Clinical, Radiological, and Chondro
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mackenzie's Mission Gene & Condition List
Mackenzie’s Mission Gene & Condition List What conditions are being screened for in Mackenzie’s Mission? Genetic carrier screening offered through this research study has been carefully developed. It is focused on providing people with information about their chance of having children with a severe genetic condition occurring in childhood. The screening is designed to provide genetic information that is relevant and useful, and to minimise uncertain and unclear information. How the conditions and genes are selected The Mackenzie’s Mission reproductive genetic carrier screen currently includes approximately 1300 genes which are associated with about 750 conditions. The reason there are fewer conditions than genes is that some genetic conditions can be caused by changes in more than one gene. The gene list is reviewed regularly. To select the conditions and genes to be screened, a committee comprised of experts in genetics and screening was established including: clinical geneticists, genetic scientists, a genetic pathologist, genetic counsellors, an ethicist and a parent of a child with a genetic condition. The following criteria were developed and are used to select the genes to be included: • Screening the gene is technically possible using currently available technology • The gene is known to cause a genetic condition • The condition affects people in childhood • The condition has a serious impact on a person’s quality of life and/or is life-limiting o For many of the conditions there is no treatment or the treatment is very burdensome for the child and their family. For some conditions very early diagnosis and treatment can make a difference for the child. -

Rapid Publication International Nosology and Classification of Constitutional Disorders of Bone
American Journal of Medical Genetics 113:65–77 (2002) Rapid Publication International Nosology and Classification of Constitutional Disorders of Bone (2001) Christine M. Hall* Department of Radiology, Great Ormond Street Children’s Hospital, London, United Kingdom The last International Classification of Con- combination of morphological and molecular groupings stitutional Disorders of Bone was published it is anticipated that two parallel but interacting clas- in 1998. Since then rapid advances have been sifications will evolve: one clinical, identifying accepted made in identifying the molecular changes terminology or nosology, and the other molecular, to responsible for defined conditions and new help further understand the pathogenesis of individual disorders are constantly being delineated. disorders. For these reasons a further update on the The major change in the classification has been the classification is appropriate. It has been addition of genetically determined dysostoses to the expended to not only the osteochondrodys- skeletal dysplasias or osteochondrodysplasias. This is plasias (33 groups) but also genetically deter- because in clinical practice these two groups overlap. mined dysostoses (3 groups). Dysostoses may be defined as skeletal malformations ß 2002 Wiley-Liss, Inc. occurring singly or in combination. The dysostoses are static and their malformations occur during blastogen- KEY WORDS: osteochondrodysplasia; dys- esis (the first eight weeks of embryonic life). This is in ostosis; gene contrast to the skeletal dysplasias which often present after this stage, have a more general skeletal involve- ment and continue to evolve as a result of active gene The International Working Group on the Classifica- involvement throughout life. Only those dysostoses tion of Constitutional Disorders of Bone met in Oxford which have an identified chromosomal locus have been on September 4th and 5th 2001 to update the last clas- included. -

Blueprint Genetics Comprehensive Skeletal Dysplasias and Disorders
Comprehensive Skeletal Dysplasias and Disorders Panel Test code: MA3301 Is a 251 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of disorders involving the skeletal system. About Comprehensive Skeletal Dysplasias and Disorders This panel covers a broad spectrum of skeletal disorders including common and rare skeletal dysplasias (eg. achondroplasia, COL2A1 related dysplasias, diastrophic dysplasia, various types of spondylo-metaphyseal dysplasias), various ciliopathies with skeletal involvement (eg. short rib-polydactylies, asphyxiating thoracic dysplasia dysplasias and Ellis-van Creveld syndrome), various subtypes of osteogenesis imperfecta, campomelic dysplasia, slender bone dysplasias, dysplasias with multiple joint dislocations, chondrodysplasia punctata group of disorders, neonatal osteosclerotic dysplasias, osteopetrosis and related disorders, abnormal mineralization group of disorders (eg hypopohosphatasia), osteolysis group of disorders, disorders with disorganized development of skeletal components, overgrowth syndromes with skeletal involvement, craniosynostosis syndromes, dysostoses with predominant craniofacial involvement, dysostoses with predominant vertebral involvement, patellar dysostoses, brachydactylies, some disorders with limb hypoplasia-reduction defects, ectrodactyly with and without other manifestations, polydactyly-syndactyly-triphalangism group of disorders, and disorders with defects in joint formation and synostoses. Availability 4 weeks Gene Set Description -

