Palmitate Fatty Acid Oxidation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Downloaded from GEO
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Oxylipin metabolism is controlled by mitochondrial b-oxidation during bacterial inflammation. Mariya Misheva1, Konstantinos Kotzamanis1*, Luke C Davies1*, Victoria J Tyrrell1, Patricia R S Rodrigues1, Gloria A Benavides2, Christine Hinz1, Robert C Murphy3, Paul Kennedy4, Philip R Taylor1,5, Marcela Rosas1, Simon A Jones1, Sumukh Deshpande1, Robert Andrews1, Magdalena A Czubala1, Mark Gurney1, Maceler Aldrovandi1, Sven W Meckelmann1, Peter Ghazal1, Victor Darley-Usmar2, Daniel White1, and Valerie B O’Donnell1 1Systems Immunity Research Institute and Division of Infection and Immunity, and School of Medicine, Cardiff University, UK, 2Department of Pathology, University of Alabama at Birmingham, Birmingham, AL 35294, USA, 3Department of Pharmacology, University of Colorado Denver, Aurora, CO 80045, USA, 4Cayman Chemical 1180 E Ellsworth Rd, Ann Arbor, MI 48108, United States, 5UK Dementia Research Institute at Cardiff, Cardiff University, UK Address correspondence: Valerie O’Donnell, [email protected] or Daniel White, [email protected], Systems Immunity Research Institute, Cardiff University *Both authors contributed equally to the study 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -
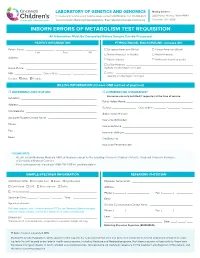
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

Free PDF Download
European Review for Medical and Pharmacological Sciences 2019; 23: 1710-1721 Next-generation sequencing identifies a homozygous mutation in ACADVL associated with pediatric familial dilated cardiomyopathy S.J. CARLUS1, I.S. ALMUZAINI2, M. KARTHIKEYAN3, L. LOGANATHAN3, G.S. AL-HARBI1, A.M. ABDALLAH4, K.M. AL-HARBI1 1Pediatrics Department, Cardiogenetics Unit, College of Medicine, Taibah University, Al-Madinah, Kingdom of Saudi Arabia 2Department of Pediatric Cardiology, Al-Madinah Maternity and Children Hospital (MMCH), Al-Madinah, Kingdom of Saudi Arabia 3Department of Bioinformatics, Alagappa University, Karaikudi, Tamil Nadu, India 4West Midlands Regional Genetics Laboratory, Birmingham Women’s NHS Foundation Trust, Birmingham, United Kingdom Abstract. – OBJECTIVE: Pediatric familial di- Key Words lated cardiomyopathy (DCM) is a rare and se- Pediatric familial dilated cardiomyopathy, Targeted vere heart disease. The genetics of familial DCM gene sequencing, ACADVL, Saudi Arabia, Consanguinity, are complex and include over 100 known dis- Molecular docking, Molecular dynamics. ease-causing genes, but many causative genes are unknown. We aimed to identify the causative gene for DCM in a consanguineous Saudi Ara- bian family with affected family members and a history of sudden death. Introduction PATIENTS AND METHODS: Affected (two chil- dren) and unaffected (one sibling and the mother) Dilated cardiomyopathy (DCM) is a heart family members were screened by next-gener- ation sequencing (NGS) for 181 candidate DCM disease characterized by ventricular dilation and genes and underwent metabolic screening. Fif- impaired myocardial contractility. DCM affects ty-seven clinically annotated controls and 46 DCM 1 in 2500 of the general population and is one of cases were then tested for the identified mutation. -

