IMPROVING MATERNAL and CHILD INSIDE.Indd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Architect of New India Fortnightly Magazine Editor Prabhat Jha
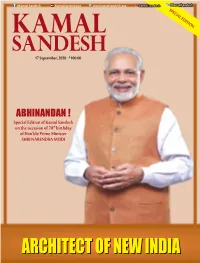
@Kamal.Sandesh KamalSandeshLive www.kamalsandesh.org kamal.sandesh @KamalSandesh SPECIAL EDITION 17 September, 2020 `100.00 ABHINANDAN ! Special Edition of Kamal Sandesh on the occasion of 70th birthday of Hon’ble Prime Minister SHRI NARENDRA MODI ARCHITECTARCHITECT OFOF NNEWEWArchitect ofII NewNDINDI India KAMAL SANDESHAA 1 Self-reliant India will stand on five Pillars. First Pillar is Economy, an economy that brings Quantum Jump rather than Incremental change. Second Pillar is Infrastructure, an infrastructure that became the identity of modern India. Third Pillar is Our System. A system that is driven by technology which can fulfill the dreams of the 21st century; a system not based on the policy of the past century. Fourth Pillar is Our Demography. Our Vibrant Demography is our strength in the world’s largest democracy, our source of energy for self-reliant India. The fifth pillar is Demand. The cycle of demand & supply chain in our economy is the strength that needs to be harnessed to its full potential. SHRI NARENDRA MODI Hon’ble Prime Minister of India 2 KAMAL SANDESH Architect of New India Fortnightly Magazine Editor Prabhat Jha Executive Editor Dr. Shiv Shakti Bakshi Associate Editors Ram Prasad Tripathy Vikash Anand Creative Editors Vikas Saini Bhola Roy Digital Media Rajeev Kumar Vipul Sharma Subscription & Circulation Satish Kumar E-mail [email protected] [email protected] Phone: 011-23381428, FAX: 011-23387887 Website: www.kamalsandesh.org 04 EDITORIAL 46 2016 - ‘IndIA IS NOT 70 YEARS OLD BUT THIS JOURNEY IS -

(PANCHAYAT) Government of Gujarat
ROADS AND BUILDINGS DEPARTMENT (PANCHAYAT) Government of Gujarat ENVIRONMENTAL AND SOCIAL IMPACT ASSESSMENT (ESIA) FOR GUJARAT RURAL ROADS (MMGSY) PROJECT Under AIIB Loan Assistance May 2017 LEA Associates South Asia Pvt. Ltd., India Roads & Buildings Department (Panchayat), Environmental and Social Impact Government of Gujarat Assessment (ESIA) Report Table of Content 1 INTRODUCTION ............................................................................................................. 1 1.1 BACKGROUND .......................................................................................................... 1 1.2 MUKHYA MANTRI GRAM SADAK YOJANA ................................................................ 1 1.3 SOCIO-CULTURAL AND ECONOMIC ENVIRONMENT: GUJARAT .................................... 3 1.3.1 Population Profile ........................................................................................ 5 1.3.2 Social Characteristics ................................................................................... 5 1.3.3 Distribution of Scheduled Caste and Scheduled Tribe Population ................. 5 1.3.4 Notified Tribes in Gujarat ............................................................................ 5 1.3.5 Primitive Tribal Groups ............................................................................... 6 1.3.6 Agriculture Base .......................................................................................... 6 1.3.7 Land use Pattern in Gujarat ......................................................................... -

