CURRICULUM VITAE JEFFREY BRENT, M.D., Ph.D. ACADEMIC
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Safety Oversight Board Members
April 29, 2021 Drug Safety Oversight Board (DSOB) Roster Chair • Douglas Throckmorton, M.D., Deputy Director for Regulatory Programs Center for Drug Evaluation and Research Executive Director • Terry Toigo, R.Ph, MBA Associate Director for Drug Safety Operations, Center for Drug Evaluation and Research Food and Drug Administration Center for Drug Evaluation and Research (CDER) Office of the Center Director (OCD) Primary Member: • Robert Temple, M.D., Deputy Director for Clinical Science Office of New Drugs (OND) Primary Member: • Mary Thanh Hai, M.D., Deputy Director, Office of New Drugs Alternate Members: • Peter Stein, M.D., Director, Office of New Drugs • Ellis Unger, M.D., Director, Office of Office of Cardiology, Hematology, Endocrinology, and Nephrology (OCHEN) Office of Medical Policy (OMP) Primary Member: • Jacqueline Corrigan-Curay, Director Alternate Member: • Leonard V. Sacks, Mgr. Supervisory Medical Officer Office of Generic Drugs (OGD) Primary Member: • Linda Forsyth, M.D., Division of Clinical Review Alternate Member: • Vacant Office of Surveillance and Epidemiology (OSE) Primary Members: • Mark I. Avigan, M.D., Associate Director for Critical Path Initiatives • Judy Zander, M.D., Director, Office of Pharmacoviligance and Epidemiology (OPE) Alternate Members: • Gerald DalPan, M.D., M.H.S., Director, OSE • S. Chris Jones, Deputy Director, Division of Pharmacovigilance (DPV) II • Judy Staffa, Ph.D., R.Ph., Associate Director for Public Health Initiatives -Page 1 of 4- April 29, 2021 • Cynthia LaCivita, R.Ph, Director, Division -
Snake Bite Protocol
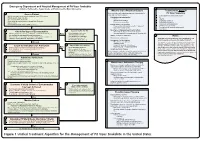
Lavonas et al. BMC Emergency Medicine 2011, 11:2 Page 4 of 15 http://www.biomedcentral.com/1471-227X/11/2 and other Rocky Mountain Poison and Drug Center treatment of patients bitten by coral snakes (family Ela- staff. The antivenom manufacturer provided funding pidae), nor by snakes that are not indigenous to the US. support. Sponsor representatives were not present dur- At the time this algorithm was developed, the only ing the webinar or panel discussions. Sponsor represen- antivenom commercially available for the treatment of tatives reviewed the final manuscript before publication pit viper envenomation in the US is Crotalidae Polyva- ® for the sole purpose of identifying proprietary informa- lent Immune Fab (ovine) (CroFab , Protherics, Nash- tion. No modifications of the manuscript were requested ville, TN). All treatment recommendations and dosing by the manufacturer. apply to this antivenom. This algorithm does not con- sider treatment with whole IgG antivenom (Antivenin Results (Crotalidae) Polyvalent, equine origin (Wyeth-Ayerst, Final unified treatment algorithm Marietta, Pennsylvania, USA)), because production of The unified treatment algorithm is shown in Figure 1. that antivenom has been discontinued and all extant The final version was endorsed unanimously. Specific lots have expired. This antivenom also does not consider considerations endorsed by the panelists are as follows: treatment with other antivenom products under devel- opment. Because the panel members are all hospital- Role of the unified treatment algorithm -

Medical Toxicology Milestone Project
The Medical Toxicology Milestone Project A Joint Initiative of The Accreditation Council for Graduate Medical Education and The American Board of Emergency Medicine July 2015 The Medical Toxicology Milestone Project The Milestones are designed only for use in evaluation of the fellow in the context of their participation in ACGME-accredited residency or fellowship programs. The Milestones provide a framework for assessment of the development of the fellow in key dimensions of the elements of physician competency in a specialty or subspecialty. They neither represent the entirety of the dimensions of the six domains of physician competency, nor are they designed to be relevant in any other context. i Medical Toxicology Milestones Chair: Susanne White, MD Working Group Advisory Group Michele M. Burns, MD, MPH Timothy Brigham, MDiv, PhD Beth Baker, MD Wallace Carter, MD Laura Edgar, EdD, CAE William W. Greaves, MD, MSPH Lewis Nelson, MD