Ab118182 – Fatty Acid Oxidation Human In-Cell ELISA
ab118182 – Fatty Acid Oxidation Human In-Cell ELISA Kit (ACADVL, ACADM, HADHA) Instructions for Use For measuring in high throughput very long chain specific acyl-CoA dehydrogenase, medium-chain specific acyl-CoA dehydrogenase and long-chain 3-hydroxyl-CoA dehydrogenase This product is for research use only and is not intended for diagnostic use. 1 Table of Contents 1. Introduction 3 2. Assay Summary 6 3. Kit Contents 7 4. Storage and Handling 7 5. Additional Materials Required 8 6. Preparation of Reagents 8 7. Sample Preparation 9 8. Assay Procedure 11 9. Data Analysis 14 10. Assay Performance and Specificity 14 11. Frequently Asked Questions 18 12. Troubleshooting 21 2 1. Introduction Principle: ab118182 uses quantitative immunocytochemistry to measure protein levels or post-translational modifications in cultured cells. Cells are fixed in a microplate and targets of interest are detected with highly specific, well-characterized monoclonal antibodies, and levels are quantified with IRDye®-labeled Secondary Antibodies. IR imaging and quantitation is performed using a LI- COR® Odyssey® or Aerius® system. Background: The Fatty acid B-oxidation (FAO) pathway is a key metabolic pathway that plays an important role in energy homeostasis particularly in organs such as the liver, heart and skeletal muscle. Oxidation of fatty acids occurs inside the mitochondria where acyl-CoA esters (activated fatty acids) of various lengths are shortened into units of acetyl-CoA each time a cycle is fully completed. Each unit of acetyl-CoA is then oxidized by the mitochondria into CO 2 and H 2O via the citric acid cycle and the mitochondria respiratory chain. -

Very Long-Chain Acyl-Coa Dehydrogenase (VLCAD) Deficiency
Very long-chain acyl-CoA dehydrogenase (VLCAD) deficiency What is VLCAD deficiency? VLCAD deficiency is an inherited metabolic disease characterized by lethargy, weakness, and low blood sugar. Individuals with VLCAD deficiency have deficiencies of the very long-chain acyl-CoA dehydrogenase enzyme, which helps to break down very long-chain fatty acids (a type of fat) that are used for energy in cells.1 Symptoms associated with VLCAD deficiency are due to low levels of energy and the toxic build-up of fatty acids in cells, especially in the heart, liver, and muscles.2 What are the symptoms of VLCAD deficiency and what treatment is available? Symptoms of VLCAD deficiency are variable in severity and age at onset, but are typically seen in infancy or early childhood.1 Children with the most severe, early-onset form of VLCAD deficiency are at risk for serious complications such as liver problems and life-threatening heart problems.2 Children or adults with a later-onset form may have intermittent muscle-related or no symptoms.3 Signs and symptoms are often triggered by fasting, illness, or exercise and may include:2,3 • Episodic hypoglycemia (low blood sugar) • Irritability • Lethargy (lack of energy) • Muscle weakness • Cardiomyopathy (abnormal heart muscle) • Abnormal heart rhythms • Hepatomegaly (enlarged liver) • Intermittant rhabdomyolysis (breakdown of muscle tissue) Treatment focuses on prevention of complications and management of symptoms through dietary modifications and avoidance of dehydration and fasting. Acute episodes may be treated with intravenous glucose.2,3 VLCAD deficiency is included in all state newborn screening profiles in the United States.4 How is VLCAD deficiency inherited? VLCAD deficiency is an autosomal recessive disease caused by mutations in the ACADVL gene.1 An individual who inherits one copy of an ACADVL gene mutation is a carrier and is not expected to have related health problems. -
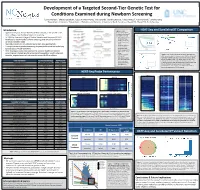
Development of a Targeted Second-Tier Genetic Test For
Development of a Targeted Second-Tier Genetic Test for Conditions Examined during Newborn Screening 1Lonna Mollison, 1Chelsea Gustafson, 1Edgar A Rivera-Munoz, 1Alicia Brandt, 1Daniela DeCristo, 1Falecia Metcalf, 2Cynthia Powell, 1Jonathan Berg 1Department of Genetics, 2Department of Pediatrics and Genetics, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina Introduction Figure 1. Library HEAT-Seq and SureSelectXT Comparison • Approximately four million children are born annually in the United States, preparation workflows for Agilent’s SureSelectXT most undergo state mandated newborn screening and Roche’s HEAT-Seq. A. B. C. • In 2006 the American College of Medical Genetics and Genomics (ACMG) • Time requirement for developed a recommended uniform screening panel (RUSP) to minimize SureSelectXT was about 32 hours, and variability between states for HEAT-Seq about 8 • Most RUSP conditions are detected by tandem mass spectrometry hours. • Recommended DNA • Through the use of genetic sequencing it is possible to detect the underlying input amount for genetic cause of RUSP conditions SureSelectXT was • Here we propose a step-wise approach to enhance traditional newborn about 3000ng, and for HEAT-Seq was about D. screening and integrate genetic screening into population health using cost- 250ng. effective, targeted sequencing to examine current RUSP conditions • Cost per sample for Figure 4. (A-C) The percent of bases at varying read depths for SureSelectXT HEAT-Seq and SureSelect when normalized to 5M reads (A), 50M (including all human reads (B) and 200M reads (C) for each of the 8 samples. (D) The exon baits) was about percent of targeted bases in all samples sequenced at 30 fold Core Condition Associated Gene(s) ACMG Code $333, and for HEAT- coverage were estimated normalizing the data to various values Maple Syrup Urine Disease BCKDHA, BCKDHB, DBT MSUD Seq (including MIPs) of sequenced reads. -

