex species from China determined by a cell based proliferation assay Y. Hu1, Q.-Y. Zhang1, T.-T. Hou1, H.-L. Xin1, H.-C. Zheng1, K. Rahman2, L.-P. Qin1 Received February 14, 2007, accepted March 29, 2007 Prof. Lu-Ping Qin, Departement of Pharmacognosy, School of Pharmacy, Second Military Medical Uni- versity, 325 Guohe Road, Shanghai 200433, China [email protected], [email protected] Pharmazie 62: 872–875 (2007) doi: 10.1691/ph.2007.11.7542 Ethanolic extracts of four Chinese medicinally used Vitex species were selected and tested for their estrogen-like activities, using an ERa-positive MCF-7 cell based proliferation assay (E-screen assay) and cell cycle analysis (flow cytometry). Vitex negundo displayed the highest estrogenic-like activity, and could be useful in hormone replacement therapy (HRT). 1. Introduction 2. Investigations, result and discussion Phytoestrogens are plant-derived compounds with estro- In the E-Screen assay using MCF-7 cells, the proliferative genic or antiestrogenic properties (Umland et al. 2000). effect of the extracts relative to that of estradiol (1 nM, They seem to be interesting by their possible use as al- 100%) is expressed as Relative Proliferative Effect (RPE) ternative medicines for treating hormonal disorders such (Fig. 1). The results clearly indicate that the extracts from as in hormone replacement therapy (HRT). Thus, phy- V. rotundifolia and V. negundo were able to significantly toestrogens could be beneficial in treatment of the symp- stimulate MCF-7 cell proliferation at concentrations of toms of menopause and hence help to prevent bone re- 50 mg/mL to100 mg/mL (P < 0.01). -
Vitex Rotundifolia L.F
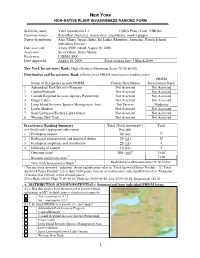
NEW YORK NON -NATIVE PLANT INVASIVENESS RANKING FORM Scientific name: Vitex rotundifolia L.f. USDA Plants Code: VIRO80 Common names: Roundleaf chastetree, beach vitex, chasteberry, monk's pepper Native distribution: Asia (China, Japan), India, Sri Lanka, Mauritius, Australia, Pacific Islands (inlcuding Hawaii) Date assessed: 3 June 2009; edited August 19, 2009 Assessors: Steve Glenn, Gerry Moore Reviewers: LIISMA SRC Date Approved: August 19, 2009 Form version date: 3 March 2009 New York Invasiveness Rank: High (Relative Maximum Score 70.00-80.00) Distribution and Invasiveness Rank ( Obtain from PRISM invasiveness ranking form ) PRISM Status of this species in each PRISM: Current Distribution Invasiveness Rank 1 Adirondack Park Invasive Program Not Assessed Not Assessed 2 Capital/Mohawk Not Assessed Not Assessed 3 Catskill Regional Invasive Species Partnership Not Assessed Not Assessed 4 Finger Lakes Not Assessed Not Assessed 5 Long Island Invasive Species Management Area Not Present Moderate 6 Lower Hudson Not Assessed Not Assessed 7 Saint Lawrence/Eastern Lake Ontario Not Assessed Not Assessed 8 Western New York Not Assessed Not Assessed Invasiveness Ranking Summary Total (Total Answered*) Total (see details under appropriate sub-section) Possible 1 Ecological impact 40 ( 40 ) 37 2 Biological characteristic and dispersal ability 25 ( 25 ) 20 3 Ecological amplitude and distribution 25 ( 25 ) 4 4 Difficulty of control 10 ( 10 ) 8 Outcome score 100 ( 100 )b 73.00 a † Relative maximum score 73.00 § New York Invasiveness Rank High (Relative Maximum Score 70.00-80.00) * For questions answered “unknown” do not include point value in “Total Answered Points Possible.” If “Total Answered Points Possible” is less than 70.00 points, then the overall invasive rank should be listed as “Unknown.” †Calculated as 100(a/b) to two decimal places. -