Scheme for Incentive to Industries Preamble One of the Leading Industrial States. Government of Gujarat Has Announced an The
Guiarat Industrial Policy 2015 - Scheme for Incentive to Industries Government of Guiarat Industries & Mines Department Resolution No.INC-10201 5-645918-I Sachivalaya, Gandhinagar Dated: 25/07 /20L6 Read: Industrial Policy 2015 of Government of Gujarat Preamble Gujarat has always been at the forefront of economic growth in the country. It is one of the leading industrial states. Government of Gujarat has announced an ambitious Industrial Poliry 2015, in lanuary 2015, with the objective of creating a healthy and conducive climate for conducting business and augmenting the industrial development of the state. The Industrial Poliry has been framed with the broad idea of enhancing industrial growth that empowers people and creates employment, and establishes a roadmap for improving the state's ability to facilitate business. Gujarat's development vision will continue to emphasize on integrated and sustainable development, employment generation, opportunities for youth, increased production and inclusive growth. Make in India is a prestigious program of Government of India. The Industrial Poliry 2015 ofthe Government of Gujarat envisages a focused approach on the Make in India program as the state's strategy for achieving growth. Gujarat is a national leader in 15 of the 25 sectors identified under the Make in India program, and is also focusing on 6 more sectors. Thus, with a strong base in 21 out of the 25 sectors under Make in India, Gujarat can take strong leadership in this prestigious program of the Government of India. The Industrial Policy 2015 aims to encourage the manufacturing sector to upgrade itself to imbibe cutting edge technology and adopt innovative methods to significantly add value, create new products and command a niche position in the national and international markets. -

District Disaster Management Plan-2017 Bhavnagar Volume-II
District Disaster Management Plan-2017 Bhavnagar Volume-II Gujarat State Disaster Management Authority and District Collector Office - Bhavnagar 1 Prologue Bhavnagar district has a number of villages at the coastal region of Arabian Sea and also many Hazardous industries are there, Worlds’ largest Ship Recycling Yard Alang; there hazardous materials are handled. Bhavnagar has faced multitude of Disasters like Flood, Cyclone, Heavy Rain, Lightening, Earthquake and Fire. Experience has shown that pre- planned and practiced procedures for handling an emergency can considerably reduce loss of life and minimize damage too. But now under the Disaster Risk Management Program Gujarat State Disaster Management Authority, and Collector Office Bhavnagar are preparing the communities and Government Officials from grass root level to top level for securing quick response mechanism right from bottom to top level under the four DRM Components. These are Capacity Building, Awareness Generation, Mock drill and Plan Preparation. The Role of each agency in the event of an emergency is specified. Needless to say that the success of disaster management depends upon the co-coordinator and effective performance of the duties assigned to each and every agency. The multy-hazard District Disaster Management plan of Bhavnagar is divided in two Volume. This volume-II is a comprehensive document covering all possible hazards, with a systematic analyses of risk and vulnerability, element at risk and level of impact through scientific and experience developed by the core team of district administration. This plan is a necessary document for reducing risks due to hazards and vulnerability; I hope this great document would be really helpful for protecting life and properties as well as sustainable development in future. -

Cabinet Ministers of India 2019 Pdf Download Telugu
Cabinet ministers of india 2019 pdf download telugu Continue 2,139 total views, 1 view today Download PDF on ministers of the Union of India government 2019. The list includes cabinet ministers, a minister of state (independent charge), a minister of state. We've updated every portfolio of cabinet ministers. Useful for all competitive exams. Write 5 GrandsTests on AP Grama/Ward Sachivalayam Only for Rs.99/- Only. List of Ministers of The Cabinet of the Union of India 2019 Ministers of The Cabinet of the Union of India 2019 Download Ministers of The Cabinet of the Union of India 2019 PDF. AP Grama/Ward Sachivalayam related posts Modi's cabinet 2.0: Shah gets home, Rajnath Defence, Nirmala first female finance ministerNEW DELHI: Here's a list of portfolios allocated to cabinet ministers and ministers of state (independent charge): Narendra Modi: Prime Minister and also in charge: Ministry of Personnel, Public Complaints and Pensions; Atomic Energy Department; Department of Space; and all important political issues; and any other tassors not assigned to any minister. CABINET MINISTERS ON 1 OCTOBER 2015. Rajnath Singh: Defence Minister. 2. Amit Shah: Interior Minister. 3. Nitin Jairam Gadkari : Minister of Road Transport and Highways; and Minister for Micro, Small and Medium-sized Enterprises. 4. D V Sadananda Gowda: Minister of Chemicals and Fertilisers. 5. Nirmala Sitharaman: Minister of Finance; and Minister of Corporate Affairs. 6. Ramvilas Paswan: Minister of Consumer Affairs, Food and Public Distribution. 7. Narendra Singh Tomar: Minister of Agriculture and Agriculture; Minister for Rural Development; and Minister Panchayati Raj. 8. Ravi Shankar Prasad : Minister of Law and Justice; Minister of Communications; and Minister for Electronics and Information Technology. -