Robert Johnson, MD Louis Ling, MD Earl Reisdorff, MD ii Milestone Reporting This document presents milestones designed for programs to use in semi-annual review of fellow performance and reporting to the ACGME. Milestones are knowledge, skills, attitudes, and other attributes for each of the ACGME competencies organized in a developmental framework from less to more advanced. They are descriptors and targets for fellow performance as a fellow moves from entry into fellowship through graduation. In the initial years of implementation, the Review Committee will examine milestone performance data for each program’s fellows as one element in the Next Accreditation System (NAS) to determine whether fellows overall are progressing. For each period, review and reporting will involve selecting milestone levels that best describe a fellow’s current performance and attributes. -

Approach to the Poisoned Patient
PED-1407 Chocolate to Crystal Methamphetamine to the Cinnamon Challenge - Emergency Approach to the Intoxicated Child BLS 08 / ALS 75 / 1.5 CEU Target Audience: All Pediatric and adolescent ingestions are common reasons for 911 dispatches and emergency department visits. With greater availability of medications and drugs, healthcare professionals need to stay sharp on current trends in medical toxicology. This lecture examines mind altering substances, initial prehospital approach to toxicology and stabilization for transport, poison control center resources, and ultimate emergency department and intensive care management. Pediatric Toxicology Dr. James Burhop Pediatric Emergency Medicine Children’s Hospital of the Kings Daughters Objectives • Epidemiology • History of Poisoning • Review initial assessment of the child with a possible ingestion • General management principles for toxic exposures • Case Based (12 common pediatric cases) • Emerging drugs of abuse • Cathinones, Synthetics, Salvia, Maxy/MCAT, 25I, Kratom Epidemiology • 55 Poison Centers serving 295 million people • 2.3 million exposures in 2011 – 39% are children younger than 3 years – 52% in children younger than 6 years • 1-800-222-1222 2011 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System Introduction • 95% decline in the number of pediatric poisoning deaths since 1960 – child resistant packaging – heightened parental awareness – more sophisticated interventions – poison control centers Epidemiology • Unintentional (1-2 -

Medical Toxicology Education in US Emergency
YAJEM-57358; No of Pages 2 American Journal of Emergency Medicine xxx (2018) xxx–xxx Contents lists available at ScienceDirect American Journal of Emergency Medicine journal homepage: www.elsevier.com/locate/ajem Medical toxicology education in US emergency medicine residencies pursuing fellowship while programs with a rotation (elective or manda- tory) reported an average of 1.15 graduates (SD: 1.4; range: 0–7) (p = 0.015). Programs offering a rotation had a statistically significantly Keywords: higher number of TOX faculty than those without (p = 0.008). Emergency medicine Medical toxicology Amongst the 57 programs that did not respond to the survey re- Residency quest, 25 had neither a mandatory or elective rotation listed on their Education website. Only 5 of these programs had at least 1 board certified/eligible medical toxicology faculty. 8 programs offered an elective in medical toxicology and 24 offered a mandatory rotation. Programs with rotation had an average of 1.25 faculty (SD 1.22 and range 0–5). Duration of Medical toxicology (TOX), a core content area of the American Board rotations was: 4 weeks (n = 20; 63%), 3 weeks (n = 3; 9%), 2 weeks of Emergency Medicine [1] and an American Board of Medical Special- (n = 6; 19%), and 1 week (n = 3; 9%). ties (ABMS) recognized subspecialty of Emergency Medicine (EM), We describe the nature of TOX education amongst US-EM-residency Pediatrics, and Preventive Medicine [2] focuses on the “diagnosis, man- programs. agement, and prevention of poisoning and other adverse effects due to We demonstrate a statistically significant difference in the number medications, occupational and environmental toxicants and biological of board-certified TOX faculty and graduates pursuing TOX fellowship agents” [3] The importance of TOX training has long been recognized. -

