Colchester Group Practice
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
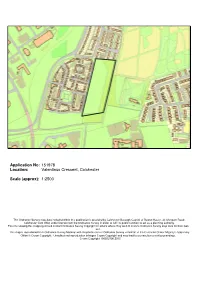
Application No: 151978 Location: Valentinus Crescent, Colchester
Application No: 151978 Location: Valentinus Crescent, Colchester Scale (approx): 1:2500 The Ordnance Survey map data included within this publication is provided by Colchester Borough Council of Rowan House, 33 Sheepen Roadl, Colchester CO3 3WG under licence from the Ordnance Survey in order to fulfil its public function to act as a planning authority. Persons viewing this mapping should contact Ordnance Survey copyright for advice where they wish to licence Ordnance Survey map data for their own use. This map is reproduced from Ordnance Survey Material with the permission of Ordnance Survey on behalf of the Controller Of Her Majesty’s Stationery Office Crown Copyright. Unauthorised reproduction infringes Crown Copyright and may lead to prosecution or civil proceedings. Crown Copyright 100023706 2015 7.3 Case Officer: Alistair Day Due Date: 03/12/2015 MAJOR Site: Valentinus Crescent, Colchester Application No: 151978 Date Received : 3 September 2015 Agent: Mr Stephen Collis Applicant: Colchester Borough Council Development: Variation of condition 2 of planning permission 142439. Ward: Berechurch Summary of Recommendation: Conditional Approval 1.0 Reason for Referral to the Planning Committee 1.1 This application is referred to the Planning Committee because the applicant is Colchester Borough Council. 2.0 Synopsis 2.1 The key issues explored below are whether the variation of condition 2 of planning approval 142439 (amendment of the car park layout) will have a significant impact on the character and appearance of the area and/or amenity of nearby residents. 3.0 Site Description and Context 3.1 The application site is a rectangular shaped piece of land that extends to some 2.49 hectares. -

2018 Eastern Command (History & Personnel)
2018 www.BritishMilitaryHistory.co.uk Author: Robert PALMER A CONCISE HISTORY OF: EASTERN COMMAND (HISTORY & PERSONNEL) A concise history of Middle East Command, a higher level formation of the British Army in existence from 1939 until 1967. In addition, known details of the key appointments held between 1939 and 1950 are included. Copyright ©www.BritishMilitaryHistory.co.uk (2018) 9 October 2018 [EASTERN COMMAND HISTORY & PERSONNEL] A Concise History of Eastern Command (History & Personnel) This edition dated: 9 October 2018 ISBN All rights reserved. No part of the publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means including; electronic, electrostatic, magnetic tape, mechanical, photocopying, scanning without prior permission in writing from the publishers. Author: Robert PALMER, M.A. (copyright held by author) Published privately by: The Author – Publishing as: www.BritishMilitaryHistory.co.uk ©www.BritishMilitaryHistory.co.uk Page 1 9 October 2018 [EASTERN COMMAND HISTORY & PERSONNEL] Eastern Command Eastern Command was reorganised in 1920 following the Great War. Its Headquarters were based in Queen’s Gardens, Bayswater, London; but it moved to Horse Guards, London SW1 by 1930. As one of the five Home Commands within the United Kingdom, it was a Lieutenant General (or General’s) command, who was the General Officer Commanding-in-Chief. This meant he had complete jurisdiction of all land forces within his command. Eastern Command in 1939 comprised the counties of Cambridgeshire, Norfolk, Suffolk, Essex (except Purfleet and Rainham Rifle Range, and the Guards Barracks at Warley – when occupied by the Foot Guards – which all came under the London District), Hertfordshire, Bedfordshire, Middlesex, Kent, Sussex and Surrey (less the area within Aldershot Command). -

