Ocular Syphilis: New Challenges of an Old Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ocular Leishmaniasis Presenting As Chronic
perim Ex en l & ta a l ic O p in l h t C h f Journal of Clinical & Experimental a o l m l a o n l r o g u Ayele et al., J Clin Exp Ophthalmol 2015, 6:1 y o J Ophthalmology ISSN: 2155-9570 DOI: 10.4172/2155-9570.1000395 Case Report Open Access Ocular Leishmaniasis Presenting as Chronic Ulcerative Blepharoconjunctivitis: A Case Report Fisseha Admassu Ayele*, Yared Assefa Wolde, Tesfalem Hagos and Ermias Diro University of Gondar, Gondar, Amhara, Ethiopia *Corresponding author: Fisseha Admassu Ayele MD, University of Gondar, Gondar, Amhara 196, Ethiopia, Tel: 251911197786; E-mail: [email protected] Received date: Dec 01, 2014, Accepted date: Feb 02, 2015, Published date: Feb 05, 2015 Copyright: © 2015 Ayele FH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Leishmaniasis is caused by unicellular eukaryotic obligate intracellular protozoa of the genus Leishmania that is endemic in over 98 countries in the world-most of which are developing countries including Ethiopia. It is transmitted by phlebotomine sandflies. The eye may be affected in cutaneous, mucocutaneous and Post Kala-Azar Dermal Leishmaniasis. We report a case of ocular leishmaniasis with eyelid and conjunctival involvement that had simulated ulcerative blepharoconjunctivitis not responding to conventional antibiotics. The patient was diagnosed by microscopy of a sample obtained via direct smear from the lesions. He was treated with systemic sodium stibogluconate (20 mg/kg/day) for 45 days and was clinically cured with this treatment. -

Syphilis Staging and Treatment Syphilis Is a Sexually Transmitted Disease (STD) Caused by the Treponema Pallidum Bacterium
Increasing Early Syphilis Cases in Illinois – Syphilis Staging and Treatment Syphilis is a sexually transmitted disease (STD) caused by the Treponema pallidum bacterium. Syphilis can be separated into four different stages: primary, secondary, early latent, and late latent. Ocular and neurologic involvement may occur during any stage of syphilis. During the incubation period (time from exposure to clinical onset) there are no signs or symptoms of syphilis, and the individual is not infectious. Incubation can last from 10 to 90 days with an average incubation period of 21 days. During this period, the serologic testing for syphilis will be non-reactive but known contacts to early syphilis (that have been exposed within the past 90 days) should be preventatively treated. Syphilis Stages Primary 710 (CDC DX Code) Patient is most infectious Chancre (sore) must be present. It is usually marked by the appearance of a single sore, but multiple sores are common. Chancre appears at the spot where syphilis entered the body and is usually firm, round, small, and painless. The chancre lasts three to six weeks and will heal without treatment. Without medical attention the infection progresses to the secondary stage. Secondary 720 Patient is infectious This stage typically begins with a skin rash and mucous membrane lesions. The rash may manifest as rough, red, or reddish brown spots on the palms of the hands, soles of the feet, and/or torso and extremities. The rash does usually does not cause itching. Rashes associated with secondary syphilis can appear as the chancre is healing or several weeks after the chancre has healed. -

Diagnostic Code Descriptions (ICD9)
INFECTIONS AND PARASITIC DISEASES INTESTINAL AND INFECTIOUS DISEASES (001 – 009.3) 001 CHOLERA 001.0 DUE TO VIBRIO CHOLERAE 001.1 DUE TO VIBRIO CHOLERAE EL TOR 001.9 UNSPECIFIED 002 TYPHOID AND PARATYPHOID FEVERS 002.0 TYPHOID FEVER 002.1 PARATYPHOID FEVER 'A' 002.2 PARATYPHOID FEVER 'B' 002.3 PARATYPHOID FEVER 'C' 002.9 PARATYPHOID FEVER, UNSPECIFIED 003 OTHER SALMONELLA INFECTIONS 003.0 SALMONELLA GASTROENTERITIS 003.1 SALMONELLA SEPTICAEMIA 003.2 LOCALIZED SALMONELLA INFECTIONS 003.8 OTHER 003.9 UNSPECIFIED 004 SHIGELLOSIS 004.0 SHIGELLA DYSENTERIAE 004.1 SHIGELLA FLEXNERI 004.2 SHIGELLA BOYDII 004.3 SHIGELLA SONNEI 004.8 OTHER 004.9 UNSPECIFIED 005 OTHER FOOD POISONING (BACTERIAL) 005.0 STAPHYLOCOCCAL FOOD POISONING 005.1 BOTULISM 005.2 FOOD POISONING DUE TO CLOSTRIDIUM PERFRINGENS (CL.WELCHII) 005.3 FOOD POISONING DUE TO OTHER CLOSTRIDIA 005.4 FOOD POISONING DUE