Proteomic and Biochemical Studies of Lysine Malonylation Suggests Its Malonic
MCP Papers in Press. Published on August 28, 2015 as Manuscript M115.048850 Proteomic and biochemical studies of lysine malonylation suggests its malonic aciduria-associated regulatory role in mitochondrial function and fatty acid oxidation Gozde Colak1¶, Olga Pougovkina2¶, Lunzhi Dai1¶, Minjia Tan3, Heleen te Brinke2, He Huang1, Zhongyi Cheng4, Jeongsoon Park5, Xuelian Wan3, Xiaojing Liu6, Wyatt W. Yue7, Ronald J. A. Wanders2,8, Jason W. Locasale6, David B. Lombard5, Vincent C. J. de Boer2,8*, and Yingming Zhao1,3* 1Ben May Department of Cancer Research, University of Chicago, Chicago, IL, 60637, USA 2 Laboratory Genetic Metabolic Diseases, Department of Clinical Chemistry, Academic Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ, Amsterdam, The Netherlands 3State Key Laboratory of Drug Research, Shanghai Institute of Materia Medica, Chinese Academy of Sciences, Shanghai, 201203, P.R. China 4PTM Biolabs, Chicago, IL 60612, USA 5Department of Pathology and Institute of Gerontology, University of Michigan, Ann Arbor, MI 48109, USA 6Division of Nutritional Sciences, Cornell University, Ithaca, NY 14853 7Structural Genomics Consortium, University of Oxford, Oxford OX3 7DQ, UK 8Department of Pediatrics, Emma’s Children Hospital, Academic Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, The Netherlands 1 Copyright 2015 by The American Society for Biochemistry and Molecular Biology, Inc. ¶ Equal contribution. *Correspondence: [email protected], ph: (773) 834-1561 [email protected], ph: -

Download ( 947KB )
Arvind Rajan, Andrea S. Pereyra, Jessica M. Ellis Department of Physiology, Brody School of Medicine, East Carolina Diabetes and Obesity Institute, East Carolina University Determining the Effects of Impaired Muscle Fatty Acid Oxidation on Liver Metabolism Introduction 2. Hepatic Synthesis of Alternative Substrates 5. Effects of Carnitine Supplementation Skeletal muscle plays an extremely critical role in maintaining A. Free Carnitine B. LC-acylcarnitines in Skeletal Muscle C. L-carnitine hepatic synthesis n glucose homeostasis, and is responsible for the majority of 3 +/+ ) Sk LF o ✱ D +/+ i ✱ -/- Sk LF F ✱ s Figure 2. Because whole-body Sk LF n 2.5 ✱ ✱ i +/+ -/- s glucose uptake for energy production. Carnitine +/+ 100000 L Sk HF Sk LF Sk LF e e + t r -/- -/- / +/+ glucose homeostasis is highly ) Sk HF ✱ ✱ + e Sk HF Sk LF p 2.0 o F palmitoyltransferase II (CPT2) is an irreplaceable enzyme for k n ✱ +/+ r 80000 x -/- i 2 L Sk HF S Sk HF t E p regulated by liver metabolism, 14 i + -/- / o 1.5 e n Sk HF t + oxidation of long-chain fatty acids in muscle, converting ✱ g r 60000 v k i u a genes in three main hepatic ✱ d t / S e t a C 1.0 l acylcarnitine into acyl-CoA within the mitochondrial matrix to ✱ z n i o e e 40000 l pathways (GNG: gluconeogenesis, t 1 u e R a r 0.5 o allow for β-oxidation. N m ( F A KG: ketogenesis and β-Oxidation c r 20000 N Defects in CPT2 o n R 0.0 N of fatty acids) were assessed. -

