Sunitinib Reversestype-1Immune Suppression and Decreases T-Regulatory Cells in Renal Cell Carcinoma Patients James H
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antitumor Reactivity in Vitro Sorafenib Differentially Affect NK Cell The
The Kinase Inhibitors Sunitinib and Sorafenib Differentially Affect NK Cell Antitumor Reactivity In Vitro This information is current as Matthias Krusch, Julia Salih, Manuela Schlicke, Tina of September 24, 2021. Baessler, Kerstin Maria Kampa, Frank Mayer and Helmut Rainer Salih J Immunol 2009; 183:8286-8294; ; doi: 10.4049/jimmunol.0902404 http://www.jimmunol.org/content/183/12/8286 Downloaded from References This article cites 44 articles, 21 of which you can access for free at: http://www.jimmunol.org/content/183/12/8286.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 24, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2009 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology The Kinase Inhibitors Sunitinib and Sorafenib Differentially Affect NK Cell Antitumor Reactivity In Vitro1 Matthias Krusch,2 Julia Salih,2 Manuela Schlicke,2 Tina Baessler, Kerstin Maria Kampa, Frank Mayer,3 and Helmut Rainer Salih3,4 Sunitinib and Sorafenib are protein kinase inhibitors (PKI) approved for treatment of patients with advanced renal cell cancer (RCC). -

Imatinib-Induced Interstitial Lung Disease and Sunitinib-Associated
CASE Imatinib-induced interstitial lung disease and REPORT sunitinib-associated intra-tumour haemorrhage Herbert H Loong 龍浩鋒 Winnie Yeo 楊明明 An ethnically Chinese patient with newly diagnosed metastatic gastro-intestinal stromal tumour initially treated with imatinib mesylate developed severe interstitial lung disease. As his condition improved after cessation of imatinib mesylate and treatment with corticosteroids, he was started on sunitinib malate. His clinical course was then unfortunately complicated with intra-tumour bleeding. This case report illustrates the dilemmas and complexities associated with treating patients with gastro-intestinal stromal tumours with the new tyrosine kinase inhibitors. Case report A 63-year-old man was referred to our department in January 2007 after being diagnosed with a recurrent gastro-intestinal stromal tumour (GIST). He was initially diagnosed with a duodenal GIST in January 2000 on presenting with symptoms of anaemia. A workup, including upper endoscopy, revealed an ulcerative growth over the third and fourth part of the duodenum. A computed tomographic (CT) scan showed a 4.5 x 5.5 cm soft tissue mass over the same area. A duodenectomy and duodeno-jejunostomy were performed and a pathological examination of tissue removed at surgery confirmed a low-grade GIST (S-100 positive; 4.5 cm in size, mitosis 6/10 high-power field, c-KIT positive). The resection margins were clear so he was managed with routine follow-up and observation. An abdominal ultrasound performed in 2003 showed no evidence of metastases. He remained well until January 2007 when hepatomegaly was found during a physical examination. An abdominal CT scan showed multiple hypervascular tumour foci with cystic changes in both liver lobes. -

The Tyrosine-Kinase Inhibitor Sunitinib Targets Vascular Endothelial (VE)-Cadherin: a Marker of Response to Antitumoural Treatment in Metastatic Renal Cell Carcinoma
www.nature.com/bjc ARTICLE Translational Therapeutics The tyrosine-kinase inhibitor sunitinib targets vascular endothelial (VE)-cadherin: a marker of response to antitumoural treatment in metastatic renal cell carcinoma Helena Polena1, Julie Creuzet1, Maeva Dufies2, Adama Sidibé1, Abir Khalil-Mgharbel1, Aude Salomon1, Alban Deroux3, Jean-Louis Quesada4, Caroline Roelants1, Odile Filhol1, Claude Cochet1, Ellen Blanc5, Céline Ferlay-Segura5, Delphine Borchiellini6, Jean-Marc Ferrero6, Bernard Escudier7, Sylvie Négrier5, Gilles Pages8 and Isabelle Vilgrain1 BACKGROUND: Vascular endothelial (VE)-cadherin is an endothelial cell-specific protein responsible for endothelium integrity. Its adhesive properties are regulated by post-translational processing, such as tyrosine phosphorylation at site Y685 in its cytoplasmic domain, and cleavage of its extracellular domain (sVE). In hormone-refractory metastatic breast cancer, we recently demonstrated that sVE levels correlate to poor survival. In the present study, we determine whether kidney cancer therapies had an effect on VE- cadherin structural modifications and their clinical interest to monitor patient outcome. METHODS: The effects of kidney cancer biotherapies were tested on an endothelial monolayer model mimicking the endothelium lining blood vessels and on a homotypic and heterotypic 3D cell model mimicking tumour growth. sVE was quantified by ELISA in renal cell carcinoma patients initiating sunitinib (48 patients) or bevacizumab (83 patients) in the first-line metastatic setting (SUVEGIL and TORAVA trials). RESULTS: Human VE-cadherin is a direct target for sunitinib which inhibits its VEGF-induced phosphorylation and cleavage on endothelial monolayer and endothelial cell migration in the 3D model. The tumour cell environment modulates VE-cadherin functions through MMPs and VEGF. We demonstrate the presence of soluble VE-cadherin in the sera of mRCC patients (n = 131) which level at baseline, is higher than in a healthy donor group (n = 96). -

