Effect of Progesterone, Terbutaline and Leptin on the Function Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Betamethasone
Betamethasone Background Betamethasone is a potent, long-acting, synthetic glucocorticoid widely used in equine veterinary medicine as a steroidal anti-inflammatory.1 It is often administered intra-articularly for control of pain associated with inflammation and osteoarthritis.2 Betamethasone is a prescription medication and can only be dispensed from or upon the request of a http://en.wikipedia.org/wiki/Betamethasone#/media/File:Betamethasone veterinarian. It is commercially available .png in a variety of formulations including BetaVet™, BetaVet Soluspan Suspension® and Betasone Aqueous Suspension™.3 Betamethasone can be used intra-articularly, intramuscularly, by inhalation, and topically.4 When administered intra-articularly, it is often combined with other substances such as hyaluronan.5 Intra-articular and intramuscular dosages range widely based upon articular space, medication combination protocol, and practitioner preference. Betamethasone is a glucocorticoid receptor agonist which binds to various glucocorticoid receptors setting off a sequence of events affecting gene transcription and the synthesis of proteins. These mechanisms of action include: • Potential alteration of the G protein-coupled receptors to interfere with intracellular signal transduction pathways • Enhanced transcription in many genes, especially those involving suppression of inflammation. • Inhibition of gene transcription – including those that encode pro-inflammatory substances. The last two of these are considered genomic effects. This type of corticosteroid effect usually occurs within hours to days after administration. The genomic effects persist after the concentrations of the synthetic corticosteroid in plasma are no longer detectable, as evidenced by persistent suppression of the normal production of hydrocortisone following synthetic corticosteroid administration.6 When used judiciously, corticosteroids can be beneficial to the horse. -

Steroid Use in Prednisone Allergy Abby Shuck, Pharmd Candidate
Steroid Use in Prednisone Allergy Abby Shuck, PharmD candidate 2015 University of Findlay If a patient has an allergy to prednisone and methylprednisolone, what (if any) other corticosteroid can the patient use to avoid an allergic reaction? Corticosteroids very rarely cause allergic reactions in patients that receive them. Since corticosteroids are typically used to treat severe allergic reactions and anaphylaxis, it seems unlikely that these drugs could actually induce an allergic reaction of their own. However, between 0.5-5% of people have reported any sort of reaction to a corticosteroid that they have received.1 Corticosteroids can cause anything from minor skin irritations to full blown anaphylactic shock. Worsening of allergic symptoms during corticosteroid treatment may not always mean that the patient has failed treatment, although it may appear to be so.2,3 There are essentially four classes of corticosteroids: Class A, hydrocortisone-type, Class B, triamcinolone acetonide type, Class C, betamethasone type, and Class D, hydrocortisone-17-butyrate and clobetasone-17-butyrate type. Major* corticosteroids in Class A include cortisone, hydrocortisone, methylprednisolone, prednisolone, and prednisone. Major* corticosteroids in Class B include budesonide, fluocinolone, and triamcinolone. Major* corticosteroids in Class C include beclomethasone and dexamethasone. Finally, major* corticosteroids in Class D include betamethasone, fluticasone, and mometasone.4,5 Class D was later subdivided into Class D1 and D2 depending on the presence or 5,6 absence of a C16 methyl substitution and/or halogenation on C9 of the steroid B-ring. It is often hard to determine what exactly a patient is allergic to if they experience a reaction to a corticosteroid. -

Therapeutic Drug Class
BUREAU FOR MEDICAL SERVICES EFFECTIVE WEST VIRGINIA MEDICAID PREFERRED DRUG LIST WITH PRIOR AUTHORIZATION CRITERIA 07/01/2018 This is not an all-inclusive list of available covered drugs and includes only Version 2018.3e managed categories. Refer to cover page for complete list of rules governing this PDL. • Prior authorization for a non-preferred agent in any class will be given only if there has been a trial of the preferred brand/generic equivalent or preferred formulation of the active ingredient, at a therapeutic dose, that resulted in a partial response with a documented intolerance. • Prior authorization of a non-preferred isomer, pro-drug, or metabolite will be considered with a trial of a preferred parent drug of the same chemical entity, at a therapeutic dose, that resulted in a partial response with documented intolerance or a previous trial and therapy failure, at a therapeutic dose, with a preferred drug of a different chemical entity indicated to treat the submitted diagnosis. (The required trial may be overridden when documented evidence is provided that the use of these preferred agent(s) would be medically contraindicated.) • Unless otherwise specified, the listing of a particular brand or generic name includes all legend forms of that drug. OTC drugs are not covered unless specified. • PA criteria for non-preferred agents apply in addition to general Drug Utilization Review policy that is in effect for the entire pharmacy program, including, but not limited to, appropriate dosing, duplication of therapy, etc. • The use of pharmaceutical samples will not be considered when evaluating the members’ medical condition or prior prescription history for drugs that require prior authorization. -