(Lamiaceae and Verbenaceae) Using Two DNA Barcode Markers
J Biosci (2020)45:96 Ó Indian Academy of Sciences DOI: 10.1007/s12038-020-00061-2 (0123456789().,-volV)(0123456789().,-volV) Re-evaluation of the phylogenetic relationships and species delimitation of two closely related families (Lamiaceae and Verbenaceae) using two DNA barcode markers 1 2 3 OOOYEBANJI *, E C CHUKWUMA ,KABOLARINWA , 4 5 6 OIADEJOBI ,SBADEYEMI and A O AYOOLA 1Department of Botany, University of Lagos, Akoka, Yaba, Lagos, Nigeria 2Forest Herbarium Ibadan (FHI), Forestry Research Institute of Nigeria, Ibadan, Nigeria 3Department of Education Science (Biology Unit), Distance Learning Institute, University of Lagos, Akoka, Lagos, Nigeria 4Landmark University, Omu-Aran, Kwara State, Nigeria 5Ethnobotany Unit, Department of Plant Biology, Faculty of Life Sciences, University of Ilorin, Ilorin, Nigeria 6Department of Ecotourism and Wildlife Management, Federal University of Technology, Akure, Ondo State, Nigeria *Corresponding author (Email, [email protected]) MS received 21 September 2019; accepted 27 May 2020 The families Lamiaceae and Verbenaceae comprise several closely related species that possess high mor- phological synapomorphic traits. Hence, there is a tendency of species misidentification using only the mor- phological characters. Herein, we evaluated the discriminatory power of the universal DNA barcodes (matK and rbcL) for 53 species spanning the two families. Using these markers, we inferred phylogenetic relation- ships and conducted species delimitation analysis using four delimitation methods: Automated Barcode Gap Discovery (ABGD), TaxonDNA, Bayesian Poisson Tree Processes (bPTP) and General Mixed Yule Coalescent (GMYC). The phylogenetic reconstruction based on the matK gene resolved the relationships between the families and further suggested the expansion of the Lamiaceae to include some core Verbanaceae genus, e.g., Gmelina. -

A Taxonomic Revision of the Genus Vi7ex L
J. Adelaide Sot. Gard. 10(1): 31-79(1987) A TAXONOMIC REVISION OF THE GENUS VI7EX L. (VERBENACEAE)* IN AUSTRALIA Ahmad Abid Munir State Herbarium, Botanic Gardens, North Terrace, Adelaide, South Australia 5000 Abstract A taxonomic revision of Vitex in Australia is presented. The following eight species are recognised: V. acuminata, V. bentlzamiana, V. glabrata, V. helogiton, V. melicopea, V. rotundifolia, V. trifolia and V. velutinifolia. V. velutinifolia (from Western Australia) is described as new. V. melicopea and V. helogiton are reinstated, with V. helogiton being recorded from Australia for the first time. V. rotundifolia is reinstated as the oldest valid name for the 1-foliolate species previously often named V. ovata, V. tnfolia var. ovata, V. &Oita var. unifoliolata, V. trifolia var. simplicifolia or V. trtfolia subsp. littoralis. V. tnfolia var, bicolor is placed in synonymy of V. trifolia var. trifolia. The following four species are typified: V. acuminata, V. benthamiana, V. helogiton and V. melicopea. A mnge of material of the non- endemic species was examined from Malesia. Affinities and distribution are considered for each species. A key to the species is provided and a detailed description of each species is supplemented by a habit sketch of a flowering branch and analytical drawings of the flower. Taxonomic History of the Genus The genus Vitex was described by Linnaeus (1753) with four species, V. agnus-castus, V trifolio, V. negundo and V. pinnata. The syntypes of the first named species came from Sicily and Naples, the second and third from India, and the fourth type from Ceylon. The genus was placed together with Clerodendrum, Gmelina and a few other genera of present Verbenaceae in "Didynamia Angiospermia", where it was retained by Murray (1774), Reichard (1778), Loureiro (1793), Schreber (1791), Gmelin (1792), Persoon (1797, 1807), Willdenow (1800), Link (1822), Lamarck & Poiret (1823), Sprengel (1825), Roxburgh (1832), Dietrich (1842) and a few others. -

