Drug-Induced Immune Thrombocytopenia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protein S Deficiency Presenting with Hemorrhage in a Term Neonate
: Curre re nt a R C e Ayari et al., Health Care Current Reviews 2018, 6:1 h v t i l e a w DOI: 10.4172/2375-4273.1000219 e s H Health Care: Current Reviews ISSN: 2375-4273 Review Article Open Access Protein S Deficiency Presenting with Hemorrhage in a Term Neonate Fairouz Ayari*, Takoua Bensmail, Essid Latifa, Wiem Barbaria and Samia Kacem Neonatology Intensive Care Unit of the Maternity and Neonatology Center, Tunis, Tunisia Abstract Unexplained bleeding symptoms in otherwise healthy full-term usually present a diagnostic challenge for treating physicians requiring prompt and accurate laboratory investigations to ensure appropriate treatment and possibly avoid long-term morbidity. We report a case of a term neonate with severe protein S deficiency manifested by systemic hemorrhage and multiple organ failure at 9 days of age. We review how protein S influences the coagulation and the fibrinolytic pathways, discussing therapeutic approaches of neonates with purpura fulminans. Keywords: Protein S deficiency; Blood sample; Thrombophilic dis- resuscitation with 20 ml/kg bodyweight (BW) saline solution and, after order blood sampling, intravenous administration of 10 mg vitamin K, 20 ml/kg BW fresh frozen plasma, 20 ml/kg BW packed red blood cells Introduction (5 transfusion cycles), 20 mg/kg BW Phenobarbital and vasoactive Protein S (PS) is an antithrombotic plasma protein that acts mainly drugs. Cerebral ultrasound revealed intraventricular haemorrhage, as a cofactor of activated protein C (APC) anticoagulant activity in the abdominal ultrasound showed splenic hemorrhage and cardiac degradation of factor Va and activated factor VIII [1]. PS circulates in ultrasound showed a floating intracardiac thrombus. -

Outcomes of Patients with Thrombocytopenia Evaluated at Hematology Subspecialty Clinics
Henry Ford Health System Henry Ford Health System Scholarly Commons Hematology Oncology Articles Hematology-Oncology 2-11-2021 Outcomes of patients with thrombocytopenia evaluated at hematology subspecialty clinics Zaid H. Abdel Rahman Kevin C. Miller H Jabbour Yaser Alkhatib Vijayalakshmi Donthireddy Follow this and additional works at: https://scholarlycommons.henryford.com/ hematologyoncology_articles Hematol Oncol Stem Cell Ther xxx (xxxx) xxx Available at www.sciencedirect.com ScienceDirect journal homepage: www.elsevier.com/locate/hemonc Outcomes of patients with thrombocytopenia evaluated at hematology subspecialty clinics Zaid H. Abdel Rahman a,*, Kevin C. Miller b, Hiba Jabbour c, Yaser Alkhatib c, Vijaya Donthireddy c a Division of Hematology and Medical Oncology, Mayo Clinic, Jacksonville, FL, USA b Department of Medicine, Massachusetts General Hospital, Boston, MA, USA c Division of Hematology and Medical Oncology, Henry Ford Hospital, Detroit, MI, USA Received 6 October 2020; received in revised form 9 December 2020; accepted 15 January 2021 KEYWORDS Abstract Hematology; Background: Thrombocytopenia is a frequently encountered laboratory abnormality and a Malignancy; common reason for hematology referrals. Workup for thrombocytopenia is not standardized Platelets; and frequently does not follow an evidence-based algorithm. We conducted a systematic anal- Referrals; Thrombocytopenia ysis to evaluate the laboratory testing and outcomes of patients evaluated for thrombocytope- nia at hematology clinics in a tertiary referral center between 2013 and 2016. Patient and methods: We performed a comprehensive chart review for patients evaluated for thrombocytopenia during the study period. Patients were followed for 1 year from the initial hematology evaluation and assessed for the development of a hematologic malignancy, rheumatologic, or infectious diseases among other clinical outcomes. -

