Medicolegal Death Investigation Forensic Pathology: Forensic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Sleuths BEHIND the Scenes for PATHOLOGISTS, the UNUSUAL IS the USUAL
ON THE COVER sleuths BEHIND THE scenes FOR PATHOLOGISTS, THE UNUSUAL IS THE USUAL. BY HOWARD BELL ennifer Boland’s path to pathology began during her sec- ond year of medical school at Washington University in St. Louis. Boland would take study breaks by looking at Jspecimen slides and images, learning to identify them. “Pathology is a visual science. I found it more enjoyable than memorizing notes,” she recalls. After a surgical pathology elective during her clinical rotations, she was hooked. “In medicine it can be hard to find the field you love,” says Boland, who is now a pathologist at Mayo Clinic. “I was lucky enough to find it.” Boland began practicing at Mayo three years ago, after com- pleting a pathology residency as well as pulmonary and surgical pathology fellowships there. She specializes in pulmonary and bone and soft-tissue pathology. Her particular expertise is in lung and chest sarcomas. “They’re a rare and interesting set of tumors,” she says. “Very few are diagnosed in this country each year.” Like many Mayo pathologists, she spends about half her time evaluating specimens from around the world for Mayo Medical Laboratories and the other half evaluating specimens from Mayo patients. Depending on case complexity, she evaluates around 25 to 50 specimens each day. “I like the mystery-solving of pathol- ogy,” she says. Boland is one of 332 pathologists who practice in Minnesota, according to the Minnesota Board of Medical Practice. Often thought of as either white-coated geeks hunched over microscopes or sexy swashbucklers who spend more time solving crimes than analyzing specimens (thanks to TV), pathologists 20 | MINNESOTA MEDICINE | OCTOBER 2014 ON THE COVER OCTOBER 2014 | MINNESOTA MEDICINE | 21 ON THE COVER are sleuths working behind the scenes to ogy, Boland says, adding that many don’t years for neuropathology). -
Views of the Commission Recognizing the Autonomy and Neutrality of Forensic Pathologists
NATIONAL COMMISSION ON FORENSIC SCIENCE Views of the Commission Recognizing the Autonomy and Neutrality of Forensic Pathologists Subcommittee Date of Current Version 13/12/16 Medicolegal Death Investigation Approved by Subcommittee 15/12/16 Status Approved by Commission 09/01/17 Adopted by the Commission Commission Action On January 9, 2017, the Commission voted to adopt this Views Document by a more than two- thirds majority affirmative vote (94% yes, 0% no, 6% abstain). Note: This document reflects the views of the National Commission on Forensic Science, and does not necessarily represent the views of the Department of Justice or the National Institute of Standards and Technology. The portion of the document directly labeled “Views of The Commission” represents the formal Views of the Commission. Information beyond that section is provided for context. Views documents do not request specific action by the Attorney General, and thus do not require further action by the Department of Justice upon their approval by the Commission. The National Commission on Forensic Science is a Federal Advisory Committee established by the Department of Justice. For more information, please visit: https://www.justice.gov/ncfs. Overview Currently, many medicolegal offices do not allow (or they restrict) forensic pathologists (FPs) from performing private work outside of their full-time employment, to include consultative work and/or locum tenens for reasons of alleged conflicts of commitment and/or interest. Because of the national shortage of forensic -

Forensic Sciences Medical Examiner - 20859
State of Alabama Personnel Department 64 North Union Street P. O. Box 304100 Montgomery, AL 36130-4100 Phone: (334) 242-3389 Fax: (334) 242-1110 www.personnel.alabama.gov Continuous Announcement FORENSIC SCIENCES MEDICAL EXAMINER - 20859 Salary: $116,277.60 – 177,266.40 Announcement Date: February 5, 2009 **Effective Thursday, February 5, 2009, this recruitment is being reannounced** JOB INFORMATION The Forensic Sciences Medical Examiner is a permanent full-time position with the Department of Forensic Sciences. Positions are located throughout the state. This is complex professional work in the field of death investigations and forensic pathology. Employees in this class perform complex professional work as physicians, skilled not only in medical and laboratory procedures, but also experienced and knowledgeable in the medicolegal investigation of death. MINIMUM REQUIREMENTS • Graduation from an accredited medical school or osteopathic school • Successful completion of a residency program in anatomic pathology or combined anatomic and clinical pathology program accredited by the American Council for Graduate Medical Education (ACGME) • Preferred board certification in anatomic pathology by the American Board of Pathology • Successful completion of a forensic fellowship program accredited by ACGME. ADDITIONAL REQUIREMENT • Applicants must obtain a valid license to practice medicine or osteopathy in the State of Alabama. Please list all certification and licensing (e.g., license #) information on your application. BENEFITS • Low-Cost Health/Dental -