Sunitinib Malate)
Prescribing Information Update for SUTENT® (sunitinib malate) July 12, 2010 Dear Health Care Provider: Pfizer Oncology is committed to providing you with up-to-date information about SUTENT® (sunitinib malate) capsules. This letter is to inform you of an important update to the SUTENT prescribing information (PI). The following boxed warning and safety information has been added to the PI for SUTENT: WARNING: HEPATOTOXICITY Hepatotoxicity has been observed in clinical trials and post-marketing experience. This hepatotoxicity may be severe and deaths have been reported. WARNINGS and PRECAUTIONS Hepatotoxicity SUTENT has been associated with hepatotoxicity, which may result in liver failure or death. Liver failure has been observed in clinical trials (7/2281 [0.3%]) and post-marketing experience. Liver failure signs include jaundice, elevated transaminases and/or hyperbilirubinemia in conjunction with encephalopathy, coagulopathy, and/or renal failure. Monitor liver function tests (ALT, AST, bilirubin) before initiation of treatment, during each cycle of treatment, and as clinically indicated. SUTENT should be interrupted for Grade 3 or 4 drug-related hepatic adverse events and discontinued if there is no resolution. Do not restart SUTENT if patients subsequently experience severe changes in liver function tests or have other signs and symptoms of liver failure. Safety in patients with ALT or AST >2.5 × ULN or, if due to liver metastases, >5.0 × ULN has not been established. In addition, the labeling includes a new Medication Guide that your patients will receive when SUTENT is dispensed. Pfizer maintains a global safety database, monitoring all clinical trials and reports of spontaneous adverse events. The incidence of liver failure referenced above is consistent with the very low rate of hepatic failure described in the clinical trials of sunitinib used to support original FDA registration in 2006. -

Mechanism of Myeloid-Derived Suppressor Cell
MECHANISM OF MYELOID-DERIVED SUPPRESSOR CELL ACCUMULATION IN CANCER AND SUSCEPTIBILITY TO REVERSAL BY SUNITINIB by JENNIFER SUSAN KO, M.D. Submitted in partial fulfillment of the requirements For the degree of Doctor of Philosophy Thesis Adviser: Dr. James H. Finke Department of Pathology CASE WESTERN RESERVE UNIVERSITY January, 2010 CASE WESTERN RESERVE UNIVERSITY SCHOOL OF GRADUATE STUDIES We hereby approve the thesis of Jennifer Susan Ko candidate for the Doctor of Philosophy degree*. (signed) Alan Levine Ph.D. David Kaplan M.D., Ph.D. Clark Distelhorst M.D. James Finke Ph.D. Charles Tannenbaum Ph.D. (date) October 12th, 2009 *We also certify that written approval has been obtained for any proprietary material contained therein. 2 TABLE OF CONTENTS Title Page 1 Signature Sheet 2 Table of Contents 3 List of Tables 6 List of Figures 7 Acknowledgements 9 List of Abbreviations 10 Abstract 14 Chapter 1: Introduction 16 Overview: Myeloid-derived suppressor cells in cancer: a novel therapeutic target. 16 Immunotherapy in cancer 16 Myeloid-derived suppressor cells limit immunotherapy 22 Myeloid-derived suppressor cells limit anti-angiogenic therapy 28 Multiple factors are implicated in MDSC formation 30 Vascular Endothelial Growth Factor 30 Stem Cell Factor 32 Granulocyte- and Granulocyte/Monocyte Colony Stimulating Factors 33 S100A9 and Inflammation 34 Intracellular signaling implicated in MDSC programming 36 3 Chapter 2: Sunitinib Mediates Reversal of Myeloid-Derived Suppressor Cell Accumulation in Renal Cell Carcinoma Patients 44 Statement -