Severe Fever with Thrombocytopenia Syndrome: a Newly Discovered Emerging Infectious Disease
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector REVIEW Severe fever with thrombocytopenia syndrome: a newly discovered emerging infectious disease D. X. Li Key Laboratory for Medical Virology, National Institute for Viral Disease Control and Prevention, China CDC, Beijing, China Abstract Severe fever with thrombocytopenia syndrome (SFTS) is a newly discovered emerging infectious disease that has recently become epidemic in Asia. The causative agent of SFTS is a novel phlebovirus in the family Bunyaviridae, designated SFTS virus (SFTSV). SFTS clinically presents with high fever, thrombocytopenia, leukocytopenia, gastrointestinal disorders, and multi-organ dysfunction, with a high viral load and a high case- fatality rate. In human infection, SFTSV targets microphages, replicates in the spleen of infected mice, and causes thrombocytopenia and a cytokine storm. The tick disseminates virus to humans and animals, forming a special transmission model in nature. Person-to-person transmission though direct contact with patient blood has been frequently reported. Measurements of viral RNA and antibodies have been established for diagnosis, but vaccines and specific therapeutics are not available so far. Clinical Microbiology and Infection © 2015 European Society of Clinical Microbiology and Infectious Diseases. Published by Elsevier Ltd. All rights reserved. Keywords: Clinical, epidemiology, SFTS virus, SFTS, virology Article published online: 11 March 2015 Virology D.X. Li, Key Laboratory for Medical Virology, NCHFP, RRC, National Institute for Viral Disease Control and Prevention, China CDC, Bei- jing 102206, China E-mail: [email protected] The causative agent of SFTS is SFTSV, which is a tick-borne virus in the family Bunyaviridae, genus Phlebovirus. -

Neonatal Leukopenia and Thrombocytopenia
Neonatal Leukopenia and Thrombocytopenia Vandy Black, M.D., M.Sc., FAAP March 3, 2016 April 14, 2011 Objecves • Summarize the differenHal diagnosis of leukopenia and/or thrombocytopenia in a neonate • Describe the iniHal steps in the evaluaon of a neonate with leukopenia and/or thrombocytopenia • Review treatment opHons for leukopenia and/ or thrombocytopenia in the NICU Clinical Case 1 • One day old male infant admiUed to the NICU for hypoglycemia and a sepsis rule out • Born at 38 weeks EGA by SVD • Birth weight 4 lbs 13 oz • Exam shows a small cephalohematoma; no dysmorphic features • PLT count 42K with an otherwise normal CBC Definions • Normal WBC count 9-30K at birth – Mean 18K • What is the ANC and ALC – <1000/mm3 is abnormal – 6-8% of infants in the NICU • Normal platelet count: 150-450,000/mm3 – Not age dependent – 22-35% of infants in the NICU have plts<150K Neutropenia Absolute neutrophil count <1500/mm3 Category ANC* InfecHon risk • Mild 1000-1500 None • Moderate 500-1000 Minimal • Severe <500 Moderate to Severe (Highest if <200) • Recurrent bacterial or fungal infecHons are the hallmark of symptomac neutropenia! • *ANC = WBC X % (PMNs + Bands) / 100 DefiniHon of Neutropenia Black and Maheshwari, Neoreviews 2009 How to Approach Cytopenias • Normal vs. abnormal (consider severity) • Malignant vs. non-malignant • Congenital vs. acquired • Is the paent symptomac • Transient, recurrent, cyclic, or persistent How to Approach Cytopenias • Adequate vs. decreased marrow reserve • Decreased producHon vs. increased destrucHon/sequestraon Decreased neutrophil/platelet producon • Primary – Malignancy/leukemia/marrow infiltraon – AplasHc anemia – Genec disorders • Secondary – InfecHous – Drug-induced – NutriHonal • B12, folate, copper Increased destrucHon/sequestraon • Immune-mediated • Drug-induced • Consumpon à Hypersplenism vs. -
