APC Clindoc 036]
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table 2. 2012 AGS Beers Criteria for Potentially
Table 2. 2012 AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults Strength of Organ System/ Recommendat Quality of Recomm Therapeutic Category/Drug(s) Rationale ion Evidence endation References Anticholinergics (excludes TCAs) First-generation antihistamines Highly anticholinergic; Avoid Hydroxyzin Strong Agostini 2001 (as single agent or as part of clearance reduced with e and Boustani 2007 combination products) advanced age, and promethazi Guaiana 2010 Brompheniramine tolerance develops ne: high; Han 2001 Carbinoxamine when used as hypnotic; All others: Rudolph 2008 Chlorpheniramine increased risk of moderate Clemastine confusion, dry mouth, Cyproheptadine constipation, and other Dexbrompheniramine anticholinergic Dexchlorpheniramine effects/toxicity. Diphenhydramine (oral) Doxylamine Use of diphenhydramine in Hydroxyzine special situations such Promethazine as acute treatment of Triprolidine severe allergic reaction may be appropriate. Antiparkinson agents Not recommended for Avoid Moderate Strong Rudolph 2008 Benztropine (oral) prevention of Trihexyphenidyl extrapyramidal symptoms with antipsychotics; more effective agents available for treatment of Parkinson disease. Antispasmodics Highly anticholinergic, Avoid Moderate Strong Lechevallier- Belladonna alkaloids uncertain except in Michel 2005 Clidinium-chlordiazepoxide effectiveness. short-term Rudolph 2008 Dicyclomine palliative Hyoscyamine care to Propantheline decrease Scopolamine oral secretions. Antithrombotics Dipyridamole, oral short-acting* May -

Appendix A: Potentially Inappropriate Prescriptions (Pips) for Older People (Modified from ‘STOPP/START 2’ O’Mahony Et Al 2014)
Appendix A: Potentially Inappropriate Prescriptions (PIPs) for older people (modified from ‘STOPP/START 2’ O’Mahony et al 2014) Consider holding (or deprescribing - consult with patient): 1. Any drug prescribed without an evidence-based clinical indication 2. Any drug prescribed beyond the recommended duration, where well-defined 3. Any duplicate drug class (optimise monotherapy) Avoid hazardous combinations e.g.: 1. The Triple Whammy: NSAID + ACE/ARB + diuretic in all ≥ 65 year olds (NHS Scotland 2015) 2. Sick Day Rules drugs: Metformin or ACEi/ARB or a diuretic or NSAID in ≥ 65 year olds presenting with dehydration and/or acute kidney injury (AKI) (NHS Scotland 2015) 3. Anticholinergic Burden (ACB): Any additional medicine with anticholinergic properties when already on an Anticholinergic/antimuscarinic (listed overleaf) in > 65 year olds (risk of falls, increased anticholinergic toxicity: confusion, agitation, acute glaucoma, urinary retention, constipation). The following are known to contribute to the ACB: Amantadine Antidepressants, tricyclic: Amitriptyline, Clomipramine, Dosulepin, Doxepin, Imipramine, Nortriptyline, Trimipramine and SSRIs: Fluoxetine, Paroxetine Antihistamines, first generation (sedating): Clemastine, Chlorphenamine, Cyproheptadine, Diphenhydramine/-hydrinate, Hydroxyzine, Promethazine; also Cetirizine, Loratidine Antipsychotics: especially Clozapine, Fluphenazine, Haloperidol, Olanzepine, and phenothiazines e.g. Prochlorperazine, Trifluoperazine Baclofen Carbamazepine Disopyramide Loperamide Oxcarbazepine Pethidine -