DIPROLENE® AF (DIH-Pro-Leen) (Augmented Betamethasone Dipropionate) Cream Important Information: DIPROLENE AF Cream Is for Use on Skin Only
Patient Information DIPROLENE® AF (DIH-pro-leen) (augmented betamethasone dipropionate) Cream Important information: DIPROLENE AF Cream is for use on skin only. Do not use DIPROLENE AF Cream in your eyes, mouth, or vagina. What is DIPROLENE AF Cream? DIPROLENE AF Cream is a prescription corticosteroid medicine used on the skin (topical) for the relief of redness, swelling, heat, pain (inflammation) and itching, caused by certain skin problems in people 13 years of age and older. DIPROLENE AF Cream should not be used in children under 13 years of age. Do not use DIPROLENE AF Cream if you are allergic to betamethasone dipropionate or any of the ingredients in DIPROLENE AF Cream. See the end of this leaflet for a complete list of ingredients in DIPROLENE AF Cream. Before using DIPROLENE AF Cream, tell your healthcare provider about all of your medical conditions, including if you: have had irritation or other skin reaction to a steroid medicine in the past. have thinning of the skin (atrophy) at the treatment site. have diabetes. have adrenal gland problems. have liver problems. have cataracts or glaucoma. are pregnant or plan to become pregnant. It is not known if DIPROLENE AF Cream will harm your unborn baby. If you use DIPROLENE AF Cream during pregnancy, use DIPROLENE AF Cream on the smallest area of the skin and for the shortest time needed. are breastfeeding or plan to breastfeed. It is not known if DIPROLENE AF Cream passes into your breast milk. Breastfeeding women should use DIPROLENE AF Cream on the smallest area of the skin and for the shortest time needed. -
PRODUCT CATALOGUE 2021 Available on Product Known Teva Tech US EU Japan Korea Therapeutic Api IP File*** DMF DMF DMF DMF Area**
S NH2 N N O O O HN CH OH 3 N O SO3H PRODUCT CATALOGUE 2021 Available on www.teva-api.com Product Known Teva Tech US EU Japan Korea therapeutic api IP file*** DMF DMF DMF DMF area** A ABALOPARATIDE Osteoporosis ABEMACICLIB Oncology ABIRATERONE ACETATE Oncology ACALABRUTINIB Oncology AFATINIB Oncology ALCLOMETASONE DIPROPIONATE Dermatology ALLOPURINOL Rheumatology CEP AMCINONIDE Dermatology AMITRIPTYLINE HCl Neurology - Psychiatry CEP ANASTROZOLE Oncology CEP ANIDULAFUNGIN Infectious disease APALUTAMIDE* Oncology Coagulation APIXABAN inhibitors APREMILAST* Psoriasis ARIPIPRAZOLE* Neurology-Psychiatry CEP ATOMOXETINE HCl Neurology-Psychiatry ATORVASTATIN CALCIUM Lipid lowering CEP Preterm labor ATOSIBAN ACETATE prevention ATRACURIUM BESYLATE Muscle relaxant CEP AZACITIDINE Oncology AZITHROMYCIN DIHYDRATE Infectious disease CEP AZITHROMYCIN MONOHYDRATE Infectious disease CEP AZTREONAM* Infectious disease B BALOXAVIR Antiviral 2 Product Known Teva Tech US EU Japan Korea therapeutic api IP file*** DMF DMF DMF DMF area** BARICITINIB Rheumatology BECLOMETHASONE DIPROPIONATE Respiratory CEP BETAMETHASONE ACETATE Inflammation BETAMETHASONE BASE Dermatology CEP BETAMETHASONE DIPROPIONATE Dermatology CEP BETAMETHASONE VALERATE Dermatology CEP BICALUTAMIDE Oncology CEP BIVALIRUDIN Hematology BLEOMYCIN SULFATE Oncology BORTEZOMIB Oncology BREXANOLONE Neurology-Psychiatry BREXPIPRAZOLE Neurology-Psychiatry BROMOCRIPTINE MESYLATE Cardiovascular CEP BUDESONIDE Respiratory CEP BUPRENORPHINE BASE Neurology-Psychiatry CEP BUPRENORPHINE HCl Neurology-Psychiatry -