Thrombocytopenia.Pdf
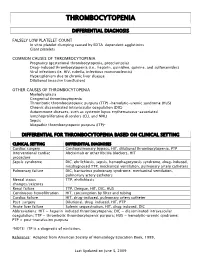
THROMBOCYTOPENIA DIFFERENTIAL DIAGNOSIS FALSELY LOW PLATELET COUNT In vitro platelet clumping caused by EDTA-dependent agglutinins Giant platelets COMMON CAUSES OF THROMBOCYTOPENIA Pregnancy (gestational thrombocytopenia, preeclampsia) Drug-induced thrombocytopenia (i.e., heparin, quinidine, quinine, and sulfonamides) Viral infections (ie. HIV, rubella, infectious mononucleosis) Hypersplenism due to chronic liver disease Dilutional (massive transfusion) OTHER CAUSES OF THROMBOCYTOPENIA Myelodysplasia Congenital thrombocytopenia Thrombotic thrombocytopenic purpura (TTP) -hemolytic-uremic syndrome (HUS) Chronic disseminated intravascular coagulation (DIC) Autoimmune diseases, such as systemic lupus erythematosus-associated lymphoproliferative disorders (CLL and NHL) Sepsis Idiopathic thrombocytopenic purpura (ITP)* DIFFERENTIAL FOR THROMBOCYTOPENIA BASED ON CLINICAL SETTING CLINICAL SETTING DIFFERENTIAL DIAGNOSES Cardiac surgery Cardiopulmonary bypass, HIT, dilutional thrombocytopenia, PTP Interventional cardiac Abciximab or other IIb/IIIa blockers, HIT procedure Sepsis syndrome DIC, ehrlichiosis, sepsis, hemophagocytosis syndrome, drug-induced, misdiagnosed TTP, mechanical ventilation, pulmonary artery catheters Pulmonary failure DIC, hantavirus pulmonary syndrome, mechanical ventilation, pulmonary artery catheters Mental status TTP, ehrlichiosis changes/seizures Renal failure TTP, Dengue, HIT, DIC, HUS Continuous hemofiltration HIT, consumption by filter and tubing Cardiac failure HIT, drug-induced, pulmonary artery catheter Post-surgery -
Canine and Feline Coagulopathies Office News Michelle Fulks, DVM, Virginia Sinnott, DVM, DACVECC William B
Monthly Update August 2013 Issue Contributors: Michelle Fulks, DVM, Virginia Sinnott, DVM, DACVECC, William B. Henry DVM, DACVS Editor: William B. Henry DVM, DACVS Canine and Feline Coagulopathies Office News Michelle Fulks, DVM, Virginia Sinnott, DVM, DACVECC William B. Henry, Jr. DVM, DACVS Canine and Feline Coagulopathies Bleeding disorders are considered a potential life-threatening emergency in small animal practice. It is crucial to recognize the potential for a coagulation disorder through history and physical exam findings, pursue appropriate diagnostic tests and then treat appropriately in order to prevent massive bleeding in these patients. Three areas of the hemostatic system may be affected to cause coagulopathies: Amanda Spencer, CVT joined our surgery team in late 2012. She has 10 1. Disorders of Primary Hemostasis years experience in surgery and 2. Disorders of Secondary Hemostasis emergency care. Her sole focus at BVS 3. Disorders of Fibrinolysis is with the surgical practice. Her skills, dedication to excellence, and caring Primary hemostasis is the formation of the initial platelet plug. Decreases in attitude towards our clients and platelet number, platelet function, or reduced von Willebrand factor (VWF) can all patients, has been outstanding. Her cause disorders of primary hemostasis and lead to mucosal bleeding or calm upbeat personality makes our bruising. Secondary hemostasis is the formation of a stable fibrin clot via cascade days together as a team more of enzymes that ultimately convert fibrinogen to fibrin. Defects in coagulation enjoyable. She is one of those staff factors can lead to severe bleeding diatheses. Fibrinolysis is the breakdown of the members "behind the public eye" who fibrin clot by plasmin. -

Thrombocytopenia and Intracranial Venous Sinus Thrombosis After “COVID-19 Vaccine Astrazeneca” Exposure