Hypersalivation in Children and Adults
Pharmacological Management of Hypersalivation in Children and Adults Scope: Adult patients with Parkinson’s disease, children with neurodisability, cerebral palsy, long-term ventilation with drooling, and drug-induced hypersalivation. ASSESSMENT OF SEVERITY/RESPONSE TO TREATMENT: Severity of drooling can be assessed subjectively via discussion with patients and their carers/parents and by observation. Amount of drooling can be quantified by measuring the number of bibs required per day and this can also be graded using the Thomas-Stonell and Greenberg scale: • 1 = Dry (no drooling) • 2 = Mild (moist lips) • 3 = Moderate (wet lips and chin) • 4 = Severe (damp clothing) CONSIDERATIONS FOR PRESCRIBING/TITRATION No evidence to support the use of one particular treatment over another. Drug choice is to be determined by individual patient factors. When prescribing/titrating antimuscarinic drugs to treat hypersalivation always take account of: • Coexisting conditions (for example, history of urinary retention, constipation, glaucoma, dental issues, reflux etc.) • Use of other existing medication affecting the total antimuscarinic burden • Risk of adverse effects Titrate dose upward until the desired level of dryness, side effects or maximum dose reached. Take into account the preferences of the patients and their carers/ parents, and the age range and indication covered by the marketing authorisations (see individual summaries of product characteristics, BNF or BNFc for full prescribing information). FIRST LINE DRUG TREATMENT OPTIONS FOR ADULTS -
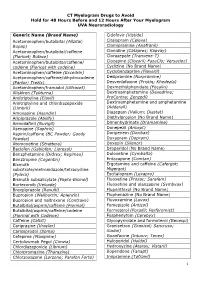
CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology
CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology Generic Name (Brand Name) Cidofovir (Vistide) Acetaminophen/butalbital (Allzital; Citalopram (Celexa) Bupap) Clomipramine (Anafranil) Acetaminophen/butalbital/caffeine Clonidine (Catapres; Kapvay) (Fioricet; Butace) Clorazepate (Tranxene-T) Acetaminophen/butalbital/caffeine/ Clozapine (Clozaril; FazaClo; Versacloz) codeine (Fioricet with codeine) Cyclizine (No Brand Name) Acetaminophen/caffeine (Excedrin) Cyclobenzaprine (Flexeril) Acetaminophen/caffeine/dihydrocodeine Desipramine (Norpramine) (Panlor; Trezix) Desvenlafaxine (Pristiq; Khedezla) Acetaminophen/tramadol (Ultracet) Dexmethylphenidate (Focalin) Aliskiren (Tekturna) Dextroamphetamine (Dexedrine; Amitriptyline (Elavil) ProCentra; Zenzedi) Amitriptyline and chlordiazepoxide Dextroamphetamine and amphetamine (Limbril) (Adderall) Amoxapine (Asendin) Diazepam (Valium; Diastat) Aripiprazole (Abilify) Diethylpropion (No Brand Name) Armodafinil (Nuvigil) Dimenhydrinate (Dramamine) Asenapine (Saphris) Donepezil (Aricept) Aspirin/caffeine (BC Powder; Goody Doripenem (Doribax) Powder) Doxapram (Dopram) Atomoxetine (Strattera) Doxepin (Silenor) Baclofen (Gablofen; Lioresal) Droperidol (No Brand Name) Benzphetamine (Didrex; Regimex) Duloxetine (Cymbalta) Benztropine (Cogentin) Entacapone (Comtan) Bismuth Ergotamine and caffeine (Cafergot; subcitrate/metronidazole/tetracycline Migergot) (Pylera) Escitalopram (Lexapro) Bismuth subsalicylate (Pepto-Bismol) Fluoxetine (Prozac; Sarafem) -