Rectal Corticosteroids Versus Alternative Treatments in Ulcerative Colitis: a Meta-Analysis Gut: First Published As 10.1136/Gut.40.6.775 on 1 June 1997
Gut 1997; 40: 775-781 775 Rectal corticosteroids versus alternative treatments in ulcerative colitis: a meta-analysis Gut: first published as 10.1136/gut.40.6.775 on 1 June 1997. Downloaded from J K Marshall, E J Irvine Abstract medication consistently to the splenic Background-Clear strategies to optimise flexure,49 and a larger volume seems to allow the use of corticosteroids in ulcerative more proximal delivery.10 11 Rectal foam dis- colitis are lacking. seminates medication to the rectum and distal Aim-A meta-analysis was undertaken to descending colon,'2-16 whereas suppositories examine critically the role of rectal corti- coat only the rectum.'7 18 costeroids in the management of active Although studies of rectally administered distal ulcerative colitis. corticosteroids have reported fewer systemic Methods-AJl reported randomised con- adverse effects than with oral preparations, trolled trials were retrieved by searching plasma concentrations of prednisolone were the Medline and EMBASE databases and similar after administration of identical oral or the bibliographies of relevant studies. rectal doses.'9 20 Suppression of the hypo- Trials which met inclusion criteria were thalamic-pituitary-adrenal axis in association assessed for scientific rigour. Data were with rectal therapy has also been shown.2' 26 extracted by two independent observers Newer topically active corticosteroids such according to predetermined criteria. as tixocortol, beclomethasone, prednisolone Results-Of 83 trials retrieved, 33 met metasulphabenzoate, and budesonide, with inclusion criteria. Pooled odds ratios restricted absorption or rapid hepatic metab- (POR) showed conventional rectal corti- olism have been developed to reduce the costeroids and rectal budesonide to be adverse effects associated with conventional clearly superior to placebo. -
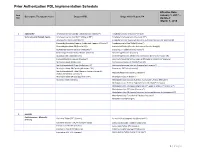
Prior Authorization PDL Implementation Schedule
Prior Authorization PDL Implementation Schedule Effective Date: Item January 1, 2017 – Descriptive Therapeutic Class Drugs on PDL Drugs which Require PA Nbr Updated: March 1, 2018 1 ADD/ADHD Amphetamine Salt Combo Tablet ( Generic Adderall®) Amphetamine ODT (Adzenys® XR ODT) Stimulants and Related Agents Amphetamine Salt Combo ER (Adderall XR®) Amphetamine Suspension (Dyanavel XR®) Atomoxetine Capsule (Strattera®) Amphetamine Salt Combo ER (Generic; Authorized Generic for Adderall XR) Dexmethylphenidate (Generic; Authorized Generic of Focalin®) Amphetamine Sulfate Tablet (Evekeo®) Dexmethylphenidate ER (Focalin XR®) Armodafinil Tablet (Generic; Authorized Generic; Nuvigil®) Dextroamphetamine Solution (Procentra®) Clonidine ER Tablet (Generic; Kapvay®) Dextroamphetamine Sulfate Tablet (Generic) Dexmethylphenidate (Focalin®) Guanfacine ER Tablet (Generic) Dexmethylphenidate XR (Generic; Authorized Generic for Focalin XR) Lisdexamfetamine Capsule (Vyvanse®) Dextroamphetamine Sulfate Capsule ER (Generic; Dexedrine®Spansule) Methylphenidate IR (Generic) Dextroamphetamine IR Tablet (Zenzedi®) Methylphenidate ER Chew (Quillichew ER®) Dextroamphetamine Solution (Generic for Procentra®) Methylphenidate ER Capsule (Metadate CD®) Guanfacine ER Tablet (Intuniv®) Methylphenidate ER Tablet (Generic; Generic Concerta®; Methamphetamine (Generic; Desoxyn®) Authorized Generic Concerta®) Methylphenidate ER Susp (Quillivant XR®) Methylphenidate IR (Ritalin®) Modafinil Tablet (Generic) Methylphenidate Solution (Generic; Authorized Generic; Methylin®) Methylphenidate -