Journal of Clinical Medicine Article Thrombocytopenia and Intracranial Venous Sinus Thrombosis after “COVID-19 Vaccine AstraZeneca” Exposure Marc E. Wolf 1,2 , Beate Luz 3, Ludwig Niehaus 4 , Pervinder Bhogal 5, Hansjörg Bäzner 1,2 and Hans Henkes 6,7,* 1 Neurologische Klinik, Klinikum Stuttgart, D-70174 Stuttgart, Germany; [email protected] (M.E.W.); [email protected] (H.B.) 2 Department of Neurology, Universitätsmedizin Mannheim, University of Heidelberg, D-68167 Mannheim, Germany 3 Zentralinstitut für Transfusionsmedizin und Blutspendedienst, Klinikum Stuttgart, D-70174 Stuttgart, Germany; [email protected] 4 Neurologie, Rems-Murr-Klinikum Winnenden, D-71364 Winnenden, Germany; [email protected] 5 Department of Interventional Neuroradiology, The Royal London Hospital, Barts NHS Trust, London E1 1FR, UK; [email protected] 6 Neuroradiologische Klinik, Klinikum Stuttgart, D-70174 Stuttgart, Germany 7 Medical Faculty, University Duisburg-Essen, D-47057 Duisburg, Germany * Correspondence: [email protected]; Fax: +49-711-278-345-09 Abstract: Background: As of 8 April 2021, a total of 2.9 million people have died with or from the coronavirus infection causing COVID-19 (Corona Virus Disease 2019). On 29 January 2021, the European Medicines Agency (EMA) approved a COVID-19 vaccine developed by Oxford University Citation: Wolf, M.E.; Luz, B.; and AstraZeneca (AZD1222, ChAdOx1 nCoV-19, COVID-19 vaccine AstraZeneca, Vaxzevria, Cov- Niehaus, L.; Bhogal, P.; Bäzner, H.; ishield). While the vaccine prevents severe course of and death from COVID-19, the observation of Henkes, H. Thrombocytopenia and pulmonary, abdominal, and intracranial venous thromboembolic events has raised concerns. Objec- Intracranial Venous Sinus Thrombosis after “COVID-19 Vaccine tive: To describe the clinical manifestations and the concerning management of patients with cranial AstraZeneca” Exposure. -

Immune Thrombocytopenia: Antiplatelet Autoantibodies Inhibit Proplatelet Formation by Megakaryocytes and Impair Platelet Production in Vitro
Perdomo J. Immune Thrombocytopenia: Antiplatelet Autoantibodies Inhibit Proplatelet Formation by Megakaryocytes and Impair Platelet Production in vitro. J Immunological Sci. (2018); 2(6): 1-3 Journal of Immunological Sciences Commentary Article Open Access Immune Thrombocytopenia: Antiplatelet Autoantibodies Inhibit Proplatelet Formation by Megakaryocytes and Impair Platelet Production in vitro José Perdomo Haematology Research Unit, St George and Sutherland Clinical School, Faculty of Medicine, University of New South Wales, Sydney, NSW, Australia This commentary review considers the above publication, as Article Info invited by the Journal of Immunological Science. These data are Article Notes already published and no additional data are provided. The paper Received: September 3, 2018 Accepted: November 1, 2018 deals with samples from 19 immune thrombocytopenia patients and was published in the journal Haematologica1. *Correspondence: Dr. José Perdomo, Haematology Research Unit, St George Immune thrombocytopenia (ITP) is an autoimmune bleeding and Sutherland Clinical School, Faculty of Medicine, condition characterised by low platelet counts (< 100 x 109/L; University of New South Wales, Sydney, NSW, Australia; 9 Telephone No: +61 2 91131915; reference count 150 – 400 x 10 /L) in the absence of other triggers Email: [email protected] that may cause thrombocytopenia2. Bleeding (petechiae, mucosal bleeding) is a common sign of ITP. There is a risk of internal bleeding © 2018 Perdomo J. This article is distributed under the terms of 3 the Creative Commons Attribution 4.0 International License. and fatal haemorrhage has been reported . ITP patients have reduced quality of life and decreased life expectancy4. Autoantibodies against abundant platelets antigens such as glycoproteins (GP) Ib/IX and IIb/ IIIa are found in ITP patients and contribute to platelet destruction. -

Thrombocytopenia in Older Adults Melissa (Kah Poh) Loh, MD
