Osteochondral Allograft/Autograft Transplantation (OAT) Health Technology Assessment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lameness in Fattening Pigs – Mycoplasma Hyosynoviae, Osteochondropathy and Reduced Dietary Phosphorus Level As Three Infuencing Factors: a Case Report
Lameness in fattening pigs – Mycoplasma hyosynoviae, osteochondropathy and reduced dietary phosphorus level as three inuencing factors: A case report Birte Wegner Veterinary Practice Duemmerland Jörg Tenhündfeld Vetland Dr. Tenhündfeld & Kollegen Johanna Vogels Stiftung Tierarztliche Hochschule Hannover Marius Beumer Stiftung Tierarztliche Hochschule Hannover Josef Kamphues Stiftung Tierarztliche Hochschule Hannover Florian Hansmann Stiftung Tierarztliche Hochschule Hannover Hanna Rieger Stiftung Tierarztliche Hochschule Hannover Elisabeth grosse Beilage Stiftung Tierarztliche Hochschule Hannover Isabel Hennig-Pauka ( [email protected] ) University of Veterinary Medicine Hannover https://orcid.org/0000-0003-3994-5979 Case report Keywords: Locomotor disorder, mineral supply, Mycoplasma hyosynoviae, nutrition, swine Posted Date: September 25th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-35962/v2 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/28 Version of Record: A version of this preprint was published on December 15th, 2020. See the published version at https://doi.org/10.1186/s40813-020-00184-w. Page 2/28 Abstract Background: Multiple diagnostic procedures, their results and interpretation in a case with severe lameness in fattening pigs are described. It is shown that selected diagnostic steps lead to identication of various risk factors for disease development in the affected herd. One focus of this case report is the prioritization of diagnostic steps to verify the impact of the different conditions, which nally led to the clinical disorder. Disease is the consequence of previously acting factors, and the involved diagnostic institute is the last stage in the timeline. Some diagnostic ndings might therefore no longer be signicant. -

Frequency and Criticality of Diagnoses in Family Medicine Practices: from the National Ambulatory Medical Care Survey (NAMCS)
J Am Board Fam Med: first published as 10.3122/jabfm.2018.01.170209 on 12 January 2018. Downloaded from ORIGINAL RESEARCH Frequency and Criticality of Diagnoses in Family Medicine Practices: From the National Ambulatory Medical Care Survey (NAMCS) Michael R. Peabody, PhD, Thomas R. O’Neill, PhD, Keith L. Stelter, MD, MMM, and James C. Puffer, MD Background: Family medicine is a specialty of breadth, providing comprehensive health care for the individual and the family that integrates the broad scope of clinical, social, and behavioral sciences. As such, the scope of practice (SOP) for family medicine is extensive; however, over time many family phy- sicians narrow their SOP. We sought to provide a nationally representative description of the most com- mon and the most critical diagnoses that family physicians see in their practice. Methods: Data were extracted from the 2012 National Ambulatory Medical Care Survey (NAMCS) to select all ICD-9 codes reported by family physicians. A panel of family physicians then reviewed 1893 ICD-9 codes to place each code into an American Board of Family Medicine Family Medicine Certifica- tion Examination test plan specifications (TPS) category and provide a rating for an Index of Harm (IoH). Results: An analysis of all 1893 ICD-9 codes seen by family physicians in the 2012 NAMCS found that 198 ICD-9 codes could not be assigned a TPS category, leaving 1695 ICD-9 codes in the dataset. Top 10 lists of ICD-9 codes by TPS category were created for both frequency and IoH. Conclusions: This study provides a nationally representative description of the most common diag- copyright. -

The Oregon Journal of Orthopaedics
OJO The Oregon Journal of Orthopaedics Volume II May 2013 JUST WHEN YOU THOUGHT BIOMET KNEE IMPLANTS COULDN’T GET ANY BETTER. THE INDUSTRY’S ONLY LIFETIME KNEE IMPLANT REPLACEMENT WARRANTY† IN THE U.S. This’ll make you feel good. Every Oxford® Partial Knee used with Signature™* technology now comes with Biomet’s Lifetime Knee Implant Replacement Warranty.† It’s the first knee replacement warranty† of its kind in the U.S. – and just one more reason to choose a partial knee from Biomet. Other reasons include a faster recovery with less pain and more natural motion.** And now, the Oxford® is available with Signature™ personalized implant positioning for a solution that’s just for you. Who knew a partial knee could offer so much? ® 800.851.1661 I oxfordknee.com Risk Information: Not all patients are candidates for partial knee replacement. Only your orthopedic surgeon can tell you if you’re a candidate for joint replacement surgery, and if so, which implant is right for your specific needs. You should discuss your condition and treatment options with your surgeon. The Oxford® Meniscal Partial Knee is intended for use in individuals with osteoarthritis or avascular necrosis limited to the medial compartment of the knee and is intended to be implanted with bone cement. Potential risks include, but are not limited to, loosening, dislocation, fracture, wear, and infection, any of which can require additional surgery. For additional information on the Oxford® knee and the Signature™ system, including risks and warnings, talk to your surgeon and see the full patient risk information on oxfordknee.com and http://www.biomet.com/orthopedics/getFile.cfm?id=2287&rt=inline or call 1-800-851-1661. -