(ALK) Rearrangement in Adult Renal Cell Carcinoma with Lung Metastasis: a Case Report and Literature Review
2861 Case Report Anaplastic lymphoma kinase (ALK) rearrangement in adult renal cell carcinoma with lung metastasis: a case report and literature review Shengyu Zhou1, Guanxing Sun2, Jianwei Wang1, Hongtu Zhang1 1Department of Medical Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences (CAMS) and Peking Union Medical College (PUMC), Beijing, China; 2Department of Medical Oncology, Zaozhuang Municipal Hospital, Zaozhuang, China Correspondence to: Shengyu Zhou. Department of Medical Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences (CAMS) and Peking Union Medical College (PUMC), Beijing 100021, China. Email: [email protected]. Abstract: Renal cell carcinoma (RCC) with anaplastic lymphoma kinase (ALK) rearrangement is rare, and the genetic profiles of the tumor have not been elucidated. Here, we report a case with recurrent papillary RCC and lung metastasis after nephrectomy for nearly 7 years. The patient first received sunitinib, whereas the drug toxicity was intolerable. Combined Immunohistology (IHC) and fluorescence in situ hybridization (FISH) revealed the patient has an ALK rearrangement, and the patient then was treated with crizotinib. The patient had good tolerance, and a partial response in the target lesions was achieved. In order to further understand the benefit of crizotinib in ALK-rearranged RCC, the patient was detected with whole exome sequencing (WES) to study her genetic profiles. Compared those of RCC cases without ALK rearrangement (nALK-RCC), the patient and nine RCC cases with ALK rearrangement (ALK-RCC) revealed unique genetic characteristics: 1) The common mutations that occurred in RCC were not found in ALK-RCC.; 2) A total of 11 co-existing mutations in ALK-RCC were found, and they occurred in nALK-RCC at a relatively low frequency. -

Tyrosine Kinase Inhibitors Significantly Improved Survival Outcomes in Patients with Metastatic Gastrointestinal Stromal Tumour: a Multi-Institutional Cohort Study
ORIGINAL ARTICLE Tyrosine kinase inhibitors significantly improved survival outcomes in patients with metastatic gastrointestinal stromal tumour: a multi-institutional cohort study † ‡ A. Deruchie Tan BSc,* K. Willemsma BSc,* A. MacNeill MD, K. DeVries MSc, A. Srikanthan MD MHSc,* ‡ † § C. McGahan MSc, T. Hamilton MD, H. Li BSc,* C.D. Blanke MD, and C.E. Simmons MD MSc* ABSTRACT Background The real-world impact of tyrosine kinase inhibitors (TKIs) in clinical practice for gastrointestinal stromal tumour (GIST) has not been extensively reported. We sought to assess how outcomes have changed over the eras and to evaluate the effect of access to imatinib and sunitinib on survival in patients with unresectable or metastatic GIST in British Columbia. Methods Patients with metastatic or unresectable GIST were allocated to one of three eras: pre-2002, 2002–2007, and post-2007 based on treatment availability (pre-imatinib, post-imatinib, and post-sunitinib). Overall survival (OS) and progression-free survival (PFS) were compared between eras. Univariate and multivariate analyses were performed to determine the effects of tumour, patient, and treatment characteristics on survival outcomes. Results Of 657 patients diagnosed with GIST throughout British Columbia during 1996–2016, 196 had metastatic disease: 23 in the pre-imatinib era, 67 in the post-imatinib era, and 106 in the post-sunitinib era. A significant increase in OS, by 53.6 months (p = 0.0007), and PFS, by 29.1 months (p = 0.044), was observed after the introduction of imatinib. The introduction of sunitinib did not significantly affect OS or PFS. Conclusions Implementation of TKIs has drastically improved survival outcomes for patients with metastatic GIST by up to 4.55 years in the real-world setting. -