Snake Bite Prevention What to Do If You Are Bitten
SNAKE BITE PREVENTION It has been estimated that 7,000–8,000 people per year are bitten by venomous snakes in the United States, and for around half a dozen people, these bites are fatal. In 2015, poison centers managed over 3,000 cases of snake and other reptile bites during the summer months alone. Approximately 80% of these poison center calls originated from hospitals and other health care facilities. Venomous snakes found in the U.S. include rattlesnakes, copperheads, cottonmouths/water moccasins, and coral snakes. They can be especially dangerous to outdoor workers or people spending more time outside during the warmer months of the year. Most snakebites occur when people accidentally step on or come across a snake, frightening it and causing it to bite defensively. However, by taking extra precaution in snake-prone environments, many of these bites are preventable by using the following snakebite prevention tips: Avoid surprise encounters with snakes: Snakes tend to be active at night and in warm weather. They also tend to hide in places where they are not readily visible, so stay away from tall grass, piles of leaves, rocks, and brush, and avoid climbing on rocks or piles of wood where a snake may be hiding. When moving through tall grass or weeds, poke at the ground in front of you with a long stick to scare away snakes. Watch where you step and where you sit when outdoors. Shine a flashlight on your path when walking outside at night. Wear protective clothing: Wear loose, long pants and high, thick leather or rubber boots when spending time in places where snakes may be hiding. -

Medical Toxicology Core Content Task Force for the Medical Toxicology Subboard & Julia N
J. Med. Toxicol. (2012) 8:183–191 DOI 10.1007/s13181-012-0223-5 SPECIAL ARTICLE The 2012 Core Content of Medical Toxicology Lewis S. Nelson & Beth A. Baker & Kevin C. Osterhoudt & Curtis P. Snook & The Medical Toxicology Core Content Task Force for the Medical Toxicology Subboard & Julia N. Keehbauch & for the American Board of Emergency Medicine Published online: 30 May 2012 # This article is being published without copyright 2012 Keywords Core content . Medical toxicology. Curriculum Medical Toxicology. The Core Content encompasses the spe- cialty of medical toxicology and outlines the areas of knowl- edge considered essential for the practice of medical toxicology. Functionally, the Core Content provides the orga- Preamble nizational framework for the development of the medical toxicology certification and cognitive expertise examinations, In December 2011, the Medical Toxicology Subboard, com- and details the knowledge to be tested on those examinations, posed of representatives from emergency medicine, pediatrics, beginning with the 2014 examinations. In addition, the Core and preventive medicine, approved a revised Core Content of Content may serve as a template for the development of medical toxicology fellowship curricula. The previous version, 1 Medical Toxicology Subboard Members: Frederick Fung, M.D., initiated in 2000, approved in 2002, and published in 2004, Daniel A. Goldstein, M.D., Rama B. Rao, M.D., Anne-Michelle Ruha, will be retired and replaced by this new version. M.D., and Saralyn R. Williams, M.D. The first Medical Toxicology Core Content was devel- James H. Jones, M.D. (American Board of Emergency Medicine Board oped to assist in the construction of the first examination in Liaison), Julia N. -
![Bites and Stings [Poisonous Animals and Plants]](https://docslib.b-cdn.net/cover/0546/bites-and-stings-poisonous-animals-and-plants-720546.webp)
Bites and Stings [Poisonous Animals and Plants]