Curated Materials
PATHOLOGY RESOURCES TO DOWNLOAD Looking for more information or mentorship in Pathology? Send an email to: [email protected] for announcements on future pathology open houses hosted by the APC! QUICK LINKS TO DOWNLOAD: PDF RESOURCES WITH MORE LINKS! • Follow Pathology & Pathologists: www.dropbox.com/s/olq2dvuptrxcgli/Pathology_People%2BOrganizations.pdf?dl=0 • Watch Pathology Videos: www.dropbox.com/s/jor8en7g1y4soaf/Pathology_VideosToWatch.pdf?dl=0 • Free Memberships & Awards: www.dropbox.com/s/6erz3nh2ndngi16/Pathology_StudentOpportunities.pdf?dl=0 OTHER DOWNLOADABLE PDF RESOURCES ABOUT PATHOLOGY • Top 5 Pathology Myth Busted Flier (cap.org) https://documents.cap.org/documents/pathology-five-myths-busted-flier.pdf • Pathology 101 for Medical Students (cap.org) https://documents.cap.org/documents/pathology-101-for-medical-students.pdf • Overview of Anatomic and Clinical Pathology (cap.org) https://documents.cap.org/documents/overview-anatomic-clinical-pathology-medical-students.pdf • The Road to Becoming a Biomedical Physician Scientist (asip.org) www.asip.org/ASIP/assets/file/careers/TheRoad.pdf SALARIES, JOB MARKET, WORKFORCE TRENDS, AND CAREERS IN PATHOLOGY From APC’s Journal – Academic Pathology • Pathology: A Satisfying Medical Profession: journals.sagepub.com/doi/full/10.1177/2374289516661559 • Opportunity: Newly Created Physician-Scientist Research Pathway by the American Board of Pathology: journals.sagepub.com/doi/full/10.1177/2374289516632240 • The Pathology Workforce and Clinical Licensure: The Role of the PhD Clinical Laboratorian in the United States: journals.sagepub.com/doi/full/10.1177/2374289518775948 • Entry of Graduates of US Pathology Residency Programs Into the Workforce: Cohort Data Between 2008 and 2016 Remain Positive and Stable: journals.sagepub.com/doi/10.1177/2374289520901833 From ASCP’s Magazine – The Pathologist • Dr. -
Saundersautopsy.Pdf
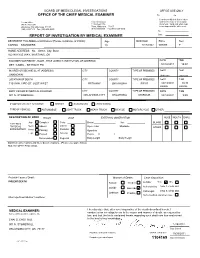
BOARD OF MEDICOLEGAL INVESTIGATIONS OFFICE USE ONLY OFFICE OF THE CHIEF MEDICAL EXAMINER Re Co I hereby certify that this is a true Central Office Eastern Division and correct copy of the original 901 N. Stonewall 1115 West 17th document. Valid only when copy Oklahoma City, Oklahoma 73117 Tulsa, Oklahoma 74107 bears imprint of the office seal. (405) 239-7141 Fax (405) 239-2430 (918) 582-0985 Fax (918) 585-1549 By REPORT OF INVESTIGATION BY MEDICAL EXAMINER Date DECEDENT First-Middle-Last Names (Please avoid use of initials) Age Birth Date Race Sex CARINA SAUNDERS 19 7/17/1992 WHITE F HOME ADDRESS - No. - Street, City, State 922 W KYLE WAY, MUSTANG, OK EXAMINER NOTIFIED BY - NAME - TITLE (AGENCY, INSTITUTION, OR ADDRESS) DATE TIME DET. CADEL - BETHANY PD 10/13/2011 15:07 INJURED OR BECAME ILL AT (ADDRESS) CITY COUNTY TYPE OF PREMISES DATE TIME UNKNOWN Unknown Unknown LOCATION OF DEATH CITY COUNTY TYPE OF PREMISES DATE TIME 7101 NW 23RD ST. JUST WEST BETHANY OKLAHOMA FIELD 10/13/2011 10:30 FOUND FOUND BODY VIEWED BY MEDICAL EXAMINER CITY COUNTY TYPE OF PREMISES DATE TIME 901 N. STONEWALL OKLAHOMA CITY OKLAHOMA MORGUE 10/14/2011 9:00 IF MOTOR VEHICLE ACCIDENT: DRIVER PASSENGER PEDESTRIAN TYPE OF VEHICLE: AUTOMOBILE LIGHT TRUCK HEAVY TRUCK BICYCLE MOTORCYCLE OTHER: DESCRIPTION OF BODY RIGOR LIVOR EXTERNAL OBSERVATION NOSE MOUTH EARS Jaw Complete Color Beard Hair BLOOD EXTERNAL Neck Lateral PHYSICAL Absent Eyes: Color Mustache OTHER EXAMINATION Posterior Arms Passing Opacities Legs Passed Anterior Pupils: R L Decomposed Regional Body Length Body Weight Significant observations and injury documentations - (Please use space below) SEE AUTOPSY PROTOCOL Probable Cause of Death: Manner of Death: Case disposition: VIOLENT DEATH Natural Accident Autopsy Yes No Authorized by CHAI S. -