Microfracture Surgery Improves Knee Function
March 2006 • www.rheumatologynews.com Arthritis 19 Microfracture Surgery Improves Knee Function BY DOUG BRUNK the mean Lysholm scores improved from strenuous sports activities, we found they tissue at a level adjacent with normal ar- San Diego Bureau 57 to 87; the Tegner scores improved from increased to 80% in the first 2 years but ticular surface and were firm when pal- 3 to 5; and the subjective evaluation im- then gradually decreased to 55% at final pated with a probe. Biopsies from these S AN D IEGO — Microfracture as a treat- proved from 40/100 to 70/100. At base- follow-up,” Dr. Gobbi added. Changing to same 10 patients showed areas of fi- ment for full thickness chondral lesions line, only three patients scored an A or B a low-risk sport, advancing age of the bromyxoid tissue with differentiation, a provided functional improvement in a on the IKDC, but by final follow-up, 70% study participants, work and family oblig- transition zone with cartilage tissue, and group of professional and recreational of patients scored an A or B. ations, and the influence of degenerative initial hyaline transformation tissue. athletes at 6-year follow-up, but the level Also by final follow-up, activities of dai- joint disease may have contributed to the Candidates should be evaluated by age, of postoperative sports participation de- ly living improved in 65% of patients while decline in postsurgical sports activity. activity level, type of sport, type of injury, clined with time, Dr. Alberto Gobbi re- imaging studies revealed increased de- Second-look arthroscopy performed in expectations, associated pathologies, like- ported at a symposium sponsored by the generative changes in 30% of patients. -

Chicago – USA May 8 – 11, 2015 12 Th World Congress of the International Cartilage Repair Society
2 015 #ICRS15 Chicago – USA May 8 – 11, 2015 12 th World Congress of the International Cartilage Repair Society Main Programme & Extended Abstracts www.cartilage.org 21 AMA PRA Categorie 1 Credits Diamond Partner Platinum Sponsor Gold Sponsor Silver Sponsors 1 Invited Abstracts 1.1.2 in preshaped plugs 10 lengths in diameters of 7, 9, 11 and 15mm. Chondrofix® Osteochondral Allograft does not have the issue of a Allografts & Autogenous OsteoChondral Technologies waiting time as it is truly off-the-shelf. Chondrofix® is donated hu- J. Farr man tissue that is decellularized; that is, the hyaline cartilage and Greenwood/United States of America cancellous bone are delivered acellular but have mechanical proper- ties that are similar to unprocessed osteochondral tissue. The graft Introduction: Osteochondral grafts have been an important part undergoes a proprietary processing protocol, which includes lipid of the clinician’s armamentarium when treating cartilage lesion for removal, viral inactivation with methylene blue photoactivation and many years. The current issues are: identifying the best applications, terminal sterilization with low temperature low dose gamma irradia- refining the technique and optimizing the use of these tissues. While tion. Chondrofix® is currently available and being actively implanted the algorithm for cartilage restoration will continue to evolve, there in the US, noting there are no published clinical studies on this will remain overlap of the available applications with autograft and unique allograft application. Another acellular approach is frozen allograft continuing to play substantial roles. The amount of availa- osteochondral allograft. The cartilage chondrocytes are not reliably ble tissue for both autograft and allograft is limited, so creative solu- viable upon thawing and thus the matrix is not well-maintained over tions for optimizing tissue use are essential. -

