The History of Traumatology and Orthopaedics Development
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lameness in Fattening Pigs – Mycoplasma Hyosynoviae, Osteochondropathy and Reduced Dietary Phosphorus Level As Three Infuencing Factors: a Case Report
Lameness in fattening pigs – Mycoplasma hyosynoviae, osteochondropathy and reduced dietary phosphorus level as three inuencing factors: A case report Birte Wegner Veterinary Practice Duemmerland Jörg Tenhündfeld Vetland Dr. Tenhündfeld & Kollegen Johanna Vogels Stiftung Tierarztliche Hochschule Hannover Marius Beumer Stiftung Tierarztliche Hochschule Hannover Josef Kamphues Stiftung Tierarztliche Hochschule Hannover Florian Hansmann Stiftung Tierarztliche Hochschule Hannover Hanna Rieger Stiftung Tierarztliche Hochschule Hannover Elisabeth grosse Beilage Stiftung Tierarztliche Hochschule Hannover Isabel Hennig-Pauka ( [email protected] ) University of Veterinary Medicine Hannover https://orcid.org/0000-0003-3994-5979 Case report Keywords: Locomotor disorder, mineral supply, Mycoplasma hyosynoviae, nutrition, swine Posted Date: September 25th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-35962/v2 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/28 Version of Record: A version of this preprint was published on December 15th, 2020. See the published version at https://doi.org/10.1186/s40813-020-00184-w. Page 2/28 Abstract Background: Multiple diagnostic procedures, their results and interpretation in a case with severe lameness in fattening pigs are described. It is shown that selected diagnostic steps lead to identication of various risk factors for disease development in the affected herd. One focus of this case report is the prioritization of diagnostic steps to verify the impact of the different conditions, which nally led to the clinical disorder. Disease is the consequence of previously acting factors, and the involved diagnostic institute is the last stage in the timeline. Some diagnostic ndings might therefore no longer be signicant. -

Pediatrics-EOR-Outline.Pdf
DERMATOLOGY – 15% Acne Vulgaris Inflammatory skin condition assoc. with papules & pustules involving pilosebaceous units Pathophysiology: • 4 main factors – follicular hyperkeratinization with plugging of sebaceous ducts, increased sebum production, Propionibacterium acnes overgrowth within follicles, & inflammatory response • Hormonal activation of pilosebaceous glands which may cause cyclic flares that coincide with menstruation Clinical Manifestations: • In areas with increased sebaceous glands (face, back, chest, upper arms) • Stage I: Comedones: small, inflammatory bumps from clogged pores - Open comedones (blackheads): incomplete blockage - Closed comedones (whiteheads): complete blockage • Stage II: Inflammatory: papules or pustules surrounded by inflammation • Stage III: Nodular or cystic acne: heals with scarring Differential Diagnosis: • Differentiate from rosacea which has no comedones** • Perioral dermatitis based on perioral and periorbital location • CS-induced acne lacks comedones and pustules are in same stage of development Diagnosis: • Mild: comedones, small amounts of papules &/or pustules • Moderate: comedones, larger amounts of papules &/or pustules • Severe: nodular (>5mm) or cystic Management: • Mild: topical – azelaic acid, salicylic acid, benzoyl peroxide, retinoids, Tretinoin topical (Retin A) or topical antibiotics [Clindamycin or Erythromycin with Benzoyl peroxide] • Moderate: above + oral antibiotics [Minocycline 50mg PO qd or Doxycycline 100 mg PO qd], spironolactone • Severe (refractory nodular acne): oral -

Frequency and Criticality of Diagnoses in Family Medicine Practices: from the National Ambulatory Medical Care Survey (NAMCS)
J Am Board Fam Med: first published as 10.3122/jabfm.2018.01.170209 on 12 January 2018. Downloaded from ORIGINAL RESEARCH Frequency and Criticality of Diagnoses in Family Medicine Practices: From the National Ambulatory Medical Care Survey (NAMCS) Michael R. Peabody, PhD, Thomas R. O’Neill, PhD, Keith L. Stelter, MD, MMM, and James C. Puffer, MD Background: Family medicine is a specialty of breadth, providing comprehensive health care for the individual and the family that integrates the broad scope of clinical, social, and behavioral sciences. As such, the scope of practice (SOP) for family medicine is extensive; however, over time many family phy- sicians narrow their SOP. We sought to provide a nationally representative description of the most com- mon and the most critical diagnoses that family physicians see in their practice. Methods: Data were extracted from the 2012 National Ambulatory Medical Care Survey (NAMCS) to select all ICD-9 codes reported by family physicians. A panel of family physicians then reviewed 1893 ICD-9 codes to place each code into an American Board of Family Medicine Family Medicine Certifica- tion Examination test plan specifications (TPS) category and provide a rating for an Index of Harm (IoH). Results: An analysis of all 1893 ICD-9 codes seen by family physicians in the 2012 NAMCS found that 198 ICD-9 codes could not be assigned a TPS category, leaving 1695 ICD-9 codes in the dataset. Top 10 lists of ICD-9 codes by TPS category were created for both frequency and IoH. Conclusions: This study provides a nationally representative description of the most common diag- copyright. -