Preference and Suitability of Nigerian Grown Gmelina Arborea Linn. Roxb
International Journal of Scientific & Engineering Research, Volume 5, Issue 5, May-2014 1484 ISSN 2229-5518 Preference and Suitability of Nigerian Grown Gmelina arborea Linn. Roxb. and Vitex doniana Sweet Woods for Beekeeping in Imeko, Nigeria Adedeji, G. A. and A.A. Aiyeloja. Abstract It has been observed that Apis mellifera native to tropical Africa has special preferential nesting behaviour for white and yellow woods’ cavities in Nigeria. In contrast, the use of brown coloured wood like Milicia excelsa for beekeeping on the ground of its durability has been recommended in Ghana. In response to this, the study investigated the suitability of one exotic white coloured wood species (Gmelina arborea), one indigenous white coloured wood species (Vitex doniana) and one indigenous brown coloured wood species (Erythrophleum suaveolens) for beekeeping in Imeko between February, 2009 and April, 2012. A total of 9 hives comprising 3 each of Erythrophleum suaveolens, Gmelina arborea and Vitex doniana woods were placed at three different sites (1,2,3) within Nazareth High School Compound Imeko. At each site, 3 hives placed comprised the mixture of the 3 wood species’ hives. Colonisation of hives made of G. arborea and V. doniana woods within two months of placement at the 3 sites were observed. Honeybees colonized E. suaveolens wood hive at site 3 and absconded in the same month of colonisation (October, 2010). Quantitative analysis of the wood samples’ extracts indicated the presence of 39.62mg/g total alkaloids, 1.38mg/g total flavonoids, 84.19mg/g total phenol, 366.52mg/g total Saponins and 101.18mg/g total tannins in E. -

Antineoplastic Potential of the Vitex Species: an Overview
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromáticas BOLETÍN LATINOAMERICANO Y DEL CARIBE DE PLANTAS MEDICINALES Y AROMÁTICAS 17 (5): 492 - 502 (2018) © / ISSN 0717 7917 / www.blacpma.usach.cl Revisión | Review Antineoplastic potential of the Vitex species: An overview [Potencial antineoplásico de la especie Vitex: una visión general] Manisha Nigam1, Sarla Saklani2, Sergey Plygun3,4 & Abhay Prakash Mishra2 1Department of Biochemistry, H. N. B. Garhwal (A Central) University, Srinagar Garhwal, 246174, Uttarakhand, India 2Department of Pharmaceutical Chemistry, H. N. B. Garhwal (A Central) University, Srinagar Garhwal, 246174, Uttarakhand, India 3All Russian Research Institute of Phytopathology, Moscow Region, Russia 4European Society of Clinical Microbiology and Infectious Diseases, Basel, Switzerland Contactos | Contacts: Abhay Prakash MISHRA - E-mail address: [email protected] Abstract: Irrespective of progressive treatments, cancer remains to have the utmost rate of treatment failure due to numerous reasons associated. In recent years, the use of traditional medicine in cancer research has established considerable interest. Natural products represent an amazing source for cancer therapy and combating associated side-effects. More than thousand plants have been found to possess significant anticancer properties. Vitex is the largest genus in the family Lamiaceae which comprises 250 species distributed throughout world and several species have been reported to have anticancer properties. Despite a long tradition of use of some species, the genus has not been explored properly in terms of its anticancer profile. Here we are reporting the updated knowledge of the antineoplastic profile of this genus available so far. -