Fatty Acid Oxidation Gene Panel, Varies
NEW TEST Notification Date: February 16, 2021 Effective Date: February 23, 2021 Fatty Acid Oxidation Gene Panel, Varies Test ID: HFAOP Useful for: • Follow up for abnormal biochemical results suggestive of a fatty acid oxidation disorder • Establishing a molecular diagnosis for patients with a fatty acid oxidation disorder • Identifying variants within genes known to be associated with a fatty acid oxidation disorder, allowing for predictive testing of at-risk family members Genetics Information: This test utilizes next-generation sequencing to detect single nucleotide and copy number variants in 44 genes associated with fatty acid oxidation disorders: ACAA2, ACACA, ACAD8, ACAD9, ACADL, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACAT2, ACOT9, ALDH5A1, CPT1A, CPT2, DECR1, ECHS1, ECI1, ETFA, ETFB, ETFDH, ETHE1, FLAD1, GLUD1, HADH, HADHA, HADHB, HMGCL, HMGCS2, HSD17B10, LPIN1, MLYCD, NADK2, OPA1, PPARG, SLC22A5, SLC25A20, SLC25A29, SLC25A32, SLC52A1, SLC52A2, SLC52A3, TANGO2, TAZ. Identification of a pathogenic variant may assist with diagnosis, prognosis, clinical management, familial screening, and genetic counseling for fatty acid oxidation disorders. Additional first-tier testing may be considered/recommended. Methods: Custom Sequence Capture and Targeted Next-Generation Sequencing followed by Polymerase Chain Reaction (PCR) and Sanger Sequencing. Reference Values: An interpretive report will be provided. Specimen Requirements: Specimen Type Whole Blood Preferred: Lavender top (EDTA) or yellow top (ACD) Acceptable: Any anticoagulant Specimen Volume: 3 mL Minimum Volume: 1 mL Specimen Stability Information: Ambient (preferred) / Refrigerated Collection Instructions: 1. Invert several times to mix blood. 2. Send specimen in original tube. © Mayo Foundation for Medical Education and Research. All rights reserved. 1 of 3 Specimen Stability Information: Specimen Type Temperature Time Varies Varies Cautions: Clinical Correlations: Test results should be interpreted in context of clinical findings, family history, and other laboratory data. -

Ab118183 Fatty Acid Oxidation Human Flow Cytometry Kit
Version 3 Last updated 17 January 2019 ab118183 Fatty Acid Oxidation Human Flow Cytometry Kit For the detection of key FAO enzymes (ACADVL, ACADM, HADHA) in live cells by flow cytometry. View kit datasheet: www.abcam.com/ab118183 (use www.abcam.cn/ab118183 for China, or www.abcam.co.jp/ab118183 for Japan) This product is for research use only and is not intended for diagnostic use. Copyright © 2019 Abcam. All rights reserved Table of Contents 1. Overview 1 2. Protocol Summary 4 3. Precautions 5 4. Storage and Stability 5 5. Limitations 6 6. Materials Supplied 6 7. Materials Required, Not Supplied 7 8. Technical Hints 8 9. Reagent Preparation 9 10. Assay Procedure 10 11. Data Analysis 13 12. Typical data 14 13. Assay Performance and Specificity 16 14. Troubleshooting 18 15. FAQs 19 16. Notes 20 Copyright © 2019 Abcam. All rights reserved 1. Overview Fatty Acid Oxidation Human Flow Cytometry Kit (ab118183) is a panel of antibodies against key enzymes of the mitochondrial fatty acid oxidation (FAO), specially designed to be used in flow cytometry. The kit measures the levels of three of the most studied enzymes in the FAO pathway: ACADVL (acyl-CoA dehydrogenase, very long chain specific), ACADM (acyl-CoA dehydrogenase, medium chain specific) and HADHA (long chain 3-hydroxyl-CoA dehydrogenase). The assay combines the power of single cell analysis obtained from flow cytometry with the specificity of antibody-based immunostaining to quantify protein levels in cultured cells. Cells are harvested and fixed/permeabilized in suspension and targets of interest are detected with highly specific monoclonal antibodies, which are detected in turn with fluorescently-labeled secondary antibodies. -