A Brief Overview of Psychotropic Medication Use for Persons with Intellectual Disabilities
A BRIEF OVERVIEW OF PSYCHOTROPIC MEDICATION USE FOR PERSONS WITH INTELLECTUAL DISABILITIES INTRODUCTION Individuals with intellectual disabilities are not uncommonly prescribed psychotropic medications. Too often, historically, such agents have been used to try to improve behavioral control without adequate understanding of the antecedents, purpose, and reinforcement of the problematic behavior. While an individual with an intellectual disability may experience a depressive, anxiety, or psychotic disorder in the more typical sense some individuals experience a pattern of anxiety/alarm/arousal leading to affective dysregulation and impulsive behavior. The anxiety can be stimulated by environmental change, physical discomfort, cues related to past trauma, overstimulation, boredom, confusion, or other unpleasant states. Addressing what is causing the distress or reinforcing the behavioral response is the most important thing (though not always easy). Psychotropic medications may be useful for treating more typically presenting psychiatric illnesses as well as being part of more comprehensive plans to attenuate risk behaviors. An individual with intellectual disabilities who seems sad, is withdrawn, shows low energy and lack of interest, is eating or sleeping more or less, or may be more irritable could be suffering from a depression that needs medication treatment. On the other hand an individual with intellectual disabilities who demonstrates aggression, property destruction, self-injury, or other forms of “dyscontrol” may be helped by medication aimed at blunting the anxiety/alarm and/or blocking its escalation into aggression or other dangerous behaviors. In such instances the medications are just part of an overall strategy or plan to help the individual avoid the “need” to engage in such behavior. -
The Use and Potential Abuse of Anticholinergic
British Journal of Clinical DOI:10.1111/j.1365-2125.2008.03342.x Pharmacology Correspondence Dr Pål Gjerden, Department of Psychiatry, The use and potential abuse Telemark Hospital, N-3710 Skien, Norway. Tel: + 47 3500 3476 Fax: + 47 3500 3187 of anticholinergic E-mail: [email protected] ---------------------------------------------------------------------- antiparkinson drugs in Keywords adverse effects, anticholinergic agents, antiparkinson agents, antipsychotic Norway: a agents, drug abuse ---------------------------------------------------------------------- Received pharmacoepidemiological 9 June 2008 Accepted 18 October 2008 study Published Early View 16 December 2008 Pål Gjerden, Jørgen G. Bramness1 & Lars Slørdal2 Department of Psychiatry,Telemark Hospital, Skien, 1Department of Pharmacoepidemiology, Norwegian Institute of Public Health, Oslo and 2Department of Laboratory Medicine, Children’s and Women’s Health, Norwegian University of Science and Technology,Trondheim, Norway WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT • Anticholinergic antiparkinson drugs are used to ameliorate extrapyramidal AIMS symptoms caused by either Parkinson’s The use of anticholinergic antiparkinson drugs is assumed to have disease or antipsychotic drugs, but their use shifted from the therapy of Parkinson’s disease to the amelioration in the treatment of Parkinson’s disease is of extrapyramidal adverse effects induced by antipsychotic drugs. There is a considerable body of data suggesting that anticholinergic assumed to be in decline. antiparkinson drugs have a potential for abuse.The aim was to • Patients with psychotic conditions have a investigate the use and potential abuse of this class of drugs in Norway. high prevalence of abuse of drugs, including anticholinergic antiparkinson drugs. METHODS Data were drawn from the Norwegian Prescription Database on sales to a total of 73 964 patients in 2004 of biperiden and orphenadrine, and use in patients with Parkinson’s disease or in patients who were WHAT THIS STUDY ADDS also prescribed antipsychotic agents. -

CENTRAL NERVOUS SYSTEM DEPRESSANTS Opioid Pain Relievers Anxiolytics (Also Belong to Psychiatric Medication Category) • Codeine (In 222® Tablets, Tylenol® No
CENTRAL NERVOUS SYSTEM DEPRESSANTS Opioid Pain Relievers Anxiolytics (also belong to psychiatric medication category) • codeine (in 222® Tablets, Tylenol® No. 1/2/3/4, Fiorinal® C, Benzodiazepines Codeine Contin, etc.) • heroin • alprazolam (Xanax®) • hydrocodone (Hycodan®, etc.) • chlordiazepoxide (Librium®) • hydromorphone (Dilaudid®) • clonazepam (Rivotril®) • methadone • diazepam (Valium®) • morphine (MS Contin®, M-Eslon®, Kadian®, Statex®, etc.) • flurazepam (Dalmane®) • oxycodone (in Oxycocet®, Percocet®, Percodan®, OxyContin®, etc.) • lorazepam (Ativan®) • pentazocine (Talwin®) • nitrazepam (Mogadon®) • oxazepam ( Serax®) Alcohol • temazepam (Restoril®) Inhalants Barbiturates • gases (e.g. nitrous oxide, “laughing gas”, chloroform, halothane, • butalbital (in Fiorinal®) ether) • secobarbital (Seconal®) • volatile solvents (benzene, toluene, xylene, acetone, naptha and hexane) Buspirone (Buspar®) • nitrites (amyl nitrite, butyl nitrite and cyclohexyl nitrite – also known as “poppers”) Non-Benzodiazepine Hypnotics (also belong to psychiatric medication category) • chloral hydrate • zopiclone (Imovane®) Other • GHB (gamma-hydroxybutyrate) • Rohypnol (flunitrazepam) CENTRAL NERVOUS SYSTEM STIMULANTS Amphetamines Caffeine • dextroamphetamine (Dexadrine®) Methelynedioxyamphetamine (MDA) • methamphetamine (“Crystal meth”) (also has hallucinogenic actions) • methylphenidate (Biphentin®, Concerta®, Ritalin®) • mixed amphetamine salts (Adderall XR®) 3,4-Methelynedioxymethamphetamine (MDMA, Ecstasy) (also has hallucinogenic actions) Cocaine/Crack -