Discover Dysplasias Gene Panel
Discover Dysplasias Gene Panel Discover Dysplasias tests 109 genes associated with skeletal dysplasias. This list is gathered from various sources, is not designed to be comprehensive, and is provided for reference only. This list is not medical advice and should not be used to make any diagnosis. Refer to lab reports in connection with potential diagnoses. Some genes below may also be associated with non-skeletal dysplasia disorders; those non-skeletal dysplasia disorders are not included on this list. Skeletal Disorders Tested Gene Condition(s) Inheritance ACP5 Spondyloenchondrodysplasia with immune dysregulation (SED) AR ADAMTS10 Weill-Marchesani syndrome (WMS) AR AGPS Rhizomelic chondrodysplasia punctata type 3 (RCDP) AR ALPL Hypophosphatasia AD/AR ANKH Craniometaphyseal dysplasia (CMD) AD Mucopolysaccharidosis type VI (MPS VI), also known as Maroteaux-Lamy ARSB syndrome AR ARSE Chondrodysplasia punctata XLR Spondyloepimetaphyseal dysplasia with joint laxity type 1 (SEMDJL1) B3GALT6 Ehlers-Danlos syndrome progeroid type 2 (EDSP2) AR Multiple joint dislocations, short stature and craniofacial dysmorphism with B3GAT3 or without congenital heart defects (JDSCD) AR Spondyloepimetaphyseal dysplasia (SEMD) Thoracic aortic aneurysm and dissection (TADD), with or without additional BGN features, also known as Meester-Loeys syndrome XL Short stature, facial dysmorphism, and skeletal anomalies with or without BMP2 cardiac anomalies AD Acromesomelic dysplasia AR Brachydactyly type A2 AD BMPR1B Brachydactyly type A1 AD Desbuquois dysplasia CANT1 Multiple epiphyseal dysplasia (MED) AR CDC45 Meier-Gorlin syndrome AR This list is gathered from various sources, is not designed to be comprehensive, and is provided for reference only. This list is not medical advice and should not be used to make any diagnosis. -

Whole Exome Sequencing Gene Package Skeletal Dysplasia, Version 2.1, 31-1-2020
Whole Exome Sequencing Gene package Skeletal Dysplasia, Version 2.1, 31-1-2020 Technical information DNA was enriched using Agilent SureSelect DNA + SureSelect OneSeq 300kb CNV Backbone + Human All Exon V7 capture and paired-end sequenced on the Illumina platform (outsourced). The aim is to obtain 10 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate and non-unique reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA-MEM algorithm (reference: http://bio-bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x ABCC9 Atrial fibrillation, familial, 12, 614050 601439 65 100 100 95 Cardiomyopathy, dilated, 1O, 608569 Hypertrichotic osteochondrodysplasia, 239850 ACAN Short stature and advanced bone age, with or without early-onset osteoarthritis -