Microfracture of Knee Joint
Microfracture of Knee Joint Post-op Precautions : The patient will ambulate with crutches for 4 weeks or more after surgery. The physician will base weight- bearing status upon the location of the lesion. Phase I (1 – 5 days post-op) • Wound care: Observe for signs of infection • Gait: WB will vary by the size of the lesion and the location. See physician prescription. The patient will typically be NWB for femoral condyle lesions and TTWB (25%) for patellofemoral lesions. • Modalities: prn for pain and inflammation (ice, IFC) • Brace: Used for patellofemoral lesions locked for WB. • ROM: 0 – 90 degrees o Passive positional stretches for extension and flexion o CPM as prescribed by physician o Ankle AROM Phase II (5 days – 4 weeks post-op) • Wound care: Observe for signs of infection and begin scar management techniques when incision is closed • Gait: o Femoral condyle lesions: Initially NWB; s/p 2 weeks increase to TTWB; s/p week 3 then increase to 25% WB o Patellofemoral lesions: Initially TTWB; At s/p week 1 increase 25% per week o Initiate wt shifting activities as soon as WB status allows • Brace: if used, locked for WB • ROM: o Minimum Goals: • Week 1: 0 – 90 degrees • Week 2: 0 – 105 degrees • Week 3: 0 – 115 degrees • Week 4: 0 – 125 degrees o Stationary bike at 3 to 4 weeks o PROM for flexion with no limits unless painful o Increase / maintain patellar mobility with emphasis on superior glide o Hamstring, gastrocnemius, soleus, and hip flexor stretches • Strengthening: o Multiangle Quad and Hamstring sets o 4 way SLR o Calf raises -

Autologous Chondrocyte Implantation (ACI) for Cartilaginous Defects
MEDICAL POLICY Knee: Autologous Chondrocyte Implantation (ACI) for Cartilaginous Defects Effective Date: 10/1/2021 Medical Policy Number: 137 Technology Assessment Committee Approved Date: 4/10; 5/12; 7/14; 6/15 Medical Policy Committee Approved Date: 2/11; 2/12; 7/13; 3/16; 4/17; 6/18; 1/19; 2/2020; 8/2020; 9/2021 10/1/2021 Medical Officer Date See Policy CPT/HCPCS CODE section below for any prior authorization requirements SCOPE: Providence Health Plan, Providence Health Assurance, Providence Plan Partners, and Ayin Health Solutions as applicable (referred to individually as “Company” and collectively as “Companies”). APPLIES TO: All lines of business BENEFIT APPLICATION Medicaid Members Oregon: Services requested for Oregon Health Plan (OHP) members follow the OHP Prioritized List and Oregon Administrative Rules (OARs) as the primary resource for coverage determinations. Medical policy criteria below may be applied when there are no criteria available in the OARs and the OHP Prioritized List. POLICY CRITERIA I. Autologous chondrocyte implantation (ACI) may be considered medically necessary and covered for the treatment of single or multiple symptomatic articular cartilage defects of the knee (medial, lateral or trochlear femoral condyle, or patella) when ALL of the following criteria (A. – I.) are met: A. Age 18-55 years (adolescents must have closed growth plates); and B. Body mass index (BMI) of <35; and C. Symptoms from acute or chronic trauma interfere with age-appropriate activities of daily living; and D. Symptoms have failed to improve after 3 months of conservative treatment, including physical therapy, as part of pre-operative planning for surgery; and E. -

Code Description
Code Description 0061 Chronic intestinal amebiasis without mention of abscess 0062 Amebic nondysenteric colitis 0063 Amebic liver abscess 0064 Amebic lung abscess 00642 West Nile fever with other neurologic manifestation 00649 West Nile fever with other complications 0065 Amebic brain abscess 0066 Amebic skin ulceration 0068 Amebic infection of other sites 0069 Amebiasis, unspecified 0070 Other protozoal intestinal diseases, balantidiasis (Infection by Balantidium coli) 0071 Other protozoal intestinal diseases, giardiasis 0072 Other protozoal intestinal diseases, coccidiosis 0073 Other protozoal intestinal diseases, trichomoniasis 0074 Other protozoal intestinal diseases, cryptosporidiosis 0075 Other protozoal intestional disease cyclosporiasis 0078 Other specified protozoal intestinal diseases 0079 Unspecified protozoal intestinal disease 01000 Primary tuberculous infection, unspecified 01001 Primary tuberculous infection bacteriological or histological examination not done 01002 Primary tuberculous infection, bacteriological or histological examination results unknown 01003 Primary tuberculous infection, tubercle bacilli found by microscopy 01004 Primary tuberculous infection, tubercle bacilli found by bacterial culture 01005 Primary tuberculous infection, tubercle bacilli confirmed histolgically 01006 Primary tuberculous infection, tubercle bacilli found by other methods 01010 Tuberculous pleurisy in primary progressive tuberculosis unspecified 01011 Tuberculous pleurisy bacteriological or histological examination not done 01012 Tuberculous -