TRUMPET and BUGLE SOUNDS for the Army
/"M^ 3o3- MILITARY BOOKS ttMtsjjrtr bg lllp|l» Sttiboriig. LONDON: PRINTED UNDER THE AUTHORITY OF HIS MAJESTY'S STATIONERY OFFICE By HARRISON and SONS, 45-47, St. Martin's Lane, W.C., Printers in Ordinary to His Majesty. To be purchased, either directly or through any Bookseller, from WYMAN and SONS, Ltd., 29, Breams Buildings, Fetter Lane, B.C., and 54, St. Mary Street, Cardiff; or H.M. STATIONERY OFFICE (Scottish Branch), 23, Forth Street, Edinburgh ; or . E. PONSONBY, Ltd., 116, Grafton Street, Dublin ; or from the Agencies in the British Colonies and Dependencies, the United States of America, the Continent of Europe and Abroad of T. FISHER UNWIN, London, W.C. (The prices in brackets are those at which the hooks are obtainable, post free, by Officers, Non-Commissioned Officers and Men, in the manner prescribed by the Regulations.) ABYSSINIA. Expedition to. 2 vols, and maps. 1870. Half Mor., £5 5* Cloth, £4 4s. AFRICA. Continent of. Geology of. Notes on. 1906. 3s. (2s. id.) AMHARIO LANGUAGE. Short Manual of the. With Vocabulary. 1909. 5». (3s. 6£) ANIMAL MANAGEMENT. 1908. Is. Gd. (1*. 4d) ARABIC GRAMMAR. Two parls. 1887. (Sold to Officers only.') 10*. (10s. 6d) ARMOURERS. Instructions for, in the care, repair, browning, &c, of Small Arms, Machine Guns, " Parapet" Carriages, and for the care of Bicycles. 1912. Is. Gd. (U. id.) Ditto. Amendments. Aug. 1912. Id. (Id.) ARMY ACCOUNTS. (Reprinted from The Akmy Review, January, 1914.) 3d. (3d.) ARMY LIST. The Quarterly. Each 15*. (10s. Gd.) ARMY LIST. Monthly. Each Is. Gd. (Is. id.) ARMY CIRCULARS AND ARMY ORDERS issued before Dec. -

Essex County Council (The Commons Registration Authority) Index of Register for Deposits Made Under S31(6) Highways Act 1980
Essex County Council (The Commons Registration Authority) Index of Register for Deposits made under s31(6) Highways Act 1980 and s15A(1) Commons Act 2006 For all enquiries about the contents of the Register please contact the: Public Rights of Way and Highway Records Manager email address: [email protected] Telephone No. 0345 603 7631 Highway Highway Commons Declaration Link to Unique Ref OS GRID Statement Statement Deeds Reg No. DISTRICT PARISH LAND DESCRIPTION POST CODES DEPOSITOR/LANDOWNER DEPOSIT DATE Expiry Date SUBMITTED REMARKS No. REFERENCES Deposit Date Deposit Date DEPOSIT (PART B) (PART D) (PART C) >Land to the west side of Canfield Road, Takeley, Bishops Christopher James Harold Philpot of Stortford TL566209, C/PW To be CM22 6QA, CM22 Boyton Hall Farmhouse, Boyton CA16 Form & 1252 Uttlesford Takeley >Land on the west side of Canfield Road, Takeley, Bishops TL564205, 11/11/2020 11/11/2020 allocated. 6TG, CM22 6ST Cross, Chelmsford, Essex, CM1 4LN Plan Stortford TL567205 on behalf of Takeley Farming LLP >Land on east side of Station Road, Takeley, Bishops Stortford >Land at Newland Fann, Roxwell, Chelmsford >Boyton Hall Fa1m, Roxwell, CM1 4LN >Mashbury Church, Mashbury TL647127, >Part ofChignal Hall and Brittons Farm, Chignal St James, TL642122, Chelmsford TL640115, >Part of Boyton Hall Faim and Newland Hall Fann, Roxwell TL638110, >Leys House, Boyton Cross, Roxwell, Chelmsford, CM I 4LP TL633100, Christopher James Harold Philpot of >4 Hill Farm Cottages, Bishops Stortford Road, Roxwell, CMI 4LJ TL626098, Roxwell, Boyton Hall Farmhouse, Boyton C/PW To be >10 to 12 (inclusive) Boyton Hall Lane, Roxwell, CM1 4LW TL647107, CM1 4LN, CM1 4LP, CA16 Form & 1251 Chelmsford Mashbury, Cross, Chelmsford, Essex, CM14 11/11/2020 11/11/2020 allocated. -

