LGBT-INCLUSIVE OBSTETRICS and NURSING SUPPORT (L.I.O.N.S.) a Program for Healthcare Providers, Staff, and Students
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Marriage and Family: LGBT Individuals and Same-Sex Couples Marriage and Family: LGBT Individuals and Same-Sex Couples
Marriage and Family: LGBT Individuals and Same-Sex Couples Marriage and Family: LGBT Individuals and Same-Sex Couples Gary J. Gates Summary Though estimates vary, as many as 2 million to 3.7 million U.S. children under age 18 may have a lesbian, gay, bisexual, or transgender parent, and about 200,000 are being raised by same-sex couples. Much of the past decade’s legal and political debate over allowing same-sex couples to marry has centered on these couples’ suitability as parents, and social scientists have been asked to weigh in. After carefully reviewing the evidence presented by scholars on both sides of the issue, Gary Gates concludes that same-sex couples are as good at parenting as their different-sex counterparts. Any differences in the wellbeing of children raised in same-sex and different-sex families can be explained not by their parents’ gender composition but by the fact that children being by raised by same-sex couples have, on average, experienced more family instability, because most children being raised by same-sex couples were born to different-sex parents, one of whom is now in the same-sex relationship. That pattern is changing, however. Despite growing support for same-sex parenting, proportionally fewer same-sex couples report raising children today than in 2000. Why? Reduced social stigma means that more LGBT people are coming out earlier in life. They’re less likely than their LGBT counterparts from the past to have different-sex relationships and the children such relationships produce. At the same time, more same-sex couples are adopting children or using reproductive technologies like artificial insemination and surrogacy. -

A Photo Essay of Transgender Community in the United States
Sexuality Research & Social Policy Journal of NSRC http://nsrc.sfsu.edu December 2007 Vol. 4, No. 4 Momentum: A Photo Essay of the Transgender Community in the United States Over 30 Years, 1978–2007 Mariette Pathy Allen As a photographer, writer, advocate, and ally of the Figure 1. Vicky West (in center of photograph) at the transgender community, I have presented slide shows at hotel swimming pool, New Orleans, Louisiana, 1978. a variety of conferences during the past 30 years. I have varied the slide shows according to the audience and, to challenge myself, asked various questions about my art. What fresh visual connections can I make? How do my newest images relate to earlier series? Shall I focus on indi- vidual heroes and heroines—community leaders—or on dramatic historical events that galvanized people to rethink their lives and demand policy changes? Is it appro- priate to show body images and surgery? Should I focus on youth and relationships? What about speaking of my life as an artist and how it connects to the transgender community? Long before I knowingly met a transgender person, I pondered such questions as, Why are certain character traits assigned to men or to women? and Are these traits in different directions except for one person, Vicky West, immutable or culturally defined? My cultural anthropol- who focused straight back at me. As I peered through the ogy studies offered some theories, but it was not until camera lens, I had the feeling that I was looking at nei- 1978, when I visited New Orleans for Mardi Gras, that I ther a man nor a woman but at the essence of a human came face to face with the opportunity to explore gender being; right then, I decided that I must have this person identity issues through personal experience. -

Transgender Health at the Crossroads: Legal Norms, Insurance Markets, and the Threat of Healthcare Reform
Yale Journal of Health Policy, Law, and Ethics Volume 11 Issue 2 Yale Journal of Health Policy, Law, and Article 4 Ethics 2011 Transgender Health at the Crossroads: Legal Norms, Insurance Markets, and the Threat of Healthcare Reform Liza Khan Follow this and additional works at: https://digitalcommons.law.yale.edu/yjhple Part of the Health Law and Policy Commons, and the Legal Ethics and Professional Responsibility Commons Recommended Citation Liza Khan, Transgender Health at the Crossroads: Legal Norms, Insurance Markets, and the Threat of Healthcare Reform, 11 YALE J. HEALTH POL'Y L. & ETHICS (2011). Available at: https://digitalcommons.law.yale.edu/yjhple/vol11/iss2/4 This Article is brought to you for free and open access by Yale Law School Legal Scholarship Repository. It has been accepted for inclusion in Yale Journal of Health Policy, Law, and Ethics by an authorized editor of Yale Law School Legal Scholarship Repository. For more information, please contact [email protected]. Khan: Transgender Health at the Crossroads NOTE Transgender Health at the Crossroads: Legal Norms, Insurance Markets, and the Threat of Healthcare Reform Liza Khan INTRODUCTION ........................................................................................... 376 I. MEDICALIZED IDENTITY ...................................................................... 379 A. TRANSGENDER HEALTHCARE ..................................... 380 B. TRANSGENDER LAW AND MEDICINE: INTERSECTION OR DISCONNECT?.. 382 C. NEGOTIATING THE MEDICAL CONSTRUCTION OF GENDER: -