Georgia State Forensic Drugs
Comprehensive Forensic FT-IR Collection Library Listing – 4,286 spectra This extensive library contains materials not only of forensic interest but also for general problem solving and identification of unknown substances in industry and academia. The wide range of items include drugs, clandestine lab chemicals, explosives, paints, fabrics, dyes, polymers, inorganic compounds, pigments, adhesives, and other common materials. The library consists of 4,286 spectra that were acquired from a wide range of laboratories involved in forensic investigations. The collection includes the following classes of compounds: • Drugs of abuse, scheduled materials • Pharmaceuticals, vitamins and excipients • Clandestine lab materials and intermediates • Solvents, organic chemicals and hazardous chemicals • Accelerants • Lubricants and natural oils • Explosives, pyrotechnics, primers, powders and boosters • Herbal and plant material and fibers • Automobile paint vehicles, pigments, primers and clear coats • Textiles, natural and man-made fibers, carpet materials • Paints, coatings, varnishes, oils • Dyes and stains • Polymers, monomers, copolymers, plasticizers and rubbers • Inorganics, pigments, minerals and clays • Tape, adhesives, sealants, glues, caulks and putties • Crystal test derivatives and intermediates • Household chemicals, cleaning agents, surfactants and pesticide All spectra were measured using micro or macro Diamond ATR, thin films on salt windows or KBr pellets at 4 cm-1 spectral resolution. Comprehensive Forensic FT-IR Collection Index -

DRUG TREATMENTS for Parkinson's
DRUG TREATMENTS FOR Parkinson’s 1 There is no cure yet for Parkinson’s but there are The content in this booklet is designed to be dipped in and out many different drugs that can of – don’t feel like you need to help manage the symptoms. read everything in one go. This is particularly true because what This booklet is for people works for you when starting with Parkinson’s and their treatment for Parkinson’s may family, friends and carers. change later on. It provides information Reading the bits of this about the drugs most information that you need will commonly used to help also make this booklet more manage the condition. manageable and relevant for you. This booklet starts with some key practical points about the drugs used for treating Parkinson’s, then gives further details about categories of drugs and individual drugs. There is also a summary that gives an overview list of Parkinson’s drugs. Choosing the right medication is always a decision you should make with your specialist or Parkinson’s nurse. You can show this booklet to your specialist or Parkinson’s nurse and ask them questions about the information here. You may also find it a useful starting point when you are talking about the next steps in your treatment. Contents Section 1 This gives an overview of Parkinson’s medication and is recommended for anyone with the condition. Parkinson’s drugs: an introduction .........................................................6 This includes how drugs work, their names and what treatment to take. Other ways to manage your Parkinson’s .............................................9 This includes exercise and therapies. -

Problems Encountered When Testing for LSD in a Regional Medium Secure Unit 17
Acosta-Armas Te sting for LSD Psychiatric Bulletin (2003), 27,17^19 A. J. ACOSTA-ARMAS original Problems encountered when testing for LSD in a regional papers medium secure unit AIMS AND METHOD same day, to two different labora- without adequate confirmatory Between1998 and 2000, a surpris- tories. At the first laboratory, only analysis, many psychiatric and non- ingly high number of positive results one test method was used and at the psychiatric prescribed drugs can give was noticed in our regional medium second one test plus two confirma- false positives. secure unit when testing for D- tory tests were carried out. lysergic acid diethylamide (LSD).This CLINICAL IMPLICATIONS led to an investigation of possible RESULTS Positive LSD results should be con- factorsinvolved.Itwasfeltthatthe Outofatotalof23patientstestedon firmed by at least one, preferably testing protocol, particularly the use two separate occasions, the first chromatographic, alternative of a single, non-isotopic homoge- laboratory gave three positive results method. A protocol for testing and neous immunoassay without routine the first time and three positive reporting LSD in psychiatric patients further confirmatory testing, was results the second, while the second should be considered in order to largely to blame for what seemed to laboratory gave only one positive minimise the risk of obtaining false- be a high incidence of false positives. result on the second occasion that positive results which have negative On two different occasions, samples samples were sent and none on the clinical, legal and psychological from each patient were sent, on the first.This reinforces the belief that, repercussions. Introduction immunoassays (enzyme-linked immunosorbent assay (ELISA) and enzyme-multiplied immunoassay technique The use of D-lysergic acid diethylamide (LSD), a strong (EMIT)), high performance thin-layer chromatography and hallucinogenic drug, continues to cause concern within gas or liquid chromatography linked to mass spectro- the medical profession and particularly in the field of metry. -