TO VIBRIO PARAHAEMOLYTICUS 005.8 OTHER BACTERIAL FOOD POISONING 005.9 FOOD POISONING, UNSPECIFIED 006 AMOEBIASIS 006.0 ACUTE AMOEBIC DYSENTERY WITHOUT MENTION OF ABSCESS 006.1 CHRONIC INTESTINAL AMOEBIASIS WITHOUT MENTION OF ABSCESS 006.2 AMOEBIC NONDYSENTERIC COLITIS 006.3 AMOEBIC LIVER ABSCESS 006.4 AMOEBIC LUNG ABSCESS 006.5 AMOEBIC BRAIN ABSCESS 006.6 AMOEBIC SKIN ULCERATION 006.8 AMOEBIC INFECTION OF OTHER SITES 006.9 AMOEBIASIS, UNSPECIFIED 007 OTHER PROTOZOAL INTESTINAL DISEASES 007.0 BALANTIDIASIS 007.1 GIARDIASIS 007.2 COCCIDIOSIS 007.3 INTESTINAL TRICHOMONIASIS 007.8 OTHER PROTOZOAL INTESTINAL DISEASES 007.9 UNSPECIFIED 008 INTESTINAL INFECTIONS DUE TO OTHER ORGANISMS -

2012 Case Definitions Infectious Disease
Arizona Department of Health Services Case Definitions for Reportable Communicable Morbidities 2012 TABLE OF CONTENTS Definition of Terms Used in Case Classification .......................................................................................................... 6 Definition of Bi-national Case ............................................................................................................................................. 7 ------------------------------------------------------------------------------------------------------- ............................................... 7 AMEBIASIS ............................................................................................................................................................................. 8 ANTHRAX (β) ......................................................................................................................................................................... 9 ASEPTIC MENINGITIS (viral) ......................................................................................................................................... 11 BASIDIOBOLOMYCOSIS ................................................................................................................................................. 12 BOTULISM, FOODBORNE (β) ....................................................................................................................................... 13 BOTULISM, INFANT (β) ................................................................................................................................................... -

Understanding Vasculitis Factsheet
Vasculitis - The Facts This factsheet is intended as a simple There is no cure for PSV, but it can usually be introduction to vasculitis for those who have just controlled by use of steroids, chemotherapy and been diagnosed with vasculitis, members of their immune suppressing drugs. Long term drug therapy is family, friends, work colleagues and for others often required. If all goes well some patients go into who may want to know about the disease. “full remission” - ie they no longer need drugs. But relapse is common. What is Vasculitis Vasculitis is a rare inflammatory disease which affects People suffering from vasculitis often experience about 2-3000 new people each year in the UK. muscle weakness and chronic fatigue. Some Vasculitis means inflammation of the blood vessels. experience chronic pain due to nerve damage or Any vessels in any part of the body can be affected. severe migraines and headaches due to damaged blood vessels in the head. There are several different types of vasculitis. In the first type, the acute form, it can be caused by Others require dialysis or kidney transplants. Many infections, reaction to drugs or exposure to chemicals. have breathing problems and others are left with Often the problem is localised, such as a rash. In these permanent physical disabilities. cases the disease usually needs no treatment. Other types of vasculitis can be secondary to (or as a The most “common” types of these rare consequence of) other illnesses such as rheumatoid vasculitis diseases are: arthritis or some types of cancer. ° Granulomatosis with Polyangiitis (GPA) (previously known as Wegener’s Granulomatosis) The third group is known as Primary Systemic ° Eosinophilic Granulomatosis with Polyangiitis (EGPA) Vasculitis (PSV). -

Idiopathic Interstitial Keratitis in a Child 35