Education Policy: Issues Affecting Lesbian, Gay, Bisexual, and Transgender Youth
Education Policy ISSUES AFFECTING LESBIAN, GAY, BISEXUAL, AND TRANSGENDER YOUTH by Jason Cianciotto and Sean Cahill National Gay and Lesbian Task Force Policy Institute Washington, DC 1325 Massachusetts Avenue NW, Suite 600 Washington, DC 20005-4171 Tel 202 393 5177 Fax 202 393 2241 New York, NY 121 West 27th Street, Suite 501 New York, NY 10001 Tel 212 604 9830 Fax 212 604 9831 Los Angeles, CA 5455 Wilshire Boulevard, Suite 1505 Los Angeles, CA 90036 Tel 323 954 9597 Fax 323 954 9454 Cambridge, MA 1151 Massachusetts Avenue Cambridge, MA 02138 Tel 617 492 6393 Fax 617 492 0175 Policy Institute 214 West 29th Street, 5th Floor New York, NY 10001 Tel 212 402 1136 Fax 212 228 6414 [email protected] www.ngltf.org © 2003 The National Gay and Lesbian Task Force Policy Institute When referencing this document, we recommend the following citation: Cianciotto, J., & Cahill, S. (2003). Education policy: Issues affecting lesbian, gay, bisexual, and transgender youth. New York: The National Gay and Lesbian Task Force Policy Institute. The National Gay and Lesbian Task Force Policy Institute is a think tank dedi- cated to research, policy analysis and strategy development to advance greater understanding and equality for lesbian, gay, bisexual and transgender people. Contents PREFACE by Matt Foreman, Executive Director, National Gay and Lesbian Task Force . .vii EXECUTIVE SUMMARY . .1 1. LESBIAN, GAY, BISEXUAL, AND TRANSGENDER YOUTH: A CRITICAL POPULATION . .6 Introduction . .6 Gay Teen Forced to Read Aloud from Bible at School: A Profile of Thomas McLaughlin . .8 Methodological Barriers to Research on LGBT Youth . -

Medical Professionals and Transgender Patient Complications
Indiana University South Bend Undergraduate Research Journal Fear and Discrimination: Medical Professionals and Transgender Patient Complications Written by Steph Foreman Edited by Melanie Peters Abstract: e.g., someone born female whose gender identity is of a woman). I have met professionals who laugh at the idea of transgender Transgender people, just like everyone else, encounter a people and others who say degrading things about transgender variety of medical problems. However, many of the specific people. When I asked an EMT instructor about treating medical complications transgender people face do not emerge in transgender people he told me it would be obvious that they were the same way as they do with cisgender patients. There is an transgender. I knew this was not the case and asked, "What if we immense lack of education for students in medical professions do not know?" The instructor responded that it was their fault and about transgender people and their specific complications. This if they wanted to live then they would tell the EMTs. However, paper will address several transgender patient complications, both one of the prime goals of any medical professional is to make the in emergency care and primary care situations. I will also explain patient, no matter who it is, feel comfortable. Transgender people why, without the necessary training about these complications for know mostly through experience, either their own experience or students going into the medical profession, transgender people that of a friend, that if medical professionals know that they are will continue to receive substandard care and continue to die or be transgender then they could be refused all treatment. -