Comparative Study of Dexamethasone and Betamethasone for Women at Risk of Preterm Birth
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Chhatrala JJ et al. Int J Reprod Contracept Obstet Gynecol. 2015 Aug;4(4):1000-1003 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20150414 Research Article Comparative study of dexamethasone and betamethasone for women at risk of preterm birth Jimitkumar J. Chhatrala*, Rutwa Chawada Department of Obstetrics and Gynaecology, SBKS Medical Institute and Research Centre, Pipariya, Waghodia, Vadodara, Gujarat, India Received: 30 April 2015 Revised: 12 July 2015 Accepted: 19 July 2015 *Correspondence: Dr. Jimitkumar J. Chhatrala, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Prematurity represents a serious problem for healthcare services throughout the world. Respiratory distress syndrome, neonatal death, intra-ventricular hemorrhage and low birth weight are continues to be the serious problems during the neonatal period, affecting a large number of premature infants. Dexamethasone and betamethasone are the two antenatal corticosteroids recommended for accelerating fetal lung development in threatened preterm birth. Methods: This is a prospective comparative study conducted in the Department of Obstetrics and Gynecology, at Hiram Hospital, a tertiary care center situated in the rural area of Vadodara, in which 100 pregnant women of gestational age between 24 and 34 weeks with risk of preterm birth were taken as candidates for antenatal treatment with corticosteroids. -

Pharmacologic Characteristics of Corticosteroids 대한신경집중치료학회
REVIEW J Neurocrit Care 2017;10(2):53-59 https://doi.org/10.18700/jnc.170035 eISSN 2508-1349 Pharmacologic Characteristics of Corticosteroids 대한신경집중치료학회 Sophie Samuel, PharmD1, Thuy Nguyen, PharmD1, H. Alex Choi, MD2 1Department of Pharmacy, Memorial Hermann Texas Medical Center, Houston, TX; 2Department of Neurosurgery and Neurology, The University of Texas Medical School at Houston, Houston, TX, USA Corticosteroids (CSs) are used frequently in the neurocritical care unit mainly for their anti- Received December 7, 2017 inflammatory and immunosuppressive effects. Despite their broad use, limited evidence Revised December 7, 2017 exists for their efficacy in diseases confronted in the neurocritical care setting. There are Accepted December 17, 2017 considerable safety concerns associated with administering these drugs and should be limited Corresponding Author: to specific conditions in which their benefits outweigh the risks. The application of CSs in H. Alex Choi, MD neurologic diseases, range from traumatic head and spinal cord injuries to central nervous Department of Pharmacy, Memorial system infections. Based on animal studies, it is speculated that the benefit of CSs therapy Hermann Texas Medical Center, 6411 in brain and spinal cord, include neuroprotection from free radicals, specifically when given Fannin Street, Houston, TX 77030, at a higher supraphysiologic doses. Regardless of these advantages and promising results in USA animal studies, clinical trials have failed to show a significant benefit of CSs administration Tel: +1-713-500-6128 on neurologic outcomes or mortality in patients with head and acute spinal injuries. This Fax: +1-713-500-0665 article reviews various chemical structures between natural and synthetic steroids, discuss its E-mail: [email protected] pharmacokinetic and pharmacodynamic profiles, and describe their use in clinical practice. -

HPLC Analysis of Betamethasone Dipropionate Using a Quasar C18
APPLICATION BRIEF Liquid Chromatography Authors: Kyle Saunders Kathryn Lawson-Wood PerkinElmer, Inc. Seer Green, UK HPLC Analysis of Introduction Betamethasone Dipropionate Glucocorticoid steroids work by suppressing various aspects of Using a Quasar C18 Column the human immune system in conditions where hyperactivity can in Accordance with the United cause poor health through allergies, inflammation and autoimmune States Pharmacopeia dysfunction. Betamethasone dipropionate belongs to this class of steroids. It is used for its high potency as an anti-inflammatory and immunosuppressant in the treatment of diseases such as eczema, dermatitis and psoriasis. Betamethasone dipropionate is classified as a ‘super-potent’ steroid in the treatment of psoriasis in comparison with betamethasone valerate (another common analogue of betamethasone) which is rated as upper mid-strength.1 This application brief describes the use of a Quasar C18 column for Solvents and Samples the analysis of betamethasone dipropionate (Figure 1) in accordance All solvents were HPLC grade and samples were filtered using with the official USP monograph.2 0.45 μm PTFE filter, p/n: 02542909. Two stock solutions were prepared in acetic acid and methanol (1 in 1000) using USP betamethasone dipropionate (0.6 mg/mL) and USP beclomethasone dipropionate (0.9 mg/mL) as an internal standard. The standard solution was prepared by combining solutions, in equal parts as specified by the USP monograph, to concentrations of 0.3 mg/mL and 0.45 mg/mL respectively. Results and Discussion The USP method estimates the elution times of betamethasone and beclomethasone to be 14 and 18 minutes respectively under the specified conditions, using a column of L1 packing (300 mm x 4.0 mm). -