Second-Line Treatment for Renal Cell Cancer
British Journal of Cancer (2012) 106, 617 – 618 & 2012 Cancer Research UK All rights reserved 0007 – 0920/12 www.bjcancer.com Editorial Second-line treatment for renal cell cancer ,1 1 1 G Di Lorenzo* , S De Placido and C Buonerba 1Dipartimento di Endocrinologia ed Oncologia Clinica e Molecolare, Universita` Federico II, Napoli, Italy British Journal of Cancer (2012) 106, 617 – 618. doi:10.1038/bjc.2011.611 www.bjcancer.com & 2012 Cancer Research UK In metastatic renal cell carcinoma (mRCC), the transition to the numerically superior to that obtained with second-line sorafenib in targeted therapy era has made available a variety of effective new 52 patients with sunitinib-refractory mRCC by Di Lorenzo et al agents, including vascular endothelial growth factor tyrosine (2009). Importantly, although all of the patients enrolled in the kinase receptor (VEGF-TKR) inhibitors, such as sunitinib, Di Lorenzo trial had received a single agent for metastatic disease, pazopanib, sorafenib; anti-VEGF monoclonal antibody bevacizu- 79% of patients in the RECORD-1 trial had received more than one mab; and mTOR (mammalian target of rapamycin) inhibitors, medication for systemic disease at enrollement, including suniti- everolimus and temsirolimus. A statistically significant improve- nib, sorafenib or interferon. An indirect comparison analysis was ment in progression-free survival (PFS) was obtained with each of performed by matching patients enrolled in these two trials for these six biological drugs in well-conducted phase III trials, in histology, prior treatment, and MSKCC risk score showed that comparison with either interferon alone (in the first-line setting) everolimus was associated with a statistically significant improved or placebo (in the second-line setting). -

Pfizer Oncology Data Presentations at the ESMO 2012 Congress
See Below for Embargo Dates Pfizer Oncology Data Presentations at the ESMO 2012 Congress At the ESMO 2012 Congress, Pfizer Oncology will present the following data: Lung Cancer Presentations Crizotinib: (Abstract #1266P) Poster Session: Retrospective Study of Clinicopathologic Factors Associated with ALK Rearrangement and Survival Outcome in Chinese Patients with NSCLC. Xu-Chao Zhang. Saturday, September 29, 2012. Session Time: 13:00 – 14:00 CEST. Location: Hall XL. (Embargoed until September 17, 2012) (Abstract #1291P) Poster Session: Phase I/II Dose-Finding Study of Crizotinib in Combination with Erlotinib in Patients with Advanced Non-Small Cell Lung Cancer (NSCLC). Sai-Hong Ignatius Ou. Saturday, September 29, 2012. Session Time: 13:00 – 14:00 CEST. Location: Hall XL. (Embargoed until September 17, 2012) (Abstract #1267P) Poster Session: A Large Retrospective Analysis of Pemetrexed Activity in Patients with ALK- Positive Non-Small Cell Lung Cancer (NSCLC) Prior to Crizotinib Treatment. Giorgio V. Scagliotti. Saturday, September 29, 2012. Session Time: 13:00 – 14:00 CEST. Location: Hall XL. (Embargoed until September 17, 2012) (Abstract #1268P) Poster Session: Visual Disturbances in Patients with Anaplastic Lymphoma Kinase (ALK)- Positive Advanced Non-Small Cell Lung Cancer (NSCLC) Treated with Crizotinib. Benjamin Besse. Saturday, September 29, 2012. Session Time: 13:00 – 14:00 CEST. Location: Hall XL. (Embargoed until September 17, 2012) (Abstract #1191PD) Poster Discussion Session: Clinical Activity of Crizotinib in Patients with Advanced Non-Small Cell Lung Cancer (NSCLC) Harboring ROS1 Gene Rearrangement. Sai-Hong Ignatius Ou. Sunday, September 30, 2012. Session Time: 12:45 – 14:15 CEST. Discussion Time: 13:15 CEST. Location: Hall B. -

Protein Kinase Inhibitors for Acute Leukemia Yuan Ling, Qing Xie, Zikang Zhang and Hua Zhang*
Ling et al. Biomarker Research (2018) 6:8 https://doi.org/10.1186/s40364-018-0123-1 REVIEW Open Access Protein kinase inhibitors for acute leukemia Yuan Ling, Qing Xie, Zikang Zhang and Hua Zhang* Abstract Conventional treatments for acute leukemia include chemotherapy, radiation therapy, and intensive combined treatments (including bone marrow transplant or stem cell transplants). Novel treatment approaches are in active development. Recently, protein kinase inhibitors are on clinical trials and offer hope as new drugs for acute leukemia treatment. This review will provide a brief summary of the protein kinase inhibitors in clinical applications for acute leukemia treatment. Keywords: Protein kinase inhibitor, Acute lymphocyte leukemia, Acute myeloid leukemia Background Besides, new inhibitors specific to novel targets like Acute leukemia is subdivided into acute myelocytic IDH1/2, PP2A, DOCK2, PAK1 have been developed leukemia (AML) and acute lymphoblastic leukemia [11]. (ALL) [1, 2]. AML accounts for about 90% of all acute Thus, targeted inhibitors have been developed as re- leukemias in adults, and the cure rates are 35–40% in placements for conventional chemotherapy and provide patients under 60 years old and 5–15% in those over a less toxic and more effective way than the conven- 60 years old respectively [3]. The elderly always have tional chemotherapy. Here, we will provide a compre- poor prognosis with a median survival of 5–10 months. hensive overview of the main protein kinase inhibitors ALL is the most common subtype found in childhood (PKIs) used or being developed in acute leukemia. with a peak incidence in 2–5 years. Although more than 80% of children with ALL receive positive effect after treatments, there are only 20%–40% of adults ALL [4]. -