Drugs Which Can Affect Near Vision: a Useful List
Drugs Which Can Affect Near Vision: A Useful List Joanne L. Smith B.Sc., Ph.Phm.* J. Raymond Buncic, M.D., F.R.C.S.(C)t ABSTRACT This paper documents a list of drugs that cause problems with near vision, by virtue of effects on accommodation, occasionally refractive error and diplopia. It is meant as a reference aid to the clinician when confronted with problems of focusing on near objects or print. There are many drugs that have been reported to interfere with near or reading vision, producing blurring, decreased accommodation and diplopia. This paper lists the drugs that have been reported in the literature to produce symptoms which interfere with near vision. Case reports for the listed drugs vary greatly from many to few. The drugs have been divided into the following categories: those causing (A) blurring at near, (B) diplopia and (C) induced myopia. Those drugs which only rarely cause these symptoms have been omitted. From the Departments of Pharmacy* and Ophthalmologyt, The Hospital For Sick Children, Toronto, Ontario, Canada Requests for reprints should be addressed to: Dr. J. Raymond Buncic, Department of Ophthalmology, The Hospital For Sick Children, 555 University Ave., Toronto, Ontario, Canada M5G lX8 TABLE 1 DRUGS COMMONLY CAUSING DIFFICULTY WITH FOCUSING AT NEAR OR BLURRED VISION. DRUG INCIDENCE REFERENCE Antipsychotics Chlorpromazine 14-23 8 Clozapine 5 8,14 Fluphenazine 1.2-4.3 8 Haloperidol 6.8-16 8 Loxapine 12,14 Perphenazine 7.4-17.8 8 Pimozide 20 8 Risperidone 1-2%, >/= 10% 11 Thioridazine 0.6-18 8 Thiothixene 20 8 -

West Essex CCG Anticholinergic Side-Effects and Prescribing Guidance
Anticholinergic side-effects and prescribing guidance . Anticholinergic (antimuscarinic) medications: associated with increased risks of impaired cognition and falls in patients over the age of 65 years. Recent research also points to a link to mortality increasing with the number and potency of anticholinergic agents prescribed. Anticholinergic Syndrome: is a state of confusion with characteristic features related to dysfunction of the autonomic parasympathetic (cholinergic) nervous system. Symptoms classified into systemic and CNS manifestations: o Systemic (peripheral) symptoms: Blurred vision, photophobia, non-reactive mydriasis, loss of accommodation response, flushed and dry skin, dry mouth, tachycardia, hypertension and fever. Gastrointestinal and urinary motility are frequently reduced o CNS symptoms: Delirium, agitation, disorientation, and visual hallucinations. Ataxia, choreoathetosis, myoclonus and seizures may also occur without peripheral symptoms. Medication Issues: several commonly prescribed medications that may not be thought of as anticholinergic have significant anticholinergic effects, which when taken with known anticholinergic medication can increase the risk of adverse effects. Many medication groups e.g. antihistamines, tricyclic antidepressants, drugs for asthma and COPD, cold preparations, hyoscine have varying degrees of anticholinergic activity and have the potential to cause Anticholinergic Syndrome . Clinicians should be aware of the risk for chronic anticholinergic toxicity and the fact that not all the symptoms may manifest in patients and if they do suffer some symptoms they could be wrongly attributed to another diagnosis Evidence . A study of patients over 65 found that 20% of participants who scored four or more had died by the end of the two year study period compared with 7% of patients with a score of zero.