Forensic Pathology Large Coroner Offices Function Similar to a and the Type of Cases That Will Be Not Just for Popular TV Shows Medical Examiner Office
Victor Weedn forensic pathologists, and in some states, on coroners, who often lack training Health & Medicine ︱ coroners are appointed. Typically, a and need not heed the advice of the coroner is not a licensed physician and medical examiner. cannot perform an autopsy, so they act as medicolegal death investigators – HOW RELEVANT ARE but they retain the legal ability to sign MEDICOLEGAL DEATH the death certificate. All coroners are INVESTIGATIONS TODAY? county-based and most are rural. A few State statutes define the type of system Forensic pathology large coroner offices function similar to a and the type of cases that will be Not just for popular TV shows medical examiner office. investigated. Most deaths are natural and wikipedia.org/wiki/Charles_Norris_(medical_examiner) the patient’s doctor will certify the death Medical examiner’s offices are headed without the need for investigation, but Forensic pathology is one orensic pathology is not your implementation of collapsible steering by board-certified forensic pathologist deaths that are not under the care of a of the most exciting and average medical specialty. Made wheel columns. professionals. Forensic pathology requires physician often require a comprehensive fascinating specialties in all of Fpopular by crime scene investigation Charles Norris was the 1st Chief Medical Examiner more training and education than a family medicolegal death investigation for medicine. Dr Victor W. Weedn, TV shows over the decades, from Quincy, THE ORIGINS OF of the City of New York, in office 1918–1935. practitioner. Medical examiner offices may accurate designation of cause and Chief Medical Examiner for M.E. in the 1970s to Coroner in 2019, the FORENSIC PATHOLOGY be at city, county, regional, or state level. -

61-12-3. Office of Chief Medical Examiner Established; Appointment, Duties, Etc., of Chief Medical Examiner; Assistants and Employees; Promulgation of Rules
11/14/2019 West Virginia Code §61-12-3. Office of chief medical examiner established; appointment, duties, etc., of chief medical examiner; assistants and employees; promulgation of rules. (a) The office of chief medical examiner is hereby established within the division of health in the Department of Health and Human Resources. The office shall be directed by a chief medical examiner, who may employ pathologists, toxicologists, other forensic specialists, laboratory technicians, and other staff members, as needed to fulfill the responsibilities set forth in this article. (b) All persons employed by the chief medical examiner shall be responsible to him or her and may be discharged for any reasonable cause. The chief medical examiner shall specify the qualifications required for each position in the office of chief medical examiner, and each position shall be subject to rules prescribed by the secretary of the Department of Health and Human Resources. (c) The chief medical examiner shall be a physician licensed to practice medicine or osteopathic medicine in the State of West Virginia, who is a diplomat of the American board of pathology in forensic pathology, and who has experience in forensic medicine. The chief medical examiner shall be appointed by the director of the division of health to serve a five-year term unless sooner removed, but only for cause, by the Governor or by the director. (d) The chief medical examiner shall be responsible to the director of the division of health in all matters except that the chief medical examiner shall operate with independent authority for the purposes of: (1) The performance of death investigations conducted pursuant to section eight of this article; (2) The establishment of cause and manner of death; and (3) The formulation of conclusions, opinions or testimony in judicial proceedings. -