Pharmacology for Preterm Labor Lindsey Garfield, Phd; Emily Chin, Phd
DOI: 10.1097/JPN.0000000000000474 Continuing Education r r J Perinat Neonat Nurs Volume 34 Number 2, 155–161 Copyright C 2020 Wolters Kluwer Health, Inc. All rights reserved. Pharmacology for Preterm Labor Lindsey Garfield, PhD; Emily Chin, PhD ABSTRACT includes uterine contractions with accompanying cer- Preterm birth occurs with 10% of deliveries and yet ac- vical dilation greater than 2 cm or changes in dilation counts for more than 85% of perinatal morbidity and mor- or effacement.3 Many women presenting with preterm tality. Management of preterm labor prior to delivery in- labor will give birth at term (50%); in addition, 30% cludes a multipronged pharmacologic approach targeting of preterm labor resolves spontaneously.4,5 Preterm la- utilization of reproductive hormones for continuation of bor is generally not treated prior to neonatal viabil- pregnancy, advancement of fetal lung maturity, and the ity and only when delay of neonatal birth will benefit decrease of uterine contractility (tocolysis). This article will the newborn.3 Current pharmacologic management for review and compare guidelines on pharmacologic manage- premature labor consists of advancing fetal lung ma- ment of preterm labor as recommended by the American turity, decreasing uterine contractility, and utilizing re- College of Obstetricians and Gynecologists and the Euro- productive hormones for continuation of pregnancy.6 pean Association of Perinatal Medicine. The classifications Guidelines on the use of pharmacologic management of drugs discussed include exogenous progesterone, of preterm labor are disputed among obstetricians corticosteroids, and tocolytics (β-adrenergic agonists, mag- throughout the world and professional organizations nesium sulfate, calcium channel blockers, prostaglandin have established various guidelines for practice.6–8 This inhibitors, nitrates, and oxytocin receptor blockers). -

Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Psoriasis
Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Psoriasis Diagnosis: PSORIASIS TREATMENT RECOMMENDATIONS: • Careful physical exam for possible strep infection (throat, perianal area, inguinal folds) and treatment if positive. • Careful history for persistent or frequent history of morning stiffness or joint pain Location Eyelids Elidel 1% cream (or other calcineurin inhibitor) Face, Axillae, Hydrocortisone 2.5% ointment (or other Class 6 or 7 topical steroid) Inguinal Folds Body Thin/mild: Triamcinolone 0.1% ointment (or other Class 3, 4 topical steroid) Thick/severe: Mometasone 0.1% ointment (or other Class 1 or 2 topical steroid) Scalp Mild (or patients with dry hair): Fluocinolone 0.01% (Derma-smoothe) oil Severe: Clobetasol 0.05 % solution Shampoo: (over-the-counter) • Salicylic acid containing shampoo (e.g. T sal shampoo) • Tar containing shampoo (e.g. T gel shampoo) • Baker’s P&S shampoo Nails Mometasone 0.1% ointment (or other Class 1 or 2 topical steroid) • Apply medication to nail folds/cuticle PATIENT RESOURCES: National Psoriasis Foundation www.psoriasis.org REFERRAL RECOMMENDATIONS: • Please refer patient if there is extensive involvement (>5-10% BSA), or localiZed involvement that has failed treatment recommendations above. • If patient has persistent morning stiffness or joint complaints, please also refer to rheumatology for evaluation for possible psoriatic arthritis Educational recommendations are made from the best evidence, expert opinions and consideration for the patients and families cared for by the service. This is NOT intended to impose standards of care preventing selective variation in practice that are necessary to meet the unique needs of individual patients. The physician must consider each patient’s circumstance to make the ultimate judgment regarding best care.