HIV in Transgender Patients
HIV in Transgender Patients Anita Radix, MD MPH Callen Lorde Community Health Center Learning Objectives At the conclusion of this presentation, participants should be able to: • Adapt and implement HIV prevention strategies for persons of transgender experience • Modify evaluation and treatment approaches to ensure culturally competent delivery of HIV-related health services for your patients Off Label Disclosure This presentation will include discussion of the following non-FDA-approved or investigational uses of products/devices: • Cross gender hormone therapy Case 27 y/o HIV-infected transgender (male-to-female) woman transferring care from California. • 6 months ago CD4 420 cells/mm3 HIV RNA level of 16,000 copies/ml. • ARV naïve • PMH: HIV+ 2005, started CGHT at age 20 • Meds: spironolactone 100mg tid, Premarin 2.5mg bid The Basics • Basic terminology - what does transgender mean? • Gender vs. sexual orientation • What pronoun to use • HIV & Primary care issues • Risks/benefits hormone therapy • Creating a welcoming space Background information Terminology What is gender? 6 Gender vs. Sex Traditional • Gender is binary (M/F) • Synonymous with sex (chromosomes, genitalia) New • Gender is a spectrum • Psychological sense of oneself as male or female • May not match anatomic sex Trans-terminology •Transgender • umbrella term used to group the many gender different communities • people who transcend typical gender paradigms •Transsexual • biological men and women whose gender identity most closely matches the other gender • Sometimes -

Trans Inclusion Policy Manual for Women’S Organizations
Trans Inclusion Policy Manual For Women’s Organizations Julie Darke & Allison Cope for the Women/Trans Dialogue Planning Committee and the Trans Alliance Society Winter 2002 Copyright © 2002 Trans Alliance Society Trans inclusion policy manual for women’s organizations. ISBN 0-9730262-0-0 The contents and design of this manual are the copyright of the Trans Alliance Society and the authors. All rights reserved. You are welcome to reproduce this manual for educational purposes, in whole or in part, but please acknowledge the source. This manual was funded in part by the British Columbia Human Rights Commission (Commission). The manual expresses the views and opinions of the authors and the Project Advisory Team and does not necessarily represent the position or policies of the Commission or its Commissioners. For information on workshops contact: Trans Alliance Society c/o 1170 Bute Street Vancouver, BC, V6E 1Z6 http://www.transalliancesociety.org [email protected] i Table of Contents Acknowledgements . iv Chapter 1: Introduction . 1 Purpose of this Manual . 1 Comments on Language . 2 Implications of Policy Development . 3 Organization of the Manual . 4 Limitations of the Manual . 5 Acknowledgements from the Authors . 6 Chapter 2: Feminism and Transphobia . 8 Chapter 3: Exploring Gender . 17 Defining Gender . 18 Gender and Biology . 21 Gender and the Brain . 26 Gender and Society . 27 Gender Complexity . 30 Chapter 4: The Need for Inclusion . 31 Need for Access to Organizations . 31 Housing . 32 Employment . 34 Health Care . 36 Violence . 41 Understanding Mutual Needs . 44 Chapter 5: Legal Aspects and Human Rights . 46 Legal Aspects of Gender and Sex . -

Representing Trans Road Narratives in Mainstream Cinema (1970-2016)
Wish You Were Here: Representing Trans Road Narratives in Mainstream Cinema (1970-2016) by Evelyn Deshane A thesis presented to the University of Waterloo in fulfilment of the thesis requirement for the degree of Doctor of Philosophy in English Waterloo, Ontario, Canada, 2019 © Evelyn Deshane 2019 Examining Committee Membership The following served on the Examining Committee for this thesis. The decision of the Examining Committee is by majority vote. External Examiner Dr. Dan Irving Associate Professor Supervisor Dr. Andrew McMurry Associate Professor Internal-external Member Dr. Kim Nguyen Assistant Professor Internal Members Dr. Gordon Slethaug Adjunct Professor Dr. Victoria Lamont Associate Professor ii Author’s Declaration I hereby declare that I am the sole author of this thesis. This is a true copy of the thesis, including any required final revisions, as accepted by my examiners. I understand that my thesis may be made electronically available to the public. iii Abstract When Christine Jorgensen stepped off a plane in New York City from Denmark in 1952, she became one of the first instances of trans celebrity, and her intensely popular story was adapted from an article to a memoir and then a film in 1970. Though not the first trans person recorded in history, Jorgensen's story is crucial in the history of trans representation because her journey embodies the archetypal trans narrative which moves through stages of confusion, discovery, cohesion, and homecoming. This structure was solidified in memoirs of the 1950- 1970s, and grew in popularity alongside the booming film industry in the wake of the Hays Production Code, which finally allowed directors, producers, and writers to depict trans and gender nonconforming characters and their stories on-screen. -