Medical Examiners and Coroners
Medical Examiners and Coroners As a medical-legal officer, the coroner or medical examiner is responsible for investigating and certifying specific types of death, and the records produced by these investigations can provide valuable data. Although which deaths are investigated is governed by state law, the types of deaths usually included are:1 • Deaths as a result of an accident, suicide, or homicide • Deaths with unusual or suspicious circumstances • Deaths from disease when “the death occurred suddenly and without warning, the decedent was not being treated by a physician, or the death was unattended”2 Information is collected in different ways in each state, depending on the system in place. For example, a state may have a medical examiner system, a coroner system, or a mixed system. The system may be centralized (controlled by one state office) or decentralized (controlled by county or regional offices). The difference between coroner and medical examiner systems varies by jurisdiction. In addition, the qualifications, skills, and activities of personnel cannot necessarily be determined from the title of the office. However, some differences between coroners and medical examiners may be generalized: • Coroners are usually elected and are not required to be physicians. If an autopsy is needed, a coroner will frequently consult with a pathologist or forensic pathologist. • Medical examiners, in most cases, are appointed and must be physicians. However, they may not be required to have special training in pathology or forensic pathology. Coroner and medical examiner records generally include: • Cause and manner of death • Results of autopsies and laboratory tests for the presence of alcohol or drugs • Circumstances leading to death However, the information collected on suicides and other deaths varies by jurisdiction. -

DUKE UNIVERSITY School of Medicine Pathologists' Assistant
DUKE UNIVERSITY School of Medicine Pathologists’ Assistant Program Department of Pathology Academic Programs The Department of Pathology at Duke University offers a wide array of training programs to fit individual requirements and goals. The Residency Training program is an ACGME approved program and is available as an Anatomic Pathology/Clinical Pathology combined program, a shorter Anatomic Pathology only program, or an Anatomic Pathology/Neuropathology program. Subspecialty fellowships in Cytopathology, Dermatopathology, Hematopathology, Medical Microbiology, and Neuropathology are also ACGME approved. These programs provide the highest quality of graduate medical education by drawing on the depth and breadth of faculty expertise in the Department in all aspects of anatomic and clinical pathology and the availability of a wide variety of often complex clinical cases seen at Duke University Health System. For medical students interested in a career in Pathology predoctoral fellowships, internships and externships are available. Research Training in Experimental pathology can be obtained through Pre- and postdoctoral fellowships of one to five years. All predoctoral fellows are candidates for the Ph.D. degree in pathology. The Ph.D. is optional in postdoctoral programs, which provide didactic and research training in various aspects of modern experimental pathology. A two year NAACLS accredited Pathologists’ Assistant Program leads to a Master of Health Science degree, certifies graduates to sit for the ASCP Board of Certification examination, and leads to exciting career opportunities in a variety of anatomic pathology laboratory settings. Pathologists’ assistants are analogous to physician assistants, but with highly specialized training in autopsy and surgical pathology. This profession was pioneered in the Duke Department of Pathology more than 45 years ago, and is one of only eleven such programs in existence today. -