Poisonous animals and plants Dr Tim Healing Dip.Clin.Micro, DMCC, CBIOL, FZS, FRSB Course Director, Course in Conflict and Catastrophe Medicine Worshipful Society of Apothecaries of London Faculty of Conflict and Catastrophe Medicine Animal and plant toxins • In most instances the numbers of people affected will be small • There are a few instances where larger numbers may be involved – mainly due to food-borne toxins Poisonous species (N.B. Venomous species use poisons for attack, poisonous animals and plants for passive defence) Venomous and poisonous animals – Reptiles (snakes) – Amphibians (dart frogs) – Arthropods (scorpions, spiders, wasps, bees, centipedes) – Aquatic animals (fish, jellyfish, octopi) Poisonous plants – Contact stinging (nettles, poison ivy, algae) – Poisonous by ingestion (fungi, berries of some plants) – Some algae Snakes Venomous Snakes • About 600 species of snake are venomous (ca. 25% of all snake species). Four main groups: – Elapidae (elapids). Mambas, Cobras, King cobras, Kraits, Taipans, Sea snakes, Brown snakes, Coral snakes. – Viperidae (viperids). True vipers and pit vipers (including Rattlesnakes, Copperheads and Cottonmouths) – Colubridae (colubrids). Mostly harmless, but includes the Boomslang – Atractaspididae (atractaspidids). Burrowing asps, Mole vipers, Stiletto snakes. Geographical distribution • Elapidae: – On land, worldwide in tropical and subtropical regions, except in Europe. – Sea snakes occur in the Indian Ocean and the Pacific • Viperidae: – The Americas, Africa and Eurasia. • Boomslangs -

Venom Week 2012 4Th International Scientific Symposium on All Things Venomous
17th World Congress of the International Society on Toxinology Animal, Plant and Microbial Toxins & Venom Week 2012 4th International Scientific Symposium on All Things Venomous Honolulu, Hawaii, USA, July 8 – 13, 2012 1 Table of Contents Section Page Introduction 01 Scientific Organizing Committee 02 Local Organizing Committee / Sponsors / Co-Chairs 02 Welcome Messages 04 Governor’s Proclamation 08 Meeting Program 10 Sunday 13 Monday 15 Tuesday 20 Wednesday 26 Thursday 30 Friday 36 Poster Session I 41 Poster Session II 47 Supplemental program material 54 Additional Abstracts (#298 – #344) 61 International Society on Thrombosis & Haemostasis 99 2 Introduction Welcome to the 17th World Congress of the International Society on Toxinology (IST), held jointly with Venom Week 2012, 4th International Scientific Symposium on All Things Venomous, in Honolulu, Hawaii, USA, July 8 – 13, 2012. This is a supplement to the special issue of Toxicon. It contains the abstracts that were submitted too late for inclusion there, as well as a complete program agenda of the meeting, as well as other materials. At the time of this printing, we had 344 scientific abstracts scheduled for presentation and over 300 attendees from all over the planet. The World Congress of IST is held every three years, most recently in Recife, Brazil in March 2009. The IST World Congress is the primary international meeting bringing together scientists and physicians from around the world to discuss the most recent advances in the structure and function of natural toxins occurring in venomous animals, plants, or microorganisms, in medical, public health, and policy approaches to prevent or treat envenomations, and in the development of new toxin-derived drugs. -

Long-Term Effects of Snake Envenoming
toxins Review Long-Term Effects of Snake Envenoming Subodha Waiddyanatha 1,2, Anjana Silva 1,2 , Sisira Siribaddana 1 and Geoffrey K. Isbister 2,3,* 1 Faculty of Medicine and Allied Sciences, Rajarata University of Sri Lanka, Saliyapura 50008, Sri Lanka; [email protected] (S.W.); [email protected] (A.S.); [email protected] (S.S.) 2 South Asian Clinical Toxicology Research Collaboration, Faculty of Medicine, University of Peradeniya, Peradeniya 20400, Sri Lanka 3 Clinical Toxicology Research Group, University of Newcastle, Callaghan, NSW 2308, Australia * Correspondence: [email protected] or [email protected]; Tel.: +612-4921-1211 Received: 14 March 2019; Accepted: 29 March 2019; Published: 31 March 2019 Abstract: Long-term effects of envenoming compromise the quality of life of the survivors of snakebite. We searched MEDLINE (from 1946) and EMBASE (from 1947) until October 2018 for clinical literature on the long-term effects of snake envenoming using different combinations of search terms. We classified conditions that last or appear more than six weeks following envenoming as long term or delayed effects of envenoming. Of 257 records identified, 51 articles describe the long-term effects of snake envenoming and were reviewed. Disability due to amputations, deformities, contracture formation, and chronic ulceration, rarely with malignant change, have resulted from local necrosis due to bites mainly from African and Asian cobras, and Central and South American Pit-vipers. Progression of acute kidney injury into chronic renal failure in Russell’s viper bites has been reported in several studies from India and Sri Lanka. Neuromuscular toxicity does not appear to result in long-term effects. -