Fibroblast Growth Factor 2 Regulates Endothelial Cell Sensitivity to Sunitinib
Oncogene (2011) 30, 1183–1193 & 2011 Macmillan Publishers Limited All rights reserved 0950-9232/11 www.nature.com/onc ORIGINAL ARTICLE Fibroblast growth factor 2 regulates endothelial cell sensitivity to sunitinib JC Welti1, M Gourlaouen1, T Powles2, SC Kudahetti2, P Wilson3, DM Berney2 and AR Reynolds1 1Tumour Angiogenesis Group, The Breakthrough Breast Cancer Research Centre, The Institute of Cancer Research, London, UK; 2Centre for Molecular Oncology, Queen Mary University of London, Barts & The London School Of Medicine & Dentistry, Institute of Cancer, John Vane Science Centre, Charterhouse Square, London, UK and 3Department of Medical Oncology, West Smithfield, London, UK The vascular endothelial growth factor (VEGF) receptor variety of human tumours (Ellis and Hicklin, 2008). tyrosine kinase inhibitor sunitinib has been approved for VEGF-A drives angiogenesis by signalling through two first-line treatment of patients with metastatic renal cognate receptors on local endothelial cells, VEGFR1 cancer and is currently being trialled in other cancers. and VEGFR2 (Ferrara et al., 2003; Olsson et al., 2006). However, the effectiveness of this anti-angiogenic agent Binding of VEGF-A to VEGFR2 activates key intra- is limited by the presence of innate and acquired drug cellular signalling molecules including ERK1/2 and resistance. By screening a panel of candidate growth PLCg. Pathways such as these coordinate the biological factors we identified fibroblast growth factor 2 (FGF2) processes necessary for VEGF to induce the formation as a potent regulator of endothelial cell sensitivity to of new vessels (Olsson et al., 2006). sunitinib. We show that FGF2 supports endothelial Numerous inhibitors of the VEGF signalling axis proliferation and de novo tubule formation in the presence have been developed, including the VEGF-neutralising of sunitinib and that FGF2 can suppress sunitinib-induced antibody, bevacizumab, and VEGF receptor tyrosine retraction of tubules. -
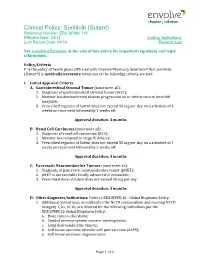
Sunitinib (Sutent) Reference Number: ERX.SPMN.118 Effective Date: 03/14 Coding Implications Last Review Date: 09/16 Revision Log
Clinical Policy: Sunitinib (Sutent) Reference Number: ERX.SPMN.118 Effective Date: 03/14 Coding Implications Last Review Date: 09/16 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Policy/Criteria It is the policy of health plans affiliated with Envolve Pharmacy Solutions® that sunitinib (Sutent®) is medically necessary when one of the following criteria are met: I. Initial Approval Criteria A. Gastrointestinal Stromal Tumor (must meet all): 1. Diagnosis of gastrointestinal stromal tumor (GIST); 2. Member has demonstrated disease progression on or intolerance to imatinib mesylate; 3. Prescribed regimen of Sutent does not exceed 50 mg per day on a schedule of 4 weeks on treatment followed by 2 weeks off. Approval duration: 3 months B. Renal Cell Carcinoma (must meet all): 1. Diagnosis of renal cell carcinoma (RCC); 2. Member has relapsed or stage IV disease; 3. Prescribed regimen of Sutent does not exceed 50 mg per day on a schedule of 4 weeks on treatment followed by 2 weeks off. Approval duration: 3 months C. Pancreatic Neuroendocrine Tumors (must meet all): 1. Diagnosis of pancreatic neuroendocrine tumor (pNET); 2. pNET is unresectable locally advanced or metastatic; 3. Prescribed dose of Sutent does not exceed 50 mg per day. Approval duration: 3 months D. Other diagnoses/indications: Refer to ERX.SPMN.16 - Global Biopharm Policy. 1. Additional Sutent uses, as outlined in the NCCN compendium and meeting NCCN category 1, 2a, or 2b, are covered for the following indications per the ERX.SPMN.16 Global Biopharm Policy: a. Bone cancer- chordoma; b.