(VLCAD) Deficiency
Very-long-chain acyl-CoA dehydrogenase (VLCAD) deficiency Disorder: VLCAD deficiency is a disorder of fatty acid metabolism with an incidence of 1 in 40,000 to 1 in 120,000 newborns. VLCAD deficiency is an autosomal recessive disorder of fatty acid oxidation (FAOD). This enzyme deficiency results in the inability to catabolize C10-C18 or longer straight- chain fatty acids for energy utilization. VLCAD deficiency may present in the first two years of life after illness or fasting. This inability to break down long chain fatty acids may result in hypoglycemia, lethargy, muscle weakness, cardiomyopathy, and liver disease especially in infants often leading to death. A milder, late-onset form that occurs in older children or adults may present with muscle soreness and exercise-induced rhabdomyolysis. Indications: • Cardiomyopathy, pericardial effusion and/or arrhythmia • Hypoglycemia Additional information and test requisitions are available • Rhabdomyolysis/skeletal myopathy at: www.cchmc.org/molecular-genetics • Abnormal newborn screen suggesting Shipping Instructions VLCAD deficiency Please enclose test requisition with sample. All information must be completed before sample • Abnormal acylcarnitine profile consistent with can be processed. VLCAD deficiency Place samples in styrofoam mailer and ship at room • Presymptomatic testing of at-risk siblings temperature by overnight Federal Express to arrive • Prenatal diagnosis of an at-risk fetus, after Monday through Friday confirmation of biallelic mutations in the parents Ship to: (by prior arrangement only) Cytogenetics and Molecular Genetics Laboratories 3333 Burnet Avenue NRB 1042 • Carrier testing in relative of a patient with Cincinnati, OH 45229 VLCAD deficiency 513-636-4474 Molecular Genetics Laboratory CLIA#: 36D0656333 Phone: (513) 636-4474 Fax: (513) 636-4373 Email: [email protected] Specimen: At least 3 mLs of whole blood in interpretation of the genetic or biochemical test purple/lavender top (EDTA) tube. -

Long-Chain Fatty Acid Oxidation Disorders Biochemical, Pathophysiological and Clinical Aspects
Long-chain fatty acid oxidation disorders biochemical, pathophysiological and clinical aspects Eugène F. Diekman Long-chain fatty acid oxidation disorders - Biochemical, pathophysiological and clinical aspects Eugène Diekman Thesis with a summary in Dutch, Utrecht University ISBN: 978-94-6169-644-1 © Copyright 2015 E.F. Diekman, Utrecht, The Netherlands All rights reserved. No part of this thesis may be reproduced in any form or by any means, electronic, mechanical, by photocopying, recording or otherwhise without prior written permission of the author. The copyrights of the publications remain with the publisher. Cover: Flux -noun- The rate of flow of a fluid, radiant energy, or particles across a given area. (photo: istockphoto.com) Layout and printing: Optima Grafische Communicatie, Rotterdam, the Netherlands Printing of this thesis was financially supported by: Sigma-Tau, Vitaflo, ABN Amro, Gen- zyme, Actelion Long-chain fatty acid oxidation disorders biochemical, pathophysiological and clinical aspects Lange-keten vetzuuroxidatie ziekten biochemische, pathofysiologische en klinische aspecten (met een samenvatting in het Nederlands) Proefschrift ter verkrijging van de graad van doctor aan de Universiteit Utrecht op gezag van de rector magnificus, prof. dr. G.J. van der Zwaan, ingevolge het besluit van het college voor promoties in het openbaar te verdedigen op dinsdag 24 maart 2015 des middags te 2.30 uur door Eugène Franciscus Diekman geboren op 24 oktober 1984 te Deventer Promotoren: Prof.dr. E.E.S. Nieuwenhuis Prof.dr. R.J.A. Wanders