Snakebite and Spiderbite Clinical Management Guidelines 2013
Guideline Ministry of Health, NSW 73 Miller Street North Sydney NSW 2060 Locked Mail Bag 961 North Sydney NSW 2059 Telephone (02) 9391 9000 Fax (02) 9391 9101 http://www.health.nsw.gov.au/policies/ space space Snakebite and Spiderbite Clinical Management Guidelines 2013 - Third Edition space Document Number GL2014_005 Publication date 17-Mar-2014 Functional Sub group Clinical/ Patient Services - Critical care Clinical/ Patient Services - Medical Treatment Summary Revised clinical resource document which provides information and advise on the management of patients with actual or suspected snakebite or spiderbite, and the appropriate levels, type and location of stored antivenom in NSW health facilities. These are clinical guidelines for best clinical practice which are not mandatory but do provide essential clinical support. Replaces Doc. No. Snakebite & Spiderbite Clinical Management Guidelines 2007 - NSW [GL2007_006] Author Branch Agency for Clinical Innovation Branch contact Agency for Clinical Innovation 9464 4674 Applies to Local Health Districts, Board Governed Statutory Health Corporations, Chief Executive Governed Statutory Health Corporations, Specialty Network Governed Statutory Health Corporations, Affiliated Health Organisations, Community Health Centres, Government Medical Officers, NSW Ambulance Service, Ministry of Health, Private Hospitals and Day Procedure Centres, Public Health Units, Public Hospitals Audience Clinicial Nursing, Medical, Allied Health Staff, Administration, ED, Intensive Care Units Distributed to Public Health System, Divisions of General Practice, Government Medical Officers, Ministry of Health, Private Hospitals and Day Procedure Centres, Tertiary Education Institutes Review date 17-Mar-2019 Policy Manual Patient Matters File No. 12/4133 Status Active Director-General FIVE Spiderbite Guidelines for Assessment and Management Introduction Red-back spider envenoming or latrodectism is Specific features of funnel-web and red back bite are characterised by severe local or regional pain associated discussed below. -

Venomous Snakebites in the United States
CLINICAL REVIEW Venomous Snakebites in the United States Bernard A. Kurecki III, MD, and H. James Brownlee, Jr., MD St. Petersburg, Florida Venomous snakebite treatment is controversial. Venomous snakebites are known to occur in all but a few states. Approximately 10 to 15 individuals die from snake bites each year, with bites from diamondback rattlesnakes accounting for 95 per cent of fatalities. The identification of the two endogenous classes of venomous snakes are discussed in detail to aid in determining the proper treatment for each class. Approximately 25 percent of all pit viper bites are “ dry" and result in no envenomation. The best first aid is a set of car keys to get the victim to a facility where anti- venin is obtainable. Incision and suction should be limited to very special situa tions; cryotherapy and use of tourniquets applied by laymen should be avoided. Proper medical management at a health care facility requires establishing whether envenomation has occurred and to what extent, followed by appropriate dosing of antivenin. The use of corticosteroids and antibiotics is controversial. Tetanus im munization should be updated, if necessary. Although research in developing a more purified antivenin is under way, the best treatment for snakebite is preven tion. venomous snakebite—rarely does any subject draw snakes and refuse treatment in the hope that their religious A more attention and controversy in an emergency de beliefs will effect a cure for the snakebite. partment. Frequently two or more proponents of different Approximately 75 percent of all snakebites occur in treatments may feel the need to defend zealously their people aged between 19 and 30 years, 1 percent to 2 per specific school of thought, and anyone who attempts even cent occur in women, and less than 1 percent occur in the simplest care of a venomous snakebite may be called blacks.