Lamiales – Synoptical Classification Vers
Lamiales – Synoptical classification vers. 2.6.2 (in prog.) Updated: 12 April, 2016 A Synoptical Classification of the Lamiales Version 2.6.2 (This is a working document) Compiled by Richard Olmstead With the help of: D. Albach, P. Beardsley, D. Bedigian, B. Bremer, P. Cantino, J. Chau, J. L. Clark, B. Drew, P. Garnock- Jones, S. Grose (Heydler), R. Harley, H.-D. Ihlenfeldt, B. Li, L. Lohmann, S. Mathews, L. McDade, K. Müller, E. Norman, N. O’Leary, B. Oxelman, J. Reveal, R. Scotland, J. Smith, D. Tank, E. Tripp, S. Wagstaff, E. Wallander, A. Weber, A. Wolfe, A. Wortley, N. Young, M. Zjhra, and many others [estimated 25 families, 1041 genera, and ca. 21,878 species in Lamiales] The goal of this project is to produce a working infraordinal classification of the Lamiales to genus with information on distribution and species richness. All recognized taxa will be clades; adherence to Linnaean ranks is optional. Synonymy is very incomplete (comprehensive synonymy is not a goal of the project, but could be incorporated). Although I anticipate producing a publishable version of this classification at a future date, my near- term goal is to produce a web-accessible version, which will be available to the public and which will be updated regularly through input from systematists familiar with taxa within the Lamiales. For further information on the project and to provide information for future versions, please contact R. Olmstead via email at [email protected], or by regular mail at: Department of Biology, Box 355325, University of Washington, Seattle WA 98195, USA. -

Micronesica 32(2):229-244, 2000
Micronesica 32(2):229-244, 2000 Structure of a Limestone Forest on Northern Guam JOHN M. MORTON,1 FRED A. AMIDON2 U.S. Fish and Wildlife Service, Pacific Islands EcoRegion, Dededo, GU 96912 LENA R. QUINATA I Tano' Consulting, Agana, GU 96910 Abstract—Area 50 is a unique 24-ha patch of limestone forest on Andersen Air Force Base in northern Guam. In advance of feral deer and pig removal, we sampled the woody and herbaceous plant communities on 50 random plots, 30 inside Area 50 (experimental) and 20 outside Area 50 (control) to establish baseline conditions. The limestone forest in Area 50 included 41 genera from 27 families; 29 (71%) of these genera were indigenous. Plots within Area 50 had significantly more woody taxa, higher stem densities, and higher basal areas than control plots. However, mean species richness and stem density within the ground flora were similar between experimental and control plots. We identify three mechanisms by which alien taxa appear to be invading the native limestone forest: failure of many native overstory species to successfully regenerate, recruitment of mostly herbaceous alien species into the ground layer, and recruitment of mostly woody alien species along the forest edge. We also discuss sampling design and analytical considerations for quantifying vegetative changes after ungulate removal. Introduction Sambar deer (Cervus mariannus) and feral pigs (Sus scofa) were introduced to Guam in the 1770s and late 1600s, respectively (Conry 1988). By the mid 1980s, feral ungulate populations in the northern limestone forest were estimated to be as high as 110 pigs/km2 and 212 deer/10 km of road transect (Conry 1988). -

Invasive Species Fact Sheet
HOW YOU CAN HELP INVASIVE SPECIES FACT SHEET Currently, an effort is being made by Mississippi State University, in cooperation with the South Carolina/North Carolina Beach Task Force, to determine the distribution of beach vitex in the Southeast and Mid-South. This infor- Beach vitex (Vitex Rotundifolia L.f.) mation which is being maintained in online databases by Mississippi State University (www.gri.msstate.edu) and Description, Distribution, and Management the South Carolina Beach Vitex Task Force (http://www.beachvitex.org), is very important in developing appropriate Victor Maddox, Ph.D., Postdoctoral Associate, Mississippi State University John D. Byrd, Jr., Ph.D., Extension/Research Professor, Mississippi State University strategies for addressing the plant. Please send reports of suspected beach vitex populations, including GPS coor- Randy Westbrooks, Ph. D., Invasive Species Specialist, U.S. Geological Survey dinates, site description / ownership, and photo images to: Victor Maddox, GeoResources Institute, Box 9555, Mis- Betsy Brabson, Ph. D., South Carolina Beach Vitex Task Force sissippi State, MS 39762-9652, Ph. 662-325-2123, E-mail: [email protected]; or to Betsy Brabson, South GRI Publication #5020 Carolina Beach Vitex Task Force, Georgetown, SC, Ph. 843-546-9531; E-mail: [email protected]. There are other ways to help with this effort, as well: INTRODUCTION Beach vitex (Vitex rotundifolia L.f.) is a deciduous woody • Do not plant beach vitex. Use native species such as sea oats. vine that was introduced to the Southeastern U.S. from • Remove beach vitex seedlings from public beach areas. Korea in the mid-1980s. Prior to its intoduction to the • Contact the GeoResources Institute for advice on removal of mature beach vitex colonies, and replacement with South Atlantic coast of the U.S., beach vitex had no native plant species. -