LGBT Parents and Their Children Prepared by Melanie L. Duncan M.A
LGBT Parents and their Children Prepared by Melanie L. Duncan M.A. & Kristin E. Joos, Ph.D. University of Florida Distributed by the Sociologists for Women in Society September 2011 Introduction Recently, international groups that advocate on the behalf of LGBT families have declared May 6, 2012 to be International Family Equality Day1. While this day is meant to highlight to increasingly visibility of LGBT families it is also a celebration of the diverse forms that families can take on. This is just one of the many changes that have occurred since the first version of this document was publishes, in 2003. Over the course of the past eight years, six states and Washington D.C. have come to legally recognize same-sex marriages, the Defense of Marriage Act is no longer being enforced, Don‟t Ask Don‟t Tell was repealed, and same-sex couples can now adopt in a number of states, including Florida2. Traditionally, depictions of the family have often centered on the heteronormative nuclear family of mother, father, and child(ren). However, as time has gone on we have seen that family forms have become increasingly diverse and include: single parents, child-free couples, parents who adopt or are foster parents, multiracial couples and their children, stepfamilies, etc. Parents who are lesbian, gay, bisexual, or transgender (LGBT), and their children are contributing to this societal shift that is broadening the traditional and idealized notion of family. The presence of LGBT families in media, courts, and research has grown over the last ten years. What may have been a previously labeled as the “gayby boom3” is now becoming a more commonly recognized by individuals and professionals means of forming a family. -

Social Workers' Attitudes Towards Lesbian, Gay, Bisexual and Transgender Adoptions
California State University, San Bernardino CSUSB ScholarWorks Electronic Theses, Projects, and Dissertations Office of aduateGr Studies 6-2015 SOCIAL WORKERS' ATTITUDES TOWARDS LESBIAN, GAY, BISEXUAL AND TRANSGENDER ADOPTIONS Christina Nicole Kemper California State University - San Bernardino Natalie Jazmin Reynaga California State University - San Bernardino Follow this and additional works at: https://scholarworks.lib.csusb.edu/etd Part of the Social Work Commons Recommended Citation Kemper, Christina Nicole and Reynaga, Natalie Jazmin, "SOCIAL WORKERS' ATTITUDES TOWARDS LESBIAN, GAY, BISEXUAL AND TRANSGENDER ADOPTIONS" (2015). Electronic Theses, Projects, and Dissertations. 149. https://scholarworks.lib.csusb.edu/etd/149 This Thesis is brought to you for free and open access by the Office of aduateGr Studies at CSUSB ScholarWorks. It has been accepted for inclusion in Electronic Theses, Projects, and Dissertations by an authorized administrator of CSUSB ScholarWorks. For more information, please contact [email protected]. SOCIAL WORKERS’ ATTITUDES TOWARDS LESBIAN, GAY, BISEXUAL AND TRANSGENDER ADOPTIONS A Project Presented to the Faculty of California State University, San Bernardino In Partial Fulfillment of the Requirements for the Degree Master of Social Work by Christina Nicole Kemper Natalie Jazmin Reynaga June 2015 SOCIAL WORKERS’ ATTITUDES TOWARDS LESBIAN, GAY, BISEXUAL AND TRANSGENDER ADOPTIONS A Project Presented to the Faculty of California State University, San Bernardino by Christina Nicole Kemper Natalie Jazmin Reynaga June 2015 Approved by: Dr. Erica Lizano, Faculty Supervisor, Social Work Dr. Rosemary McCaslin, M.S.W. Research Coordinator © 2015 Christina Nicole Kemper and Natalie Reynaga ABSTRACT This study explores the attitudes of social workers in relation to lesbian, gay, bisexual and transgender (LGBT) adoptions. -