Skeletal Dysplasia Panel Versie V1 (345 Genen) Centrum Voor Medische Genetica Gent
H9.1-OP2-B40: Genpanel Skeletal dysplasia, V1, in voege op 14/02/2020 Skeletal_dysplasia panel versie V1 (345 genen) Centrum voor Medische Genetica Gent Associated phenotype, OMIM phenotype ID, phenotype Gene OMIM gene ID mapping key and inheritance pattern Atrial fibrillation, familial, 12, 614050 (3), Autosomal dominant; ABCC9 601439 Cardiomyopathy, dilated, 1O, 608569 (3); Hypertrichotic osteochondrodysplasia, 239850 (3), Autosomal dominant Congenital heart defects and skeletal malformations syndrome, 617602 (3), Autosomal dominant; Leukemia, Philadelphia ABL1 189980 chromosome-positive, resistant to imatinib, 608232 (3), Somatic mutation Short stature and advanced bone age, with or without early-onset osteoarthritis and/or osteochondritis dissecans, 165800 (3), ACAN 155760 Autosomal dominant; Spondyloepimetaphyseal dysplasia, aggrecan type, 612813 (3), Autosomal recessive; ?Spondyloepiphyseal dysplasia, Kimberley type, 608361 (3), Autosomal dominant Spondyloenchondrodysplasia with immune dysregulation, 607944 ACP5 171640 (3), Autosomal recessive Fibrodysplasia ossificans progressiva, 135100 (3), Autosomal ACVR1 102576 dominant Weill-Marchesani syndrome 1, recessive, 277600 (3), Autosomal ADAMTS10 608990 recessive Weill-Marchesani 4 syndrome, recessive, 613195 (3), Autosomal ADAMTS17 607511 recessive ADAMTSL2 612277 Geleophysic dysplasia 1, 231050 (3), Autosomal recessive AFF4 604417 CHOPS syndrome, 616368 (3), Autosomal dominant AGA 613228 Aspartylglucosaminuria, 208400 (3), Autosomal recessive Rhizomelic chondrodysplasia punctata, -
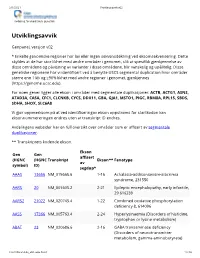
Utviklingsavvik V02
2/1/2021 Utviklingsavvik v02 Avdeling for medisinsk genetikk Utviklingsavvik Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). For noen gener ligger alle ekson i områder med segmentale duplikasjoner: ACTB, ACTG1, ASNS, ATAD3A, CA5A, CFC1, CLCNKB, CYCS, DDX11, GBA, GJA1, MSTO1, PIGC, RBM8A, RPL15, SBDS, SDHA, SHOX, SLC6A8 Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* AAAS 13666 NM_015665.6 1-16 Achalasia-addisonianism-alacrimia syndrome, 231550 AARS 20 NM_001605.2 2-21 Epileptic encephalopathy, early infantile, 29 616339 AARS2 21022 NM_020745.4 1-22 Combined oxidative phosphorylation deficiency 8, 614096 AASS 17366 NM_005763.4 2-24 Hyperlysinaemia (Disorders of histidine, tryptophan or lysine metabolism) ABAT 23 NM_020686.6 2-16 GABA transaminase deficiency (Disorders of neurotransmitter metabolism, gamma-aminobutyrate) -

Opsismodysplasia: Phosphate Wasting Osteodystrophy Responds to Bisphosphonate Therapy
CLINICAL CASE STUDY published: 22 June 2015 doi: 10.3389/fped.2015.00048 Opsismodysplasia: phosphate wasting osteodystrophy responds to bisphosphonate therapy Ansab Khwaja1, Shawn E. Parnell2, Kathryn Ness3, Viviana Bompadre1 and Klane K. White1* 1 Orthopedics and Sports Medicine, Seattle Children’s Hospital, University of Washington, Seattle, WA, USA, 2 Department of Radiology, Seattle Children’s Hospital, University of Washington, Seattle, WA, USA, 3 Division of Endocrinology, Department of Pediatrics, Seattle Children’s Hospital, University of Washington, Seattle, WA, USA We present two siblings affected with opsismodysplasia (OPS), a rare skeletal dysplasia caused by mutations in the inositol polyphosphate phosphatase-like 1 gene. The skeletal findings include short stature with postnatal onset micromelia, marked platyspondyly, squared metacarpals, delayed skeletal ossification, metaphyseal cupping, and postnatal micromelia. Respiratory compromise, delayed ambulation, and progressive lower extremity deformities are described. The severity of findings is variable. Renal phosphate wasting Edited by: Jeff Martus, is associated with severe bone demineralization and a more severe phenotype. This Vanderbilt Children’s Hospital, USA report represents the first described cases of opsismodysplasia treated with intravenous Reviewed by: bisphosphonate (pamidronate). Surgical management for lower extremity deformities Jason Troy Rhodes, University of Colorado, USA associated with OPS is also reviewed. Ryan D. Muchow, Level of Evidence: IV Case series University of Kentucky, USA Christine Ann Ho, Keywords: opsismodysplasia, metabolic bone disease, skeletal dysplasias, scoliosis, genu varum, bisphosphonates Texas Scottish Rite Hospital, USA *Correspondence: Klane K. White, Orthopedics and Sports Medicine, Introduction Seattle Children’s Hospital, University of Washington, 4800 Sand Point Opsismodysplasia (OPS) is a rare autosomal recessive skeletal dysplasia associated with delayed Way, OA.9.120, Seattle, WA, USA bone maturation and micromelia (1, 2). -