Failure of Bone Marrow Stimulation Techniques
REVIEW ARTICLE Failure of Bone Marrow Stimulation Techniques Rachel M. Frank, MD,* Eric J. Cotter, BS,* Islam Nassar, MBBCh, M.Ch (orth), MBA, MHA,w and Brian Cole, MD, MBA* to prevent further joint deterioration. The limitations in Abstract: Marrow stimulation techniques, including microfracture, intrinsic articular cartilage physiology and regeneration has are among the most commonly performed cartilage restoration led to an influx of research into surgical cartilage restora- procedures for symptomatic chondral defects of the knee. For the tion techniques. vast majority of patients, marrow stimulation results in reduced There are numerous surgical options available for the pain and improved function, providing overall satisfactory out- comes. In some cases, however, marrow stimulation fails, resulting treatment of focal chondral defects, which can be broadly in symptom recurrence and often, the need for repeat surgery. This categorized into 4 groups: palliative options, including review will describe the indications and outcomes of microfracture arthroscopic debridement and lavage; reparative options, as a primary surgical treatment for focal chondral defects of the including microfracture and other bone marrow stimulation knee, identify patient and procedure-specific factors associated with techniques; restorative options including osteochondral poor clinical outcomes, and will discuss treatment options and their autograft transfer (OATS) and autologous chondrocyte respective outcomes for patients with a failed prior microfracture implantation (ACI) procedures; and reconstructive options surgery. including osteochondral allograft transplantation.9 Regard- Key Words: cartilage restoration, microfracture failure, marrow less of the specific technique chosen, the goals of surgical stimulation failure, autologous chondrocyte implantation, osteo- treatment are similar, including the ability to improve joint chondral allograft transplantation function, relieve pain, and allow patients to return to activity or in the case of athletes, return to sport. -

Exome Sequencing Reveals a Phenotype Modifying Variant in ZNF528 in Primary Osteoporosis with a COL1A2 Deletion
ORIGINAL ARTICLE Exome Sequencing Reveals a Phenotype Modifying Variant in ZNF528 in Primary Osteoporosis With a COL1A2 Deletion Sini Skarp,1,2,3† Ji-Han Xia,2,4† Qin Zhang,2,4 Marika Löija,2,3 Alice Costantini,5 Lloyd W Ruddock,2 Outi Mäkitie,5,6,7,8,9 Gong-Hong Wei,2,4,10† and Minna Männikkö1,3† 1Infrastructure for Population Studies, Northern Finland Birth Cohorts, Faculty of Medicine, University of Oulu, Oulu, Finland 2Faculty of Biochemistry and Molecular Medicine, University of Oulu, Oulu, Finland 3Center for Life Course Health Research, Faculty of Medicine, University of Oulu, Oulu, Finland 4Biocenter Oulu, University of Oulu, Oulu, Finland 5Department of Molecular Medicine and Surgery and Center for Molecular Medicine, Karolinska Institutet/Stockholm, Stockholm, Sweden 6Department of Clinical Genetics, Karolinska University Hospital, Stockholm, Sweden 7Children’s Hospital and Pediatric Research Center, University of Helsinki and Helsinki University Hospital, Helsinki, Finland 8Folkhälsan Research Center, Genetics Research Program, Helsinki, Finland 9Research Program for Clinical and Molecular Metabolism, Faculty of Medicine, University of Helsinki, Helsinki, Finland 10Department of Biochemistry and Molecular Biology, School of Basic Medical Sciences and Zhongshan Hospital, Fudan University, Shanghai, China ABSTRACT We studied a family with severe primary osteoporosis carrying a heterozygous p.Arg8Phefs*14 deletion in COL1A2, leading to hap- loinsufficiency. Three affected individuals carried the mutation and presented nearly identical spinal fractures but lacked other typical features of either osteogenesis imperfecta or Ehlers-Danlos syndrome. Although mutations leading to haploinsufficiency in COL1A2 are rare, mutations in COL1A1 that lead to less protein typically result in a milder phenotype. -