URMC Division of Geriatrics & Aging March 2019 Thrombocytopenia in Older adults Melissa (Kah Poh) Loh, MD Background Thrombocytopenia (or low platelet count) is a common hematologic abnormality encountered in older adults Common causes of thrombocytopenia include (Table 1): Immune-related [e.g. immune thrombocytopenia purpura (ITP)] Drug-induced [e.g. heparin-induced thrombocytopenia (HIT)] Bone marrow failure Other: Infections (e.g. H. pylori, HIV, hepatitis), pseudothrombocytopenia (Figure 1), alcohol abuse, liver Figure 1: Peripheral smear showing clumped cirrhosis, blood transfusion, thrombotic thrombocytopenia platelets (pseudothrombocytopenia — falsely purpura (TTP), and hemolytic-uremic syndrome (HUS), low platelet count) thyroid disease Age-related changes in the organ and vasculature systems increase the risks of thrombocytopenia on hemostasis Factors that may enhance bleeding in older adults. These include: Comorbidities Medications Loss of subcutaneous tissue Age-specific factors that may prevent bleeding in older adults include enhanced platelet aggregation and increased fibrinogen, factor V, and von Willebrand factor Thrombocytopenia is often multifactorial in older adults. Table 1: Quick Facts on Thrombocytopenia PATHOPHYSIOLOGY Immune Thrombocytopenia Purpura Drug-Induced Increased platelet clearance in the reticulo-endothelial Impaired production (direct marrow toxicity or system of bone marrow, spleen, and/or liver megakaryocyte-specific inhibition) Inadequate platelet production due to megakaryocyte Increased platelet clearance (indirect immune clearance, inhibition by IgG antibodies antibody-specific immune clearance, miscellaneous immune -mediated) Often suppress other cell lines CAUSES Immune Thrombocytopenia Purpura Drug-Induced Often idiopathic See Table 2 Can be associated with underlying hematologic abnormalities (e.g. myelodysplastic syndrome, chronic lymphocytic leukemia) INCIDENCE RATES Immune Thrombocytopenia Purpura Drug-Induced 4.62 per 100,000 adults aged >60 years vs. -

Hemophilia Update 2015
J. Martin Johnston, MD Pediatric Project ECHO 7 December 2018 Objectives Review history and physical exam as they relate to a potential bleeding disorder Discuss step-wise laboratory evaluation: screening labs and follow-ups Review some common congenital and acquired bleeding disorders, and their management Objectives Review history and physical exam as they relate to a potential bleeding disorder Discuss step-wise laboratory evaluation: screening labs and follow-ups Review some common congenital and acquired bleeding disorders, and their management Objectives Review history and physical exam as they relate to a potential bleeding disorder Discuss step-wise laboratory evaluation: screening labs and follow-ups Review some common congenital and acquired bleeding disorders, and their management The chief complaint “Easy” bruising Nosebleeds Petechiae Menorrhagia Bleeding after Circumcision Tonsillectomy/adenoidectomy, tooth extraction Mild (head) trauma The problem…. • Everyone bleeds. • All bleeding eventually stops. The bleeding history Birth/neonatal Tooth eruption/shedding Bruising Nosebleeds Surgeries? (don’t forget circumcision!) Orthopedic hx (traumas, joints) Menstruation Family history How much bleeding is too much? Neonatal ICH, needle/heel sticks, post-circumcision How much bleeding is too much? Neonatal ICH, needle/heel sticks, post-circumcision Infant Petechiae, chest/back/buttock bruising Consider NAT How much bleeding is too much? Neonatal ICH, needle/heel sticks, post-circumcision Infant -

Pathophysiology and Diagnosis of Drug-Induced Immune Thrombocytopenia