Skeletal Dysplasia Panel Versie V2 (346 Genen) Centrum Voor Medische Genetica Gent
H9.1-OP2-B40: Genpanel Skeletal dysplasia, V2, in voege op 26/05/2020 Skeletal_dysplasia panel versie V2 (346 genen) Centrum voor Medische Genetica Gent Associated phenotype, OMIM phenotype ID, phenotype Gene OMIM gene ID mapping key and inheritance pattern Atrial fibrillation, familial, 12, 614050 (3), Autosomal dominant; ABCC9 601439 Cardiomyopathy, dilated, 1O, 608569 (3); Hypertrichotic osteochondrodysplasia, 239850 (3), Autosomal dominant Congenital heart defects and skeletal malformations syndrome, 617602 (3), Autosomal dominant; Leukemia, Philadelphia ABL1 189980 chromosome-positive, resistant to imatinib, 608232 (3), Somatic mutation Short stature and advanced bone age, with or without early-onset osteoarthritis and/or osteochondritis dissecans, 165800 (3), ACAN 155760 Autosomal dominant; Spondyloepimetaphyseal dysplasia, aggrecan type, 612813 (3), Autosomal recessive; ?Spondyloepiphyseal dysplasia, Kimberley type, 608361 (3), Autosomal dominant Spondyloenchondrodysplasia with immune dysregulation, 607944 (3), ACP5 171640 Autosomal recessive ACVR1 102576 Fibrodysplasia ossificans progressiva, 135100 (3), Autosomal dominant Weill-Marchesani syndrome 1, recessive, 277600 (3), Autosomal ADAMTS10 608990 recessive Weill-Marchesani 4 syndrome, recessive, 613195 (3), Autosomal ADAMTS17 607511 recessive ADAMTSL2 612277 Geleophysic dysplasia 1, 231050 (3), Autosomal recessive AFF4 604417 CHOPS syndrome, 616368 (3), Autosomal dominant AGA 613228 Aspartylglucosaminuria, 208400 (3), Autosomal recessive Rhizomelic chondrodysplasia punctata, -

Bilateral Hereditary Micro-Epiphyseal Dysplasia – Clinical and Genetic Analysis of a Dutch Family
BILATERAL HEREDITARY MICRO-EPIPHYSEAL DYSPLASIA Clinical and genetic analysis of a Dutch family Bilaterale hereditaire micro-epifysaire dysplasie Klinisch en genetisch onderzoek van een Nederlandse familie (met een samenvatting in het Nederlands) ADRIANUS KLAZINUS MOSTERT Cover design: The author Copy-editing/lay-out: Thea Schenk Printed by: PrintPartners Ipskamp BV, Enschede. © A.K. Mostert, Zwolle, 2003 All rights reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of the holder of the copyright. Mostert, A.K. Bilateral hereditary micro-epiphyseal dysplasia – Clinical and genetic analysis of a Dutch family. Thesis University of Utrecht, with summary in Dutch. ISBN: 90-9016417-0 ii BILATERAL HEREDITARY MICRO-EPIPHYSEAL DYSPLASIA Clinical and genetic analysis of a Dutch family Bilaterale hereditaire micro-epifysaire dysplasie Klinisch en genetisch onderzoek van een Nederlandse familie (met een samenvatting in het Nederlands) PROEFSCHRIFT Ter verkrijging van de graad van doctor aan de Universiteit Utrecht op gezag van de Rector Magnificus, Prof. dr. W.H. Gispen, ingevolge het besluit van het College voor Promoties in het openbaar te verdedigen op maandag 22 september 2003 des middags te 14.30 uur door ADRIANUS KLAZINUS MOSTERT geboren op 30 april 1962 te Winschoten Promotores: Prof. Dr. D. Lindhout, kinderarts-geneticus Prof. Dr. J.R. van Horn, orthopaedisch chirurg Copromotores: Dr. B.R.H. Jansen, orthopaedisch chirurg Prof. Dr. P. Heutink, moleculair geneticus iv Like apples of gold in settings of silver, so is a word spoken at the right moment. -