Code Description
Code Description 0061 Chronic intestinal amebiasis without mention of abscess 0062 Amebic nondysenteric colitis 0063 Amebic liver abscess 0064 Amebic lung abscess 00642 West Nile fever with other neurologic manifestation 00649 West Nile fever with other complications 0065 Amebic brain abscess 0066 Amebic skin ulceration 0068 Amebic infection of other sites 0069 Amebiasis, unspecified 0070 Other protozoal intestinal diseases, balantidiasis (Infection by Balantidium coli) 0071 Other protozoal intestinal diseases, giardiasis 0072 Other protozoal intestinal diseases, coccidiosis 0073 Other protozoal intestinal diseases, trichomoniasis 0074 Other protozoal intestinal diseases, cryptosporidiosis 0075 Other protozoal intestional disease cyclosporiasis 0078 Other specified protozoal intestinal diseases 0079 Unspecified protozoal intestinal disease 01000 Primary tuberculous infection, unspecified 01001 Primary tuberculous infection bacteriological or histological examination not done 01002 Primary tuberculous infection, bacteriological or histological examination results unknown 01003 Primary tuberculous infection, tubercle bacilli found by microscopy 01004 Primary tuberculous infection, tubercle bacilli found by bacterial culture 01005 Primary tuberculous infection, tubercle bacilli confirmed histolgically 01006 Primary tuberculous infection, tubercle bacilli found by other methods 01010 Tuberculous pleurisy in primary progressive tuberculosis unspecified 01011 Tuberculous pleurisy bacteriological or histological examination not done 01012 Tuberculous -

Download PDF File
Folia Morphol. Vol. 79, No. 1, pp. 1–14 DOI: 10.5603/FM.a2019.0047 R E V I E W A R T I C L E Copyright © 2020 Via Medica ISSN 0015–5659 journals.viamedica.pl Should Terminologia Anatomica be revised and extended? A critical literature review P.P. Chmielewski1, B. Strzelec2, 3 1Division of Anatomy, Department of Human Morphology and Embryology, Faculty of Medicine, Wroclaw Medical University, Wroclaw, Poland 2Department and Clinic of Vascular, General and Transplantation Surgery, Jan Mikulicz-Radecki Medical University Hospital, Wroclaw Medical University, Wroclaw, Poland 3Department and Clinic of Gastrointestinal and General Surgery, Wroclaw Medical University, Wroclaw, Poland [Received: 14 November 2018; Accepted: 31 December 2018] The first edition of the Terminologia Anatomica was published in 1998 by the Federative Committee for Anatomical Terminology, whereas the second edition was issued in 2011 by the Federative International Programme for Anatomical Terminologies. Since then many attempts have been made to revise and extend the official terminology as several inconsistencies have been noted. Moreover, numerous crucial terms were either omitted or deliberately excluded from the official terminology, like sulcus popliteus and diaphragma urogenitale, respec- tively. Furthermore, several synonyms are to be discarded. Notwithstanding the criticism, the use of the current version of terminology is strongly recommended. Although the Terminologia Anatomica is open to future expansion and revision, every change should be made after a thorough discussion of the historical context and scientific legitimacy of a given term. The anatomical nomenclature must be as simple as possible but also precise and coherent. It is generally accepted that hasty innovation ought not to be endorsed. -
Prezentacja Programu Powerpoint
Department of Human Anatomy. Medical University of Białystok Beata Klim Gluteal region It lies posterior to the pelvis between the level of the iliac crests and the inferior borders of the gluteus maximus muscles. The intergluteal (natal) cleft separates the buttocks from each other. The gluteal sulcus demarcates the inferior boundary of the buttock and the superior boundary of the thigh. Gluteal region The gluteal muscles (maximus, medius and minimus) form the bulk of the buttock. Pelvic girdle- muscles The anterior compartment: Psoas major Psoas minor Iliacus They are called - Iliopsoas Iliopsoas Proximal attachments: Psoas major- sides of T12-L5 vertebrae & discs between them; transverse processes of all lumbar vertebrae Psoas minor- sides of T12-L1 & intervertebral disc Iliacus- iliac crest, iliac fossa, ala of sacrum & anterior sacroiliac ligaments Iliopsoas Distal attachments: Psoas major- lesser trochanter of femur Psoas minor- pectineal line, iliopectineal eminence via iliopectineal arch Iliacus- tendon of psoas major, lesser trochanter, and femur distal to it Iliopsoas Innervation: Psoas major- ventral rami of lumbar nerves L1, L2, L3 Psoas minor- ventral rami of lumbar nerves L1, L2 Iliacus- femoral nerve L2, L3 Iliopsoas Main action: It is the chief flexor of the thigh, and when the thigh is fixed, it flexes the trunk on the hip. It is also a postural muscle that is active during standing by preventing hyperextension of the hip joint. The gluteal muscles The gluteal muscles consist of: Three large glutei (maximus, medius & minimus), which are mainly extensors and abductors of the thigh. A deeper group of smaller muscles (piriformis, obturator internus, obturator externus, gemelli and quadratus femoris), which are covered by the inferior part of the gluteus maximus. -