Available Phosphorus in Soil of Halol, Kalol and Morva Hadaf Taluka Territory of Panchmahal District by Soil Health Card Study Project
Available online a twww.scholarsresearchlibrary.com Scholars Research Library Archives of Applied Science Research, 2016, 8 (8):8-13 (http://scholarsresearchlibrary.com/archive.html) ISSN 0975-508X CODEN (USA) AASRC9 Available phosphorus in soil of Halol, Kalol and Morva Hadaf taluka Territory of Panchmahal District by soil health card study project Dilip H. Pate 1 and M. M. Lakdawala Chemistry Department, S P T Arts and Science College, Godhra, Gujarat, India _____________________________________________________________________________________________ ABSTRACT Under Gujarat Government “Soil Health Card Project” this results are reproduced, This physico-chemical study of soil covers various parameters like pH, conductivity, Total Organic Carbon, Available Nitrogen (N), Available Phosphorus (P 2O5) and Available Potassium (K 2O). This study lead us to the conclusion about the nutrient’s quantity and quality of soil of Halol, Kalol and Morva hadaf Taluka, District- Panchmahal, Gujarat. Results show that average all the villages of all three talukas have medium and very few have high Phosphorus content. The fertility index for phosphorus for all three talukas is average 2.00. This information will help farmer to know the status of their farms, requirements of nutrients addition for soil for the next crop session, that means which fertilizer to be added. Key words: Quality of soil, fertility index, Kalol, Gujarat _____________________________________________________________________________________________ INTRODUCTION Soil composition is: -

January 2019
Consulate General of India Perth INDIA BULLETIN JANUARY 2019 Indian Economy: IMF hikes India's GDP growth forecast to 7.5%; India 4th most attractive investment market: PwC pegs China's at 6.6% survey CEOs’ confidence in global economic growth has dipped dramatically by a record jump in pessimism but India has emerged as ‘the rising star’ by surpassing the UK to become fourth most attractive destination, a PwC survey said. The survey of more than 1,300 CEOs in 91 countries saw India’s popularity falling marginally The IMF’s database also suggested that India’s from 9 per cent to 8 per cent. The US topped with 27 contribution to world growth has increased from 7.6 per cent (down from 46 per cent last year), followed by per cent during 2000-2008 to 14.5 per cent in 2018. India China with 24 per cent (down from 33 per cent) and retained the fastest growing large economic growth tag Germany at 13 per cent (down from 20 per cent). as its nearest rival China is projected to have grown 6.6 per cent in 2018 and 6.2 per cent in 2019. Read More: Read More: https://www.thehindubusinessline.com/economy/indi a-4th-most-attractive-investment-market-pwc- https://www.business-standard.com/article/economy- survey/article26058293.ece policy/imf-hikes-india-s-gdp-growth-forecast-to-7-5- pegs-china-s-at-6-6-119012101284_1.html INDIA BULLETIN | Consulate General of India, Perth India to become bigger than China eventually, says India set to become third-largest consumer former RBI Governor Raghuram Rajan market: WEF India will eventually surpass China in economic size and will be in a better position to create the infrastructure being promised by the Chinese side in India is set to become the third-largest consumer South Asian countries, former RBI Governor Raghuram market behind only the US and China and consumer Rajan said. -