Nirgundi (Vitex Negundo) – Nature's Gift to Mankind
Full-length paper Asian Agri-History Vol. 19, No. 1, 2015 (5–32) 5 Nirgundi (Vitex negundo) – Nature’s Gift to Mankind SC Ahuja1, Siddharth Ahuja2, and Uma Ahuja3 1. Rice Research Station, Kaul 136 021, Kaithal, Haryana, India 2. Department of Pharmacology, Vardhman Mahavir Medical College, Safdarjung, New Delhi, India 3. College of Agriculture, CCS Haryana Agricultural University, Kaul 136 021, Haryana, India (email: [email protected]) Abstract Vitex negundo (nirgundi, in Sanskrit and Hindi) is a deciduous shrub naturalized in many parts of the world. Some consider it to have originated in India and the Philippines. There is no reference to nirgundi in the Vedas, while several references occur in post-Vedic works. In India, the plant has multifarious uses: basketry, dyeing, fuel, food, stored-grain protectant, fi eld pesticide, growth promoter, manure, as medicine for poultry, livestock, and humans. It is used in all systems of treatment – Ayurveda, Unani, Siddha, Homeopathy, and Allopathy. It is commonly used in folk medicine in India, Bangladesh, China, Philippines, Sri Lanka, and Japan. True to its meaning in Sanskrit (that which keeps the body free from all diseases), it is used to treat a plethora of ailments, ranging from headache to migraine, from skin affections to wounds, and swelling, asthmatic pains, male and female sexual and reproductive problems. Referred to as sindhuvara in Ayurveda, nirgundi has been used as medicine since ancient times. It is taken in a variety of ways, both internally and externally. The whole plant, leaves, leaf oil, roots, fruits, and seeds are administered in the treatment of specifi c diseases. -

Two New Records for the Lamiaceae of Singapore
Gardens’ Bulletin Singapore 68(2): 189–200. 2016 189 doi: 10.3850/S2382581216000144 Two new records for the Lamiaceae of Singapore R.P.J. de Kok1, S. Sengun2,3 & G.L.C. Bramley3 1Honorary Research Associate, Singapore Botanic Gardens, National Parks Board, 1 Cluny Road, Singapore 259569 [email protected] 2Birkbeck, University of London, Malet St, London WC1E 7HX, U.K. 3Royal Botanic Gardens Kew, Richmond, Surrey TW9 3AE, U.K. ABSTRACT. The species of Lamiaceae have recently been revised for Singapore. In total 44 species in 21 genera are recorded, of which 23 species are native, an additional five are probably native, and 16 are non-native species which have naturalised in Singapore. One new record for Singapore has been found (Vitex rotundifolia) and one species reinstated (Callicarpa pentandra) after being ignored for over a hundred years. Keywords. Callicarpa pentandra, conservation, distributions, Vitex rotundifolia Introduction The Lamiaceae (Mint Family) is of major ecological and economic importance in Southeast Asia. It includes major (Gmelina L. & Tectona L.f.) and minor (Teijsmanniodendron Koord. and Vitex L.) timber groups. It is important horticulturally (Clerodendrum L. and its close relatives), culinarily (Mentha L. and Ocimum L.) and medicinally (Vitex). As a consequence, members of the family are often cultivated and have been moved around the region, in some case over many centuries. Taxonomically the family is complex with many species-rich genera, some of which have undergone major nomenclatural changes in the last 10 years (De Kok, 2007, 2008, 2012, 2013; Bramley, 2009; De Kok et al., 2009; Wearn & Mabberley, 2011). Worldwide, the family consists of around 236 genera and about 7200 species (Harley et al., 2004), while in the Flora Malesiana region 50 genera with 302 species are recorded (Bramley et al., in press).