Summer 2021 • Vol 16 | No 1 Case report SA Ophthalmology Journal Idiopathic interstitial keratitis in a child 35 Idiopathic interstitial keratitis in a child DA Erasmus MBBCh, MMed, Dip Ophth (SA); Registrar, Department of Neurosciences, Division of Ophthalmology, University of the Witwatersrand, Johannesburg, South Africa ORCID: https://orcid.org/0000-0002-8395-7080 R Höllhumer MBChB, MMed, FC Ophth(SA); Consultant ophthalmologist, Department of Neurosciences, Division of Ophthalmology, University of the Witwatersrand, Johannesburg, South Africa ORCID: https://orcid.org/0000-0002-4375-2224 Corresponding author: Dr DA Erasmus, 40 2nd Avenue, Parktown North, 2193; tel.: +27 76 462 3355; email: [email protected] Abstract Interstitial keratitis represents inflammation and new vessel investigations can help to establish the underlying cause of formation in the middle layers of the cornea without tissue interstitial keratitis. loss. The most important infective aetiologies include herpes viruses, tuberculosis and syphilis. Keywords: interstitial, keratitis, inflammation, cornea, stroma Non-infectious causes such as Cogan’s syndrome should be considered in those cases with associated neurosensory Funding: No external funding was received. hearing loss. The pattern and laterality of inflammation together with the Conflict of interest: The authors have no conflicts of interest presence or absence of systemic features as well as relevant to declare. Severe Mild Moderate Moderate/Mild A * Dry Eye range like NEVER BEFORE Introduction systemic features provides a clue to the a tuberculosis (TB) endemic area such as Interstitial keratitis is a non-ulcerative underlying cause of interstitial keratitis. South Africa. Parasitic infections causing inflammation and subsequent Interstitial keratitis can be broadly interstitial keratitis are very uncommonly vascularisation of the corneal stroma divided into infectious and non-infectious encountered in South Africa but imported which does not primarily involve the aetiologies. -

Immune Defense at the Ocular Surface
Eye (2003) 17, 949–956 & 2003 Nature Publishing Group All rights reserved 0950-222X/03 $25.00 www.nature.com/eye Immune defense at EK Akpek and JD Gottsch CAMBRIDGE OPHTHALMOLOGICAL SYMPOSIUM the ocular surface Abstract vertebrates. Improved visual acuity would have increased the fitness of these animals and would The ocular surface is constantly exposed to a have outweighed the disadvantage of having wide array of microorganisms. The ability of local immune cells and blood vessels at a the outer ocular system to recognize pathogens distance where a time delay in addressing a as foreign and eliminate them is critical to central corneal infection could lead to blindness. retain corneal transparency, hence The first vertebrates were jawless fish that preservation of sight. Therefore, a were believed to have evolved some 470 million combination of mechanical, anatomical, and years ago.1 These creatures had frontal eyes and immunological defense mechanisms has inhabited the shorelines of ancient oceans. With evolved to protect the outer eye. These host better vision, these creatures were likely more defense mechanisms are classified as either a active and predatory. This advantage along with native, nonspecific defense or a specifically the later development of jaws enabled bony fish acquired immunological defense requiring to flourish and establish other habitats. One previous exposure to an antigen and the such habitat was shallow waters where lunged development of specific immunity. Sight- fish made the transition to land several hundred threatening immunopathology with thousand years later.2 To become established in autologous cell damage also can take place this terrestrial environment, the new vertebrates after these reactions. -
Comorbidities in Psoriasis: the Recognition of Psoriasis As a Systemic Disease and Current Management