1 Ministry of Health of Ukraine National O.O. Bogomolets Medical
Ministry of Health of Ukraine National O.O. Bogomolets Medical University “APPROVED” At the staff meeting of the Department of pediatrics №4 Chief of the Department of Pediatrics №4 Academician, Professor, MD, PhD Maidannyk V.G. __________________________(Signature) “_____” ___________________ 2019 y. Methodological recommendations for students Subject Pediatrics Module 1 Pediatrics PERIODS OF CHILDHOOD Topic Course 3 Faculty Medical №2 Kyiv -2019 1 Authorship TEAM OF SPECIALISTS OF THE DEPARTMENT OF PEDIATRICS №4 NATIONAL MEDICAL O.O. Bogomolets UNIVERSITY HEAD OF THE DEPARTMENT - DOCTOR OF MEDICAL SCIENCES, MD, PhD, ACADEMICIAN of the NAMS of Ukraine PROFESSOR V.G. Maidannyk., MD, PhD, ASSOCIATE PROFESSOR Ie.A. Burlaka; MD, PhD, ASSOCIATE PROFESSOR R.V. Terletskiy, MD, PhD Assistamt T.D. Klec. PERIODS OF CHILDHOOD Topic relevance. Child's organism is constantly changing in the process of individual development, and different systems and organs formation takes place at definite time. Childhood periodization is the chronological basis for studying and un- derstanding the regularities of child's growing up and developing, as well as the peculiarities of their morbidity depending on their age. The aim of the lesson: to study the chronological structure of child's age, to study the peculiarities of children's growing, development and morbidity at different age. Follow-up questions: 1. Different childhood periods chronology, critical periods. 2. Peculiarities of all critical childhood periods. 3. Peculiarities of the newborn's organism and transitory states of the newborn period. 4. Morbidity peculiarities at different childhood periods. Having covered the topic, the student should be able to: 1. Define the periods of children's age. -

Plastic Surgery and Modern Techniques Abulezz T
Plastic Surgery and Modern Techniques Abulezz T. Plast Surg Mod Tech 6: 147. Review Article DOI: 10.29011/2577-1701.100047 A Review of Recent Advances in Aesthetic Gluteoplasty and Buttock Contouring Tarek Abulezz* Department of plastic surgery, Faculty of Medicine, Sohag University, Sohag, Egypt *Corresponding author: Tarek Abulezz, Department of plastic surgery, Faculty of Medicine, Sohag University, Sohag, Egypt. Tel: +20-1003674340; Email: [email protected] Citation: Abulezz T (2019) A Review of Recent Advances in Aesthetic Gluteoplasty and Buttock Contouring. Plast Surg Mod Tech 6: 147. DOI: 10.29011/2577-1701.100047 Received Date: 20 June, 2019; Accepted Date: 03 July, 2019; Published Date: 11 July, 2019 Introduction Infragluteal fold: a horizontal crease arising from the median gluteal crease and runs laterally under the ischial tuberosity with a A well-developed buttock is a peculiar trait of the human, slight upward concavity. and not seen in the other primates [1]. The buttock is an extremely important area in woman’s sexuality and is considered a cornerstone Supragluteal fossettes: two hollows located on either side of the of female beauty. Although the concept of female beauty has medial sacral crest. They are formed by the posterior superior iliac changed over time, there are two constant items of femininity: spine and medially by the multifidus muscle. the breasts and the buttocks [2,3]. However, the parameters of V-shaped crease: two lines arising in the upper portion of the beautiful buttocks have varied according to time, culture, and gluteal crease toward the supragluteal fossettes. ethnicity [4,5]. Increasing number of patients are asking for esthetic improvement of their buttock profile or for correction of a Lumbar hyperlordosis is an additional feature that may deformity or irregularity. -