Honourable Speaker Sir, During the Last Two Decades, Our Government Has Adopted a Well-Planned Approach with a Long Term Vision for the Development of the State
Honourable Speaker Sir, During the last two decades, our Government has adopted a well-planned approach with a long term vision for the development of the State. The people of the state and the country are witnessing the encouraging results of these efforts. There was a time, when we used to present plans of the Government in the form of budget, some people used to be skeptical and trivialize its importance by calling it a dream. However, today the nation and the world has taken note of the success saga of Gujarat. And therefore, the people of Gujarat have time and again expressed their confidence in our development oriented approach and we are grateful to the people of the State for the same. Our Government is continuously marching on the development path on the foundation of the four pillars of Sensitivity, Transparency, Decisiveness and Progressiveness. We are committed to the social, economic, educational and overall development of every citizen of the state. Government is ensuring that the fruits of development reach to the poorest of the poor and they also play an important role in the development process of the State. Our Governance is based on the principle of "Sau no Sath Sau no Vikas", involving all sections of the society in the main stream development process through a well planned approach. On the one hand through Vibrant Gujarat Global Summit, Gujarat has established a unique global identity as most favoured trade and investment destination. On the other hand, the Government has ensured irrigation facilities through efficient water management of Saradar Sarovar Narmada Project and strengthening of other irrigation schemes in order to increase agricultural productivity and to achieve high agricultural growth rate. -

Gujarat in Figures
GUJARAT RUDABAI STEPWELL IN ADALAJ March 2021 For updated information, please visit www.ibef.org Table of Contents Executive Summary 3 Introduction 4 Economic Snapshot 9 Physical Infrastructure 15 Social Infrastructure 27 Industrial Infrastructure 30 Key Sectors 33 Key Procedures & Policies 47 Appendix 62 2 Executive summary Preferred Investment Destination . According to the Department for Promotion of Industry and Internal Trade (DPIIT), Foreign Direct Investment (FDI) 1 inflows in Gujarat stood at US$ 47.8 billion between April 2000 and December 2020. Port Capital of India . Gujarat is the first state in India to undertake port privatisation. Gujarat Maritime Board has developed multiple port 2 privatisation models such as private/joint sector ports, private jetties, captive jetties and GMB jetties. Highest Share in India’s Total Dairy Output . Gujarat is the fifth-largest state in milk production in India. In 2019-20, per day 203.43 lakh litre milk was received in 22 3 co-operative dairy plants. There are 19,522 co-operative milk societies in the state. Strong Textile Base . The state attracted investment commitments worth US$ 1,407 million under Gujarat's textile policy 2012, for varied 4 units such as processing, spinning, weaving, made-ups, technical textiles etc. Note: MT- Million Tonnes, FDI- Foreign Direct Investment Source: Gujarat Economic Review, 2020-21, Ministry of Textiles, Industrial Extension Bureau, 3 INTRODUCTION 4 Gujarat fact file Gandhinagar Capital 308 persons per sq km 60.3 million Population density total population 196,024 sq.km. geographical area 28.9 million 31.5 million female population male population Source: Maps of India 919:1000 Sex ratio 79.31% 33 Administrative (females per 1,000 males) Key Insights literacy rate districts • There are seven agro-climatic zones in the state that support cultivation of a wide range of crops. -