List of British Army Garrisons and Installations in the UK and Abroad
'''''''''''''''' '''''''''' ''''''''''''''''''''''''' Army Personnel Centre '''''''''' ''''''''''' ''''''''' Kentigern House 65 Brown Street GLASGOW G2 8EX Ref: FOI2018/03121 E-mail: [email protected] ''''''' ''''''''''''''''''''''' ''''' '''''' ''''''''''''''' '''''' 20 March 2018 '''''''''''''''''''''''''''''''''''''''''''''''''''''''''' Dear ''''''' '''''' Thank you for your email of 28 February requesting the following information: Could you provide the list of British Army Garrisons/Installations in the UK and abroad besides London District which have Garrison Sergeant Majors? I am treating your correspondence as a request for information under the Freedom of Information Act 2000 (FOIA). The information you require is shown at Annex A. If you have any queries regarding the content of this letter, please contact this office in the first instance. If you wish to complain about the handling of your request, or the content of this response, you can request an independent internal review by contacting the Information Rights Compliance team, Ground Floor, MOD Main Building, Whitehall, SW1A 2HB (e-mail CIO- [email protected]). Please note that any request for an internal review should be made within 40 working days of the date of this response. If you remain dissatisfied following an internal review, you may raise your complaint directly to the Information Commissioner under the provisions of Section 50 of the Freedom of Information Act. Please note that the Information Commissioner will not normally investigate your case until the MOD internal review process has been completed. The Information Commissioner can be contacted at: Information Commissioner’s Office, Wycliffe House, Water Lane, Wilmslow, Cheshire, SK9 5AF. Further details of the role and powers of the Information Commissioner can be found on the Commissioner's website at https://ico.org.uk/. -

World War II
‘We Will Remember Them ’ RONALD JACK ARGENT RAFVR 1389316 Flight Sergeant 102 (Ceylon) Squadron Royal Air Force Ronald Argent was born about 1923, the son of John and Margaret Annie Argent. Before the war he worked at Pettit's Dairy in Little Coggeshall. He joined the Royal Air Force Volunteer Reserve and at the time of his death was flying Halifaxes with 102 Squadron RAF out of Pocklington in Yorkshire . 102 Squadron was a heavy bomber squadron and part of No. 4 Group (Bomber Command). It was re-equipped with the Handley Page Halifax in 1942 and adopted by the island of Ceylon in the same year. The Squadron took part in each of the three historic 1,000-bomber raids in May/June 1942 and, later, in the battles of the Ruhr, Hamburg, and Berlin. On 4th December 1943, Halifax JD303 DY-S was airborne at 00:17 hours from RAF Pocklington as part of a bombing raid on Leipzig. The aircraft crashed at Luderitz, 9 kilometres north-west of Tangerhutte (cause not established). Five members of the crew, including Ronald Argent, were killed and two were taken prisoner by the Germans. Those killed were initially buried on 5th December 1943 at Luderitz. Their graves are now located in the Berlin 1939—1945 Cemetery. The site of Berlin 1939-45 War Cemetery was selected by the British Occupation Authorities and Commonwealth War Grave Commission officials jointly in 1945, soon after hostilities ceased. Graves were brought to the cemetery from the Berlin area and from eastern Germany. The great majority of those buried here, approximately 80 per cent of the total, were airmen who were lost in the air raids over Berlin and the towns in eastern Germany. -

Registration Document Fiscal 2014 Registration
RegistrationRegistration Document Fiscal 2014 including the Annual Financial Report 1 6 PRESENTATION OF THE GROUP 3 SHAREHOLDERS – 1.1 Messages from the Chairman of the Board FINANCIAL COMMUNICATION 267 and the Chief Executive Offi cer 4 6.1 Financial Communication 268 1.2 Our History 24 6.3 Sodexo Share Performance 272 1.3 Our Group and Our Quality of Life Services 26 6.4 Capital 276 CONTENTS 2 7 ECONOMIC, SOCIAL AND CORPORATE GOVERNANCE 279 ENVIRONMENTAL RESPONSIBILITY 87 7.1 Chairman’s Report on the Operating 2.1 The Better Tomorrow Plan 88 Procedures of the Board of Directors and 2.2 We Are 89 on Internal Control and Risk Management Procedures 280 2.3 We Do 90 7.2 Other information concerning the Corporate 2.4 We Engage 108 Offi cers and Senior Management of the 2.5 Rankings and awards 111 Company 308 2.6 Indicators, reporting methodology and 7.3 Compensation 310 Statutory Auditor’s Report 114 7.4 Audit fees 332 2.7 Data related to Sodexo’s activities in France 125 8 3 ANNUAL ORDINARY SHAREHOLDERS’ CONSOLIDATED INFORMATION 131 MEETING, JANUARY 19, 2015 335 3.1 Fiscal 2014 Activity Report 132 8.1 Board Report 3.3 Notes to the consolidated fi nancial statements 158 Presentation of Resolutions submitted to the Ordinary Shareholders’ Meeting, January 19, 3.4 Statutory Auditors’ Report on 2015 336 the consolidated fi nancial statements 216 8.2 Resolutions submitted to the Ordinary 3.5 Supplemental information 218 Shareholders’ Meeting of January 19, 2015 341 4 INFORMATION ON THE ISSUER 227 9 OTHER INFORMATION 347 4.1 Sodexo SA Individual -