Bibliography on LGBT Parenting Issues (1983-2009) Brooks, D., & Goldberg, S. (2001). Gay and Lesbian Adoptive and Foster
. Bibliography on LGBT Parenting Issues (1983-2009) Brooks, D., & Goldberg, S. (2001). Gay and lesbian adoptive and foster care placements: Can they meet the needs of waiting children? Families in Society, 46(2), 147-157. Erich, S., Kanenberg, H., Case, H, Allen, T., & Bogdanos, T. (2009). An empirical analysis of factors affecting adolescent attachment in adoptive families with homosexual and straight parents. Children and Youth Services Review, 31, 398-404. Erich, S., Leung, P., Kindle, P. & Carter, S. (2005). Gay and lesbian adoptive families: An exploratory study of family functioning, adoptive child’s behavior, and familial support networks. Journal of Family Social Work, 9, 17-32. Gates, G.J., Badgett, M.V.L., Macomber, J.E., & Chambers, K. (2007). Adoption and foster care by gay and lesbian parents in the United States. Technical report issues jointly by the Williams Institute (Los Angeles) and the Urban Institute (Washington, D.C.) Golombok, S., Spencer, A., & Rutter, M. (1983). Children in lesbian and single-parent households: Psychosexual and psychiatric appraisal. Journal of Child Psychology and Psychiatry, 24(4), 551–572. Golombok, S., & Tasker, F. (1996). Do parents influence the sexual orientation of their children? Findings from a longitudinal study of lesbian families. Developmental Psychology, 32(1), 3–11. Golombok, S., Tasker, F., & Murray, C. (1997). Children raised in fatherless families from infancy: Family relationships and the socioemotional development of children of children of lesbian and single heterosexual mothers. Journal of Child Psychology and Psychiatry 38, 783–791. Golombok, S., Perry, B., Burston, A., Murray, C., Mooney-Somers, J. & Stevens, M. (2003). Children with Lesbian Parents: A Community Study. -
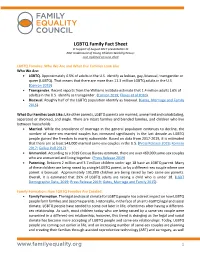
LGBTQ Family Fact Sheet in Support of August 2017 Presentation to NAC Undercount of Young Children Working Group: Last Updated on June 2020
LGBTQ Family Fact Sheet In Support of August 2017 presentation to NAC Undercount of Young Children Working Group: Last Updated on June 2020 LGBTQ Families: Who We Are and What Our Families Look Like Who We Are: • LGBTQ. Approximately 4.5% of adults in the U.S. identify as lesbian, gay, bisexual, transgender or queer (LGBTQ). That means that there are more than 11.3 million LGBTQ adults in the U.S. (Conron 2019). • Transgender. Recent reports from the Williams Institute estimate that 1.4 million adults (.6% of adults) in the U.S. identify as transgender. (Conron 2019; Flores et al 2016). • Bisexual. Roughly half of the LGBTQ population identify as bisexual. (Gates, Marriage and Family 2015). What Our Families Look Like: Like other parents, LGBTQ parents are married, unmarried and cohabitating, separated or divorced, and single. There are intact families and blended families, and children who live between households. • Married. While the prevalence of marriage in the general population continues to decline, the number of same-sex married couples has increased significantly in the last decade as LGBTQ people gained the freedom to marry nationwide. Based on data from 2017-2019, it is estimated that there are at least 543,000 married same-sex couples in the U.S. (Press Release 2019; Romero 2017; Gallup Poll 2017). • Unmarried. According to a 2019 Census Bureau estimate, there are over 469,000 same-sex couples who are unmarried and living together. (Press Release 2019). • Parenting. Between 2 million and 3.7 million children under age 18 have an LGBTQ parent.