The Economy of Gujarat and Its Policies Priyanka R Patani [email protected] Gujarat University, Ahmedabad, Gujarat
Patani Priyanka R; International Journal of Advance Research, Ideas and Innovations in Technology ISSN: 2454-132X Impact factor: 4.295 (Volume 4, Issue 5) Available online at: www.ijariit.com The economy of Gujarat and its policies Priyanka R Patani [email protected] Gujarat University, Ahmedabad, Gujarat ABSTRACT Governmental policies and its impact on the development of Gujarat as the economy of Gujarat is one of the fastest growing economies among all Indian states. The State emerged stronger and a symbol of hope for the rest of the country in terms of economic and industrial development. Gujarat is one of the states to have responded punctually and effectively to the new liberal policies. The government has been open to new ideas, technology, including organizational and management governance practices, and has designed policy responses to overcome economic challenges. The analysis in this paper suggests that stakeholders in Gujarat have been able to create an environment in which improving quality of living, focusing on basic needs, and quality of life are the main focus of public policies and discourse. Such focus is favorable to broad-based growth and upward economic and social mobility, and diversity, permitting introduction of new ideas in organizing different activities. Keywords— Development of Gujarat 1. INTRODUCTION The economy of Gujarat is one of the fastest growing economies among all Indian states. The people of Gujarat are worldwide recognized as highly entrepreneurial and industrious. The risk-taking ability, along with the mature level of commercial knowledge, has made the State the fountainhead of a new enterprise. The labor force in Gujarat is reasonably skilled in areas such as diamonds, chemicals, petrochemicals and pharmacy sectors. -

Hon'ble Speaker Sir, I Rise Before This August House of Glorious Gujarat To
Hon’ble Speaker Sir, I rise before this august House of glorious Gujarat to present the Budget for the year 2008-09 with an overwhelming feeling of joy. I have had the privilege to present the Budget for twelve times in the past and I feel honoured to have this opportunity once again. By mentioning the number of opportunities, I want to convey that the people of Gujarat appreciate the importance of stable governance. Gujarat has captured the imagination of the country and the world with its development. Such development is based on stability in governance, clarity in policy and the objective to achieve the goal. The political and social currents in Gujarat show that the common man of the State has faith in development as well as in our resolve and efforts in achieving it. Every citizen wants to participate in the process of development; because he feels that he is a beneficiary in the comprehensive development process. The response received from the people of Gujarat has encouraged our government to further enhance the already extended canvass of development. Gujarat is going to celebrate the Golden Jubilee of its formation in the year 2010 and I express my desire before this august House that it will display more than the required commitment to convert this occasion into an opportunity for development. Such commitment by this House, which would be a ray of hope for five and a half crore Gujaratis, will form an emotional bond with the common man and help us in marching ahead for the progress of one and all. -

Content Introduction 1
PM Modi at Krishi Unnati Mela, 2018 Content Introduction 1 CHAPTER 1: PRO-FARMER REFORMS – FREEDOM, 6 PROTECTION AND HIGHER INCOME Background of Reforms 6 Need for Pro-Farmer Reforms 7 Benefits of the New Farm Laws in a Nutshell 11 Impact of the Law which Gives Freedom to Sell Anywhere 13 Impact of Contract Farming Law 15 Myth and Reality 17 Timeline of Consensus and Consultation on Farm Reforms 21 Two Decades of Consultations 23 Success Stories 31 CHAPTER 2: TOWARDS DOUBLING FARMERS’ INCOME 34 SINCE Agri-Budget 35 Sustainable Farming and Soil Health 39 Access to Credit 43 Water and Electricity 47 Help during Distress 51 Insurance 55 Minimum Support Price (MSP) 61 Market Access 75 Value Addition and Enabling Ecosystem 79 Additional Income Opportunities 89 Financial Security 95 INTRODUCTION Independent India has seen many Prime Ministers but among them, Narendra Modi is unique. Before going onto win the 2014 Lok Sabha elections, he had been Chief Minister of a state for over thirteen years. As Chief Minister, Modi was known to be someone who immersed himself deeply in the intricacies of policy matters and the way they work on the ground. Transforming Lives of Farmers in Gujarat Among the biggest policy triumphs of his tenure as Chief Minister of Gujarat was the way he transformed the lives of farmers of a semi- arid state and made them self-reliant and prosperous. Modi’s working style when it came to farmer welfare was bottom up – his policy was driven by his deep understanding of farmers’ problems and in finding innovative win-win solutions for them.