Ice Manual, 914
[CV ^^^fl^^lfi^^Q^l^i ICE MANUAL, 914. BATTALION. NARY FORCE.) NOTE, Field Service Manuals are not the authority for the supply of war outfit of units, The details, laid down in latest Mobilization Store Tables, Equipment Regulations, Clothing Regulations, &c., will be followed. _ IORITY OF MAJKSTVS STA.TIONKKY h-eetlv or thrr.uKh any Bookseller, from BKKAMS BoiLJ>iios, PaTTEB LANK E.G., and STrtRr.T. OAKOJ!;-", or or ID BRANCH), 23, FORTH STREET, EDINBURGH ; LIU, GR/vrro.v STBKET, Dcm.rv ; 1445 in rho British Colonies and D^peu'lenc; s, i G7G7 . .< i tlio 'oMtinent of Europe and Abroad of 1914 c. 1 HBP ROBA Price Threepence^ MILITARY BOOKS ^utb0ritjr. LONDON: PRINTED UNDER THE AUTHORITY OF HIS MAJESTY'S STATIONERY OFFICE By HARRISON AND SONS. 45-47, ST. MARTIN'S LANK, W.C., PRINTERS IN ORDINARY TO His MA.I To be purchased, either directly or through any Bookseller, from WYXIAN AND SONS, LTD., 20, BHF.AMS BUILDINGS, FETTKR LAM , K.C., and 54, ST. MARY STRKET, CARDIFF; or UM. STATIONERY OFFICE (SCOTTISH BRANCH). :>:?. FORTH STRKET, EDINBURGH ; or K. PONSONBY, LTD., 116, GRAFTON STREET, Drm.ix -, or from the Agencies in the British Colonies ;unl IV; the United States of America flu- Continent of Kurope uml Abroad of T. FISHER L'XWIN, LONDON, W.C. (The prices in brackets are those at which the books are obtainable, post free, by Officers, Non-Commissioned Officers and Men, in the manner prescribed by the Regulations.) ABYSSINIA. Expedition to. 2 vols. and maps. 1870. Half Mor., 6 5*. -

Historic Recording Building at the Le Cateau And
1858 HISTORIC RECORDING BUILDING AT THE LE CATEAU AND CAVALRY BARRACKS COLCHESTER GARRISON ESSEX Field Archaeology Unit April 2008 Cover depicts gun practice on Abbey Field with the Cavalry & Royal Artillery Barracks in the background (http:/www.camulos.com/postcardshtm) HISTORIC BUILDING RECORDING AT THE LE CATEAU AND CAVALRY BARRACKS COLCHESTER GARRISON ESSEX Prepared By: Andrew Letch Signature: Position: Project Officer Date: 14th April 2008 Approved By: Mark Atkinson Signature: Position: Unit Manager Date: 14th April 2008 Document Ref. 1858rep Report Issue Date 14th April 2008 Circulation Lexden Restoration & Development Martin Winter (Colchester Museums Service) Essex Historic Environment Record As part of our desire to provide a quality service, we would welcome any comments you may have on the content or the presentation of this report. Please contact the Unit Manager, at the Field Archaeology Unit, Fairfield Court, Fairfield Road, Braintree, Essex CM7 3YQ Tel: 01376 331470 Fax: 01376 331428 © Field Archaeology Unit, Essex County Council, c/o County Hall, Chelmsford Essex CM1 1LF CONTENTS 1.0 INTRODUCTION 2.0 BACKGROUND 2.1 Location and description 2.2 Planning background 2.3 Historical background 3.0 AIMS AND OBJECTIVES 4.0 METHODS 5.0 BUILDING DESCRIPTIONS 5.1 Layout and general description 5.2 Stable block A 5.3 Canteen & sergeants mess 5.4 Adult school 5.5 Riding school 6.0 DISCUSSION 7.0 CONCLUSION ACKNOWLEDGEMENTS BIBLIOGRAPHY Appendices Appendix 1: Archive index Appendix 2: EHER summary sheet Figures Figure 1. Location and block plan Figure 2. General plan of Royal Artillery Barracks, 1875 Figure 3. Historic floor plans of stable block A, 1875 Figure 4. -