Exome Sequencing Reveals a Phenotype Modifying Variant in ZNF528 in Primary Osteoporosis with a COL1A2 Deletion
ORIGINAL ARTICLE Exome Sequencing Reveals a Phenotype Modifying Variant in ZNF528 in Primary Osteoporosis With a COL1A2 Deletion Sini Skarp,1,2,3† Ji-Han Xia,2,4† Qin Zhang,2,4 Marika Löija,2,3 Alice Costantini,5 Lloyd W Ruddock,2 Outi Mäkitie,5,6,7,8,9 Gong-Hong Wei,2,4,10† and Minna Männikkö1,3† 1Infrastructure for Population Studies, Northern Finland Birth Cohorts, Faculty of Medicine, University of Oulu, Oulu, Finland 2Faculty of Biochemistry and Molecular Medicine, University of Oulu, Oulu, Finland 3Center for Life Course Health Research, Faculty of Medicine, University of Oulu, Oulu, Finland 4Biocenter Oulu, University of Oulu, Oulu, Finland 5Department of Molecular Medicine and Surgery and Center for Molecular Medicine, Karolinska Institutet/Stockholm, Stockholm, Sweden 6Department of Clinical Genetics, Karolinska University Hospital, Stockholm, Sweden 7Children’s Hospital and Pediatric Research Center, University of Helsinki and Helsinki University Hospital, Helsinki, Finland 8Folkhälsan Research Center, Genetics Research Program, Helsinki, Finland 9Research Program for Clinical and Molecular Metabolism, Faculty of Medicine, University of Helsinki, Helsinki, Finland 10Department of Biochemistry and Molecular Biology, School of Basic Medical Sciences and Zhongshan Hospital, Fudan University, Shanghai, China ABSTRACT We studied a family with severe primary osteoporosis carrying a heterozygous p.Arg8Phefs*14 deletion in COL1A2, leading to hap- loinsufficiency. Three affected individuals carried the mutation and presented nearly identical spinal fractures but lacked other typical features of either osteogenesis imperfecta or Ehlers-Danlos syndrome. Although mutations leading to haploinsufficiency in COL1A2 are rare, mutations in COL1A1 that lead to less protein typically result in a milder phenotype. -