Skeletal Dysplasia Panel Versie V3 (450 Genen) Centrum Voor Medische Genetica Gent
H9.1-OP2-B40: Genpanel Skeletal dysplasia, in voege op 02/06/2021 Skeletal_dysplasia panel versie v3 (450 genen) Centrum voor Medische Genetica Gent Associated phenotype, OMIM phenotype ID, phenotype Gene OMIM gene ID mapping key and inheritance pattern Hypertrichotic osteochondrodysplasia, 239850 (3), Autosomal dominant; ?Atrial fibrillation, familial, 12, 614050 (3), ABCC9 601439 Autosomal dominant; Cardiomyopathy, dilated, 1O, 608569 (3), Autosomal dominant Leukemia, Philadelphia chromosome-positive, resistant to imatinib, 608232 (3), Somatic mutation; Congenital heart ABL1 189980 defects and skeletal malformations syndrome, 617602 (3), Autosomal dominant Short stature and advanced bone age, with or without early- onset osteoarthritis and/or osteochondritis dissecans, 165800 (3), Autosomal dominant; Spondyloepimetaphyseal dysplasia, ACAN 155760 aggrecan type, 612813 (3), Autosomal recessive; ?Spondyloepiphyseal dysplasia, Kimberley type, 608361 (3), Autosomal dominant Spondyloenchondrodysplasia with immune dysregulation, ACP5 171640 607944 (3), Autosomal recessive Fibrodysplasia ossificans progressiva, 135100 (3), Autosomal ACVR1 102576 dominant Weill-Marchesani syndrome 1, recessive, 277600 (3), ADAMTS10 608990 Autosomal recessive Weill-Marchesani 4 syndrome, recessive, 613195 (3), ADAMTS17 607511 Autosomal recessive ADAMTSL2 612277 Geleophysic dysplasia 1, 231050 (3), Autosomal recessive AFF4 604417 CHOPS syndrome, 616368 (3), Autosomal dominant AGA 613228 Aspartylglucosaminuria, 208400 (3), Autosomal recessive Rhizomelic chondrodysplasia -

Blueprint Genetics Skeletal Dysplasias Core Panel
Skeletal Dysplasias Core Panel Test code: MA3501 Is a 113 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of a skeletal dysplasia. The genes on this panel are included in the Comprehensive Skeletal Dysplasias and Disorders Panel and in the Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders Panel. About Skeletal Dysplasias Core The Skeletal Dysplasias Core Panel is designed to detect mutations responsible for various skeletal dysplasias. Some of the resulting skeletal dysplasias are severe and potentially lethal (such as thanatophoric dysplasia, different types of achondrogenesis and osteogenesis imperfecta type II). Other non-lethal skeletal dysplasias result in disproportionate short stature. Achondroplasia is the most common cause of disproportionate short stature worldwide. It is characterized by rhizomelic shortening of the limbs, exaggerated lumbar lordosis, brachydactyly, and macrocephaly with frontal bossing and midface hypoplasia. Type II collagen defects (mutations in COL2A1 genes) have been identified in a spectrum of disorders ranging from perinatally lethal conditions to those with only mild arthropathy. As many different skeletal dysplasias have similar clinical and radiological findings, multigene panel testing allows for efficient diagnostic testing. Identification of causative mutation(s) establishes the inheritance mode in the family and enables genetic counselling. In addition, identifying the causative mutation(s) provides essential information