Colchester Historic Characterisation Report 2009
Front Cover: Arial view of Colchester Castle and Castle Park. ii Content FIGURES................................................................................................................................................VI ABBREVIATIONS..................................................................................................................................IX ACKNOWLEDGEMENTS.......................................................................................................................X COLCHESTER BOROUGH HISTORIC ENVIRONMENT CHARACTERISATION PROJECT ........... 11 1 INTRODUCTION .......................................................................................................................... 11 1.1 PURPOSE OF THE PROJECT ..................................................................................................... 12 2 THE HISTORIC ENVIRONMENT OF COLCHESTER BOROUGH............................................. 14 2.1 PALAEOLITHIC ........................................................................................................................ 14 2.2 MESOLITHIC ........................................................................................................................... 15 2.3 NEOLITHIC ............................................................................................................................. 15 BRONZE AGE....................................................................................................................................... 16 2.4 IRON AGE.............................................................................................................................. -
Middlewick Ranges Archaeology Desk-Based Assessment
Middlewick Ranges Colchester Essex Archaeological Desk-Based Assessment Document Ref.: 228290.01 October 2020 © Wessex Archaeology Ltd 2020, all rights reserved 69 College Road Maidstone Kent ME15 6SX www.wessexarch.co.uk Wessex Archaeology Ltd is a company limited by guarantee registered in England, company number 1712772. It is also a Charity registered in England and Wales number 287786, and in Scotland, Scottish Charity number SC042630. Our registered office is at Portway House, Old Sarum Park, Salisbury, Wiltshire, SP4 6EB. Disclaimer The material contained in this report was designed as an integral part of a report to an individual client and was prepared solely for the benefit of that client. The material contained in this report does not necessarily stand on its own and is not intended to nor should it be relied upon by any third party. To the fullest extent permitted by law Wessex Archaeology will not be liable by reason of breach of contract negligence or otherwise for any loss or damage (whether direct indirect or consequential) occasioned to any person acting or omitting to act or refraining from acting in reliance upon the material contained in this report arising from or connected with any error or omission in the material contained in the report. Loss or damage as referred to above shall be deemed to include, but is not limited to, any loss of profits or anticipated profits damage to reputation or goodwill loss of business or anticipated business damages costs expenses incurred or payable to any third party (in all cases -

COLCHESTER BOROUGH COUNCIL PLANNING COMMITTEE 1 November 2012 at 6:00Pm
COLCHESTER BOROUGH COUNCIL PLANNING COMMITTEE 1 November 2012 at 6:00pm SUPPLEMENTARY AGENDA Part A (open to the public including the media) Pages 9. Construction of a new 300 place primary school with external hard 23 44 and soft play areas, canopy and 20 space car park (New Town) See report by the Head of Environmental and Protective Services. The Chairman has agreed pursuant to the provisions of Section 100B(4)(b) of the Local Government Act 1972 to consider this item at the meeting as a matter of urgency because the deadline date for a response to consultation by Essex County Council is 26 October 2012. 10. Amendment Sheet 45 53 See Amendment Sheet attached. Application No: 121762 Location: Garrison Area E, Circular Road East, Colchester Scale (approx): 1:1250 The Ordnance Survey map data included within this publication is provided by Colchester Borough Council of PO Box 884, Town Hall, Colchester CO1 1FR under licence from the Ordnance Survey in order to fulfil its public function to act as a planning authority. Persons viewing this mapping should contact Ordnance Survey copyright for advice where they wish to licence Ordnance Survey map data for their own use. This map is reproduced from Ordnance Survey Material with the permission of Ordnance Survey on behalf of the Controller Of Her Majesty’s Stationery Office Crown Copyright. Unauthorised reproduction infringes Crown Copyright and may lead to prosecution or civil proceedings. Crown Copyright 100023706 2012 1 Item Planning Committee 9 1 November 2012 Report of Head of Environmental & Protective Author Alistair Day Services « 01206 282479 Title Construction of a new 300 place primary school with external hard and soft play areas, canopy and 20 space car park.