Autologous Matrix-Induced Chondrogenesis (AMIC) E
REVISTA ESPAÑOLA DE ARTROSCOPIA Y CIRUGÍA ARTICULAR Asociación Española de Artroscopia Vol. 28. Issue 1. No. 71. January 2021 ISSN: 2792-2154 (printed) 2792-2162 (online) Monograph: Treatment of chondral ulcers Autologous matrix-induced chondrogenesis (AMIC) E. Sánchez Alepuz1,2,3, J. Part Soriano1,3, I. Peregrin Nevado2,3, J. Zurriaga Carda2,3, J. M. Gómez Alessandri1,3, J. Vicente Díaz2,3, R. Calero Ferrandiz1,3 1 Department of Orthopedic Surgery and Traumatology. Unión de Mutuas. Valencia (Spain) 2 Department of Orthopedic Surgery and Traumatology. IMED Valencia. Burjassot, Valencia (Spain) 3 Grupo de Estudio e Investigación del Cartílago Articular de Valencia (GEICAV) (Spain) Correspondence: Received 8 July 2019 Dr. Joan Part Soriano Accepted 16 October 2020 E-mail: [email protected] Available online: January 2021 ABSTRACT RESUMEN Objective: To analyze the evolution and current status of the au- Condrogénesis inducida por matrices (AMIC) tologous matrix-induced chondrogenesis (AMIC) technique and know its underlying biological principles, as well as the results Objetivo: examinar la evolución y la situación actual de la técni- of its use in treating chondral lesions. ca AMIC y conocer los principios biológicos sobre los que se sus- Method: A literature review is made of the basic science re- tenta, así como los resultados de su utilización en el tratamiento ferred to cartilage injuries, the surgical technique, and clinical de las lesiones condrales. outcomes versus other chondral repair and regeneration tech- Método: se realiza una revisión de la bibliografía sobre la ciencia niques. básica relativa a las lesiones de cartílago, la técnica quirúrgica y Results: According to the published studies, AMIC improves pain los resultados clínicos respecto a otras técnicas de reparación y and the clinical and functional scores, affording better outcomes regeneración condral. -
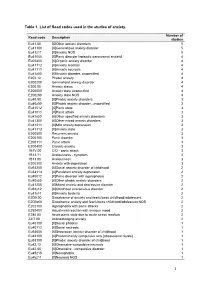
1 Table 1. List of Read Codes Used in the Studies of Anxiety
Table 1. List of Read codes used in the studies of anxiety. Number of Read code Description studies Eu41.00 [X]Other anxiety disorders 5 Eu41100 [X]Generalized anxiety disorder 5 Eu41z11 [X]Anxiety NOS 5 Eu41000 [X]Panic disorder [episodic paroxysmal anxiety] 4 Eu05400 [X]Organic anxiety disorder 4 Eu41112 [X]Anxiety reaction 4 Eu41111 [X]Anxiety neurosis 4 Eu41z00 [X]Anxiety disorder, unspecified 4 E202.12 Phobic anxiety 4 E200200 Generalised anxiety disorder 4 E200.00 Anxiety states 4 E200000 Anxiety state unspecified 4 E200z00 Anxiety state NOS 4 Eu40.00 [X]Phobic anxiety disorders 3 Eu40z00 [X]Phobic anxiety disorder, unspecified 3 Eu41012 [X]Panic state 3 Eu41011 [X]Panic attack 3 Eu41y00 [X]Other specified anxiety disorders 3 Eu41300 [X]Other mixed anxiety disorders 3 Eu41211 [X]Mild anxiety depression 3 Eu41113 [X]Anxiety state 3 E200500 Recurrent anxiety 3 E200100 Panic disorder 3 E200111 Panic attack 3 E200400 Chronic anxiety 3 1B1V.00 C/O - panic attack 3 1B13.11 Anxiousness - symptom 3 1B13.00 Anxiousness 3 E200300 Anxiety with depression 3 Eu93200 [X]Social anxiety disorder of childhood 2 Eu34114 [X]Persistant anxiety depression 2 Eu40012 [X]Panic disorder with agoraphobia 2 Eu40y00 [X]Other phobic anxiety disorders 2 Eu41200 [X]Mixed anxiety and depressive disorder 2 Eu93y12 [X]Childhood overanxious disorder 2 Eu41y11 [X]Anxiety hysteria 2 E2D0.00 Disturbance of anxiety and fearfulness childhood/adolescent 2 E2D0z00 Disturbance anxiety and fearfulness childhood/adolescent NOS 2 E202100 Agoraphobia with panic attacks 2 E292400