Review Derleme 71 DOI: 10.4274/turkderm.09476 Turkderm-Turk Arch Dermatol Venereology 2017;51:71-7 Comorbidities in psoriasis: The recognition of psoriasis as a systemic disease and current management Psoriazisde komorbiditeler: Psoriazisin sistemik hastalık olarak kabul edilmesi ve güncel yaklaşım Göknur Kalkan Ankara Yıldırım Beyazıt University Faculty of Medicine, Department of Dermatology, Ankara, Turkey Abstract Psoriasis, with a worldwide prevalence of 2-3%, is now assumed as a systemic chronic inflammatory disease accompanied by comorbidities while it was accepted as a disease limited only to the skin in the past. There are several classifications of the comorbidities which are more common in patients with moderate to severe psoriasis. Simply, comorbidities can be classified as classic, emerging, related to lifestyle, related to treatment. They can also be categorized as medical comorbidities, psychiatric/psychologic comorbidities, and behaviors contributing to medical and psychiatric comorbidities. In this review, providing early diagnosis and treatment of comorbidities, learning screening recommendations for early detection and long-term disease control and improvement in life quality by integrated, multidisciplinary approach were targeted. Keywords: Psoriasis, comorbidity, systemic disease Öz Tüm dünyada %2-3 oranında görülme sıklığına sahip psoriazis, geçmişte sadece deriye sınırlı kabul edilirken, günümüzde birçok komorbiditenin eşlik ettiği kronik sistemik enflamatuvar bir hastalık olarak ele alınmaktadır. Orta-şiddetli düzeyde -

Results of Penetrating Keratoplasty in Syphilitic Interstitial Keratitis
RESULTS OF PENETRATING KERATOPLASTY IN SYPHILITIC INTERSTITIAL KERATITIS GOEGEBUER A.*, ***, AJAY LOHIYA**, ***, CLAERHOUT I.*, KESTELYN PH.* ABSTRACT ratite interstitielle (KI) syphilitique avec ceux dé- crits dans la litérature. Purpose: To compare the results in our patient se- Méthode: Analyse rétrospective des cas, avec acui- ries after penetrating keratoplasty (PKP) for syphi- té visuelle, clarté du greffon, épisodes de rejet, pres- litic interstitial keratitis (IK) with those described in sion intraoculaire et comptage postopératoire des the literature. cellules endothéliales. Methods: Retrospective case series in which visual Résultats: L’acuité visuelle s’est améliorée dans tous acuity (VA), graft clarity,rejection episodes, intraocu- les cas. Il n’y avait pas de signes de déhiscence du lar pressure and endothelial cell density (ECD) were greffon, ni d’ occurrence d’une membrane rétrocor- examined postoperatively. néenne. L’inflammation postopératoire n’était pas Results: Postoperative VA improved in all cases. plus prononcée chez nos patients avec une kératite There was no evidence of wound dehiscense or oc- interstitielle comparée aux patients opérés pour currence of retrocorneal membrane formation in any d’autres raisons. Un déclin normal du comptage des case. Postoperative inflammation was not more se- cellules endothéliales prouvait qu’il n’y avait pas d’in- vere in our patients with syphilitic IK compared to flammation infraclinique. patients undergoing PKP for other reasons. A nor- Conclusion: Une kératoplastie transfixiante pour KI mal decline in ECD proved that there was no sub- syphilitique a un bon pronostic en ce qui concerne clinical inflammation as well. la clarté du greffon. Tous les patients bénéficiaient Conclusion: PKP for syphilitic IK has a good prog- d’ une amélioration de l’acuité visuelle, bien que par- nosis in our case series as far as graft survival is con- fois limitée. -
Successful Treatment with Rituximab in a Patient with TTP Secondary to Severe ANCA-Associated Vasculitis
□ CASE REPORT □ Successful Treatment with Rituximab in a Patient with TTP Secondary to Severe ANCA-Associated Vasculitis Yukari Asamiya 1, Takahito Moriyama 1, Mari Takano 1, Chihiro Iwasaki 1, Kazuo Kimura 1, Yukako Ando 1, Akiko Aoki 1, Kan Kikuchi 2, Takashi Takei 1, Keiko Uchida 1 and Kosaku Nitta 1 Abstract We report a case of thrombotic thrombocytopenic purpura (TTP) secondary to antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis treated by rituximab. TTP secondary to ANCA-associated vasculitis is very rare and has a high mortality rate. We employed rituximab and successfully treated TTP secondary to ANCA-associated vasculitis, because standard therapies, such as steroid therapy, intravenous pulse cyclophos- phamide, and repeated plasma exchange (PE), did not suppress her disease activity. This is the first report to suggest that rituximab can achieve complete remission of TTP secondary to ANCA-associated vasculitis. Key words: ANCA-associated vasculitis, TTP, rituximab, renal failure, intrapulmonary hemorrhage, hemo- dialysis (Inter Med 49: 1587-1591, 2010) (DOI: 10.2169/internalmedicine.49.3135) pies such as steroids and therapeutic PE (4-6). However, ri- Introduction tuximab was employed mainly against idiopathic TTP, and there were few reports discussing treatment of secondary Antineutrophil cytoplasmic antibody (ANCA)-associated TTP; in particular, TTP with ANCA-associated vasculitis vasculitis is recognized as a multisystem autoimmune dis- was rare. Here, we report a patient with TTP secondary to ease characterized by ANCA production and small vessel in- myeloperoxidase-antineutrophil cytoplasmic antibody (MPO- flammation (1). It’s typical clinical manifestations are rap- ANCA) associated vasculitis who was treated using rituxi- idly progressive glomerulonephritis and the occasional de- mab combined with steroid pulse, IVCY and repeated PE. -

Subconjunctival Bevacizumab Injection for Corneal Neovascularization in Interstitial Keratitis
perim Ex en l & ta a l ic O p in l h Journal of Clinical & Experimental t C h f a o l m l a o Thakur et al., J Clin Exp Ophthalmol 2019, 10:2 n l o r g u y o Ophthalmology J DOI: 10.4172/2155-9570.1000797 ISSN: 2155-9570 Case Report Open Access Subconjunctival Bevacizumab Injection for Corneal Neovascularization in Interstitial Keratitis Anchal Thakur, Amit Gupta* and Sabia Handa Department of Ophthalmology, Advanced Eye Centre, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh, India *Corresponding author: Amit Gupta, Department of Ophthalmology, Advanced Eye Centre, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh, India, Tel: 0172 274 7585; E-mail: [email protected] Received date: January 31, 2019; Accepted date: March 19, 2019; Published date: March 26, 2019 Copyright: ©2019 Thakur A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract We describe the use of subconjunctival Bevacizuamb as an adjunct in the treatment of viral interstitial keratitis in a 17-year-old boy. He presented with a 3 months history of gradually progressive diminution of vision. The presenting visual acuity was 20/120 in the right eye and counting fingers close to face in the left eye. Examination revealed bilateral disc shaped stromal edema with leash of blood vessels entering the superior quadrant of the cornea. Subconjunctival injection of 0.1 mL (2.5 mg) of commercially available Bevacizumab (100 mg/4 mL; Avastin) was given under topical anesthesia along with initiation of topical steroids in the form of Betamethasone 0.1%. -
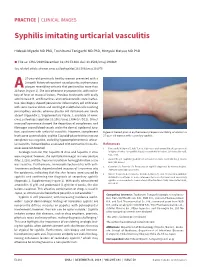
Syphilis Imitating Urticarial Vasculitis
PRACTICE | CLINICAL IMAGES Syphilis imitating urticarial vasculitis Hideaki Miyachi MD PhD, Toshibumi Taniguchi MD PhD, Hiroyuki Matsue MD PhD n Cite as: CMAJ 2019 December 16;191:E1384. doi: 10.1503/cmaj.190469 See related article at www.cmaj.ca/lookup/doi/10.1503/cmaj.191075 27-year-old previously healthy woman presented with a 2-month history of recurrent raised pruritic erythematous plaques resembling urticaria that persisted for more than 24A hours (Figure 1). She was otherwise asymptomatic, with no his- tory of fever or mucosal lesions. Previous treatments with orally administered H1 antihistamines and corticosteroids were ineffec- tive. Skin biopsy showed perivascular inflammatory cell infiltration with some nuclear debris and swelling of endothelial cells involving postcapillary venules, whereas plasma cell infiltration was nearly absent (Appendix 1, Supplementary Figure 1, available at www. cmaj.ca/lookup/suppl/doi:10.1503/cmaj.190469/-/DC1). Direct immunofluorescence showed the deposition of complement and fibrinogen around blood vessels and in the dermal–epidermal junc- tion, consistent with urticarial vasculitis. However, complement Figure 1: Raised pruritic erythematous plaques resembling urticaria in a levels were unremarkable, and the C1q solid-phase test for immune 27-year-old woman with secondary syphilis. complexes was negative, excluding hypocomplementemic urticar- ial vasculitis. Autoantibodies associated with connective tissue dis- References eases were not detected. 1. Tanizaki R, Nichijima T, Aoki T, et al. High-dose oral amoxicillin plus probenecid Serologic tests for HIV, hepatitis B virus and hepatitis C virus is highly effective for syphillis in patients with HIV infection. Clin Infect Dis 2015; 61:177-83. were negative; however, the rapid plasma reagin test was positive (titer, 1:128), and the Treponema pallidum hemagglutination assay 2.