Journal of Clinical Medicine Review Pathophysiology and Diagnosis of Drug-Induced Immune Thrombocytopenia Caroline Vayne 1,2 , Eve-Anne Guéry 2,Jérôme Rollin 1,2, Tatiana Baglo 2,3, Rachel Petermann 4,5 and Yves Gruel 1,2,* 1 EA 7501-Groupe Innovation et Ciblage Cellulaire (GICC), Université François Rabelais, CEDEX 01, 37032 Tours, France; [email protected] (C.V.); [email protected] (J.R.) 2 Laboratoire d’Hématologie-Hémostase, Hôpital Trousseau, CHRU Tours, CEDEX 09, 37044 Tours, France; [email protected] (E.-A.G.); [email protected] (T.B.) 3 Laboratoire d’Hématologie, CNHU de Cotonou, Cotonou 01 BP 386, Benin 4 Département d’Immunologie plaquettaire, Institut National de la Transfusion Sanguine (INTS), 75015 Paris, France; [email protected] 5 Equipe ETRES (Ethics, Research, Translations), Centre de Recherche des Cordeliers, UMRS 1138, INSERM, Sorbonne Université, Université de Paris, 75006 Paris, France * Correspondence: [email protected]; Tel.: +33-2-4747-4672; Fax: +33-2-4747-5904 Received: 25 June 2020; Accepted: 10 July 2020; Published: 13 July 2020 Abstract: Drug-induced immune thrombocytopenia (DITP) is a life-threatening clinical syndrome that is under-recognized and difficult to diagnose. Many drugs can cause immune-mediated thrombocytopenia, but the most commonly implicated are abciximab, carbamazepine, ceftriaxone, eptifibatide, heparin, ibuprofen, mirtazapine, oxaliplatin, penicillin, quinine, quinidine, rifampicin, suramin, tirofiban, trimethoprim-sulfamethoxazole, and vancomycin. Several different mechanisms have been identified in typical DITP, which is most commonly characterized by severe thrombocytopenia due to clearance and/or destruction of platelets sensitized by a drug-dependent antibody. Patients with typical DITP usually bleed when symptomatic, and biological confirmation of the diagnosis is often difficult because detection of drug-dependent antibodies (DDabs) in the patient’s serum or plasma is frequently not possible. -

Thromboelastometry Identifies Coagulopathy Associated with Liver Israelita Albert Einstein - São Paulo (SP), Brasil
RELATO DE CASO Tomaz Crochemore1 , Felício Aragão Savioli1 , João Carlos de Campos Guerra2, Erika Maria do A tromboelastometria identifica coagulopatia Nascimento Kalmar3 associada à insuficiência hepática e coagulação intravascular disseminada causadas por febre amarela, orientando a terapia hemostática específica: um relato de caso 1. Medicina Intensiva, Hospital Leforte - São Paulo (SP), Brasil. 2.Centro de Hematologia e Laboratório, Hospital Thromboelastometry identifies coagulopathy associated with liver Israelita Albert Einstein - São Paulo (SP), Brasil. 3.Infectologia, Hospital Israelita Albert Einstein - failure and disseminated intravascular coagulation caused by São Paulo (SP), Brasil. yellow fever, guiding specific hemostatic therapy: a case report RESUMO tromboelastometria identificou o distúrbio de coagulação específico e, assim, orientou Este relato de caso detalha um caso grave o tratamento hemostático. Administraram- de febre amarela complicada por insuficiência se concentrados de fibrinogênio e vitamina hepática e coagulação intravascular K, não sendo necessária a transfusão disseminada. A tromboelastometria de qualquer componente do sangue, foi capaz de identificar os distúrbios mesmo na presença de trombocitopenia. da coagulação e orientar o tratamento A tromboelastometria permitiu a hemostático. Relatamos o caso de um identificação precoce da coagulopatia e homem com 23 anos de idade admitido ajudou a orientar a terapêutica hemostática. na unidade de terapia intensiva com A administração de fármacos hemostáticos, quadro com início abrupto de febre e incluindo concentrados de fibrinogênio dor muscular generalizada associados e vitamina K, melhorou os parâmetros a insuficiência hepática e coagulação tromboelastométricos, com correção do intravascular disseminada. Os resultados transtorno da coagulação. Não se realizou dos exames laboratoriais convencionais transfusão de hemocomponentes, e não revelaram trombocitopenia, enquanto a ocorreu qualquer sangramento.