When Someone Dies
When Someone Dies Even when the passing of someone close to you is not unexpected, the list of tasks can be overwhelming. While we at Eddy & Schein wish you and yours a happy and long life, you may want to keep this list handy. Notifications DOCTOR A doctor is needed to establish the date and time of death and, where possible, the cause. If the person dies in the hospital, the in-hospital doctor automatically does this. If the doctor who is responsible (whether in the hospital or in hospice) suspects the cause of death was other than natural, the doctor is obligated to report it to the police who make a report and will notify the medical examiner. If the doctor does not come to the home, call 911 to report the death and the police and medical examiner will be dispatched. If there is no suspicion that the deceased died of other than natural causes, the body may be released to the funeral home. Otherwise, the body will go to the morgue and an authorized person will have to go to the medical examiner’s office to fill out papers and identify the body. FAMILY, FRIENDS, AND LEGAL REPRESENTATIVES Just after calling the doctor, inform immediate family as well as legal representatives, executors, or trustees, according to the will. People who previously acted as representatives through a Health Care Proxy or a Power of Attorney no longer have that responsibility. Make a list with telephone numbers and think about what you are going to say before you call. -

Department of Pathology
DEPARTMENT OF PATHOLOGY 2017 – 2018 HOUSESTAFF HANDBOOK 300 Pasteur Drive, L235 Stanford, CA 94305 http://pathology.stanford.edu 1 Please use the bookmarks as the Table of Contents 2 Training in Pathology at Stanford Overview The Department of Pathology at Stanford University Medical Center seeks to train outstanding candidates for academic, private practice and other leadership positions in pathology. We offer residency training in Anatomic Pathology (AP), Clinical Pathology (CP), and combined AP and CP (AP/CP). The overall goal of our program is to provide in-depth, flexible training, in all aspects of pathology, leading to board certification in AP, CP or AP/CP. We also offer accredited clinical fellowships in Blood Banking/Transfusion Medicine, Breast Pathology, Cytopathology, Dermatopathology, Gastrointestinal Pathology, Gynecologic Pathology, Hematopathology, Neuropathology, Microbiology, Molecular Genetic Pathology, and Surgical Pathology. Combined AP/Neuropathology is also offered, but must be discussed with the Program Directors and appropriate Fellowship Directors prior to pursuing these training avenues. Trainee Selection All eligible applicants will be considered for training in the Pathology Department at Stanford. Applicants must have one of the following qualifications to be eligible for consideration: ● Graduates of medical schools in the United States and Canada accredited by the Liaison Committee on Medical Education (LCME) ● Graduates of colleges of osteopathic medicine in the United States accredited by the American Osteopathic Association (AOA) ● Graduates of medical schools outside the United States and Canada who have received a currently valid certificate from the Educational Commission for Foreign Medical Graduates or have a full and unrestricted license to practice medicine in a U.S. -

2008 Annual Report OFFICE of the CHIEF MEDICAL EXAMINER
2008 Annual Report OFFICE OF THE CHIEF MEDICAL EXAMINER MAYOR FENTY CONGRATULATES THE OFFICE OF THE CHIEF MEDICAL EXAMINER FOR OBTAINING PROVISIONAL ACCREDITATION FROM THE NATIONAL ASSOCIATION OF MEDICAL EXAMINERS (NAME) The Honorable Adrian M. Fenty, Mayor Neil Albert, City Administrator Government of the District of Columbia Executive Office of the Mayor Marie Lydie Y. Pierre-Louis, MD – Chief Medical Examiner Office of the Chief Medical Examiner DISTRICT OF COLUMBIA OFFICE OF THE CHIEF MEDICAL EXAMINER MISSION: The mission of the Office of the Chief Medical Examiner (OCME), for the District of Columbia, is to investigate and certify all deaths in the District of Columbia that occur by any means of violence (injury), and those that occur without explanation or medical attention, in custody, or which pose a threat to the public health. OCME provides forensic services to government agencies, health care providers and citizens in the Washington D.C. metropolitan area to ensure that justice is served and to improve the health and safety of the public. The Executive Leadership Team Marie-Lydie Y. Pierre-Louis, MD Chief Medical Examiner Sarah M. Colvin, MD Deputy Chief Medical Examiner Beverly A. Fields, Esq. Chief of Staff Lucas W. Zarwell, MFS Deputy Chief Toxicologist Peggy J. Fogg Management Services Officer Anna D. Francis Executive Assistant PRESENTED TO: The Honorable Adrian M. Fenty, Mayor, District of Columbia and The Council of the District of Columbia December 2009 A MESSAGE FROM THE CHIEF MEDICAL EXAMINER Calendar year 2008 was a year of great achievement for the OCME with a major focus on obtaining accreditation by the National Association of Medical Examiners (NAME).