Osteochondral Allograft/Autograft Transplantation (OAT) Health Technology Assessment
WA Health Technology Assessment - HTA WASHINGTON STATE HEALTH CARE AUTHORITY Osteochondral Allograft/Autograft Transplantation (OAT) Health Technology Assessment Monday, October 17, 2011 Health Technology Assessment Program 676 Woodland Square Loop SE P.O. Box 42712 Olympia, WA 98504-2712 http://www.hta.hca.wa.gov WA Health Technology Assessment - HTA Osteochondral Allograft/Autograft Transplantation (OAT) Provided by: Spectrum Research, Inc. Prepared by: Andrea C. Skelly, PhD, MPH Erika D. Ecker, BS Jeannette M. Schenk‐Kisser, PhD, MS Barbara C. Leigh, PhD, MPH Annie Raich, MS, MPH With assistance from Robin E. Hashimoto, PhD Jeffrey T. Hermsmeyer, BA WA Health Technology Assessment: OATS (10-17-2011) Page 2 of 168 WA Health Technology Assessment - HTA This technology assessment report is based on research conducted by a contracted technology assessment center, with updates as contracted by the Washington State Health Care Authority. This report is an independent assessment of the technology question(s) described based on accepted methodological principles. The findings and conclusions contained herein are those of the investigators and authors who are responsible for the content. These findings and conclusions may not necessarily represent the views of the HCA/Agency and thus, no statement in this report shall be construed as an official position or policy of the HCA/Agency. The information in this assessment is intended to assist health care decision makers, clinicians, patients and policy makers in making sound evidence‐based decisions that may improve the quality and cost‐ effectiveness of health care services. Information in this report is not a substitute for sound clinical judgment. Those making decisions regarding the provision of health care services should consider this report in a manner similar to any other medical reference, integrating the information with all other pertinent information to make decisions within the context of individual patient circumstances and resource availability. -
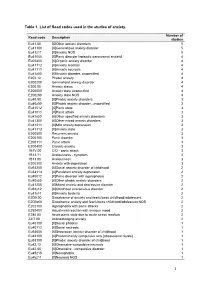
1 Table 1. List of Read Codes Used in the Studies of Anxiety
Table 1. List of Read codes used in the studies of anxiety. Number of Read code Description studies Eu41.00 [X]Other anxiety disorders 5 Eu41100 [X]Generalized anxiety disorder 5 Eu41z11 [X]Anxiety NOS 5 Eu41000 [X]Panic disorder [episodic paroxysmal anxiety] 4 Eu05400 [X]Organic anxiety disorder 4 Eu41112 [X]Anxiety reaction 4 Eu41111 [X]Anxiety neurosis 4 Eu41z00 [X]Anxiety disorder, unspecified 4 E202.12 Phobic anxiety 4 E200200 Generalised anxiety disorder 4 E200.00 Anxiety states 4 E200000 Anxiety state unspecified 4 E200z00 Anxiety state NOS 4 Eu40.00 [X]Phobic anxiety disorders 3 Eu40z00 [X]Phobic anxiety disorder, unspecified 3 Eu41012 [X]Panic state 3 Eu41011 [X]Panic attack 3 Eu41y00 [X]Other specified anxiety disorders 3 Eu41300 [X]Other mixed anxiety disorders 3 Eu41211 [X]Mild anxiety depression 3 Eu41113 [X]Anxiety state 3 E200500 Recurrent anxiety 3 E200100 Panic disorder 3 E200111 Panic attack 3 E200400 Chronic anxiety 3 1B1V.00 C/O - panic attack 3 1B13.11 Anxiousness - symptom 3 1B13.00 Anxiousness 3 E200300 Anxiety with depression 3 Eu93200 [X]Social anxiety disorder of childhood 2 Eu34114 [X]Persistant anxiety depression 2 Eu40012 [X]Panic disorder with agoraphobia 2 Eu40y00 [X]Other phobic anxiety disorders 2 Eu41200 [X]Mixed anxiety and depressive disorder 2 Eu93y12 [X]Childhood overanxious disorder 2 Eu41y11 [X]Anxiety hysteria 2 E2D0.00 Disturbance of anxiety and fearfulness childhood/adolescent 2 E2D0z00 Disturbance anxiety and fearfulness childhood/adolescent NOS 2 E202100 Agoraphobia with panic attacks 2 E292400 -

“To Assess the Efficacy of Anterior Approach to Both
A Dissertation on “TO ASSESS THE EFFICACY OF ANTERIOR APPROACH TO BOTH FEMORAL AND SCIATIC NERVE VIA A SINGLE SKIN SITE INJECTION TECHNIQUE vs CLASSICAL TWO SITE INJECTION TECHNIQUE USING NERVE LOCATOR FOR LOWER LIMB SURGERY” Submitted to the THE TAMILNADU DR. M.G.R. MEDICAL UNIVERSITY In partial fulfilment of the requirements For the award of degree of M.D. (Branch-X) ANAESTHESIOLOGY GOVERNMENT STANLEY MEDICAL COLLEGE & HOSPITAL THE TAMILNADU DR. M.G.R. MEDICAL UNIVERSITY, CHENNAI, TAMILNADU APRIL 2013 CERTIFICATE This is to certify that this dissertation entitled “TO ASSESS THE EFFICACY OF ANTERIOR APPROACH TO BOTH FEMORAL AND SCIATIC NERVE VIA A SINGLE SKIN SITE INJECTION TECHNIQUE vs CLASSICAL TWO SITE INJECTION TECHNIQUE USING NERVE LOCATOR FOR LOWER LIMB SURGERY”, Submitted by DR.GIRISH.B.K to the faculty of ANAESTHESIOLOGY, The Tamil Nadu Dr. M.G.R. Medical University, Chennai, in partial fulfillment of the requirement in the award of degree of M.D. Degree, Branch - X (ANAESTHESIOLOGY), for the April 2013 examination is a bonafide research work carried out by him during the period of November 2011 to May 2012 at Government Stanley Medical College and Hospital, Chennai under our direct supervision and guidance of Dr. KUMUDHA LINGARAJ, Professor, Department of Anaesthesiology at Stanley Medical College, Chennai. Prof. Dr .KUMUDHA LINGARAJ, Prof. Dr. P. CHANDRASEKAR, M.D., D.A., M.D., D.A., Professor, Guide, Professor and H.O.D. Department of Anaesthesiology, Department of Anaesthesiology Stanley Medical College and Hospital, Stanley Medical College Chennai – 600 001. and Hospital, Chennai – 600 001. Prof . Dr. GEETHA LAKSHMI, M.D, Ph.D Dean Government Stanley Medical College, Chennai – 600001.