Running Title: Disturbance of Consciousness in Acute Pancreatitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Physician's Newsletter
PUBLISHED· BY THE N. Y. C. MEDICAL SOCIETY PHYSICIAN'S ON ALCOHOLISM, Inc. 167 East 80 St. New York 21, N.Y. A MARCH 1966 VOL. I, NO.2 ©Copyright 1966 The N.Y.C. Medical. NEWSLETTER Society on Alcoholism, Inc. I -HISTORIC RULING I 'TOTAL ABSTINENCE' TERMED A U.S. Court of Appeals tribunal in OBJECTIVE OF TREATMENT Richmond, Va., has rulee unanimously Alcoholic patients whose treatment led to total abstinence had the best chance that it is "cruel and unusual punish of marked improvement of social adaptation, according to Dr. D. L. Davies, director ment" to arrest and treat a chronic alco of psychiatry at Maudsley Hospital, London, England, a major teaching center. He holic as a criminal; he might, however, spoke at a seminar at Norwalk Hospital, Norwalk, Conn., about an. article .of. :I.Jis · be held for medical treatment. which had been widely thought to endorse treatment directed at·a return to so6Ial The case involved an individual who drinking. had been convicted of public intoxica Misunderstandings had arisen as a result of his report, "Normal Drinking tion more than 200 times and who esti in Reversed Alcoholics" published last mates that he has spent more than two year in the Quarterly Journal of Alcohol thirds of his life in jail. Studies. The article reports the elabo CENTRAL ISLIP OPENS Crux of the decision, which set aside rate follow-up studies of patients treated ALCOHOL FACILITY a 2-year sentence, was the court's state for alcoholism in Maudsley Hospital, in Dedication of the Charles K. -

Blind Drunk: Alcoholic Pancreatitis and Loss Ofvision James R
CLINICAL REPORTS 151 Postgrad Med J: first published as 10.1136/pgmj.69.808.151 on 1 February 1993. Downloaded from Postgrad Med J (1993) 69, 151 - 152 A) The Fellowship of Postgraduate Medicine, 1993 Blind drunk: alcoholic pancreatitis and loss ofvision James R. Steel, John R. Cockcroft and James M. Ritter Department ofClinical Pharmacology, Guy's Hospital Medical School, London SE] 9RT, UK Summary: Acute loss of vision and alcoholic intoxication suggests the possibility of methanol poisoning. In this report we describe an alcoholic patient who complained of blindness after recovering from alcoholic pancreatitis and delirium tremens. Visual acuity was severely impaired and fundoscopy revealed florid bilateral cotton wool spots and a cherry red spot at the right macula. Such appearances have previously been reported in cases of post-traumatic visual loss, and may share a common aetiology of fat embolization. The association between alcoholic pancreatitis and visual loss is rare, and fundal examination should be performed on all patients with pancreatitis, especially those who complain ofvisual disturbance. Introduction Previous case reports have confirmed an associa- agitated state. Blood ethanol was 63.8 mg/l00 ml, tion between severe alcoholic pancreatitis and 'y-glutamyl transpeptidase was raised at 206 U/l visual loss.'"2 These changes are remarkably similar (normal range 11- 54), aspartate transaminase to those seen in post-traumatic retinopathy. raised at 46 U/l (normal range < 23) and amylase Protected by copyright. Although blindness associated with alcohol abuse raised at 809 U/l (normal range < 220). There was suggests the possibility of methanol ingestion, it is a neutrophil leucocytosis with total white cell count important to consider the possibility of a retino- of 17.1 x 109/l and the mean corpuscular volume pathy due to alcoholic pancreatitis and fundal was 102 fl (normal range 76-96). -

Delirium Tremens
DELIRIUM TREMENS Alcohol and Narcotic Withdrawals Delirium Tremens (commonly referred to as "The Horrors", "Jazz Hands", or "The Shakes") is a psychological and physiological reaction to the sudden disruption of habitual/prolonged daily alcohol or narcotic consumption. Delirium Tremens (aka. "DT's") is also referred to as "Alcoholic Psychosis". BACKGROUND Delirium Tremens is the most severe form of alcohol withdrawal, which may result in hallucinations, seizures, and cardiovascular collapse. According to http://emedicine.medscape.com, the syndrome was first described by Thomas Sutton in 1813, but the link to alcohol abstinence wasn't made until the 1950's. Historically, older white males had a higher risk of developing severe alcohol withdrawal. Throughout the years, alcohol and drug withdrawal have been seen frequently in the corrections setting. This is due to many offenders being addicted to alcohol or drugs, and a sudden interruption of alcohol or drug use occurs when offenders are taken into custody. Because of the volatile situation of an individual withdrawing from alcohol or drugs, correctional health care providers and custodial staff should be properly trained to recognize the symptoms and ·.·. 1--r-1OOr::'.\t,1-\/cc.;•:c•;·•;L;;;;;.;;;;c;;o•;;;;;c=c•'cefCf"'''-••;•~•·cc-c_••--•'CCCc;_;'-'.; t" . ___ ,··.; .. ; res P0 nd Pro 1 ALCOHOL-RELATED DEATHS: THENAND NOW According to the Center for Disease Control (CDC), in the United States, excessive alcohol consumption was the third leading preventable cause of death in 2001. It was estimated that in 2001, approximately 75,766 deaths were attributed to the harmful effects of excessive alcohol use. In 2008, a more recent study was done, that determined that in 2001-2005, approximately 79,000 occurred annually that were attributed to excessive alcohol use. -

Assessment and Treatment of Alcohol Dependence Suggested Citation: Quigley, A., Connolly, C., Palmer, B., & Helfgott, S
A brief guide to the Assessment and Treatment of Alcohol Dependence Suggested citation: Quigley, A., Connolly, C., Palmer, B., & Helfgott, S. (2015) A brief guide to the assessment and treatment of alcohol dependence (2nd ed.). Perth, Western Australia: Drug and Alcohol Office. ISBN: 978-1-876684-63-1 © Western Australian Drug and Alcohol Authority 2015 Note – The Drug and Alcohol Office is the business name of the Western Australian Alcohol and Drug Authority, which is an independent statutory authority established in November 1974. Its functions are set out in the Alcohol and Drug Authority Act 1974. This booklet is produced by Next Step Drug and Alcohol Services and Workforce Development Branch, Drug and Alcohol Office. It may be reproduced in whole or in part for study or training purposes subject to an inclusion of an acknowledgement of the source and no commercial usage or sale. Reproduction for purposes other than those above requires the written permission of: Drug and Alcohol Office, PO Box 126, Mount Lawley WA 6929 Website: www.dao.health.wa.gov.au Next Step DRUG AND ALCOHOL SERVICES ii A brief guide to the Assessment and Treatment of Alcohol Dependence Contents Introduction ................................................................................................................................................................2 Assessment .................................................................................................................................................................2 History .........................................................................................................................................................................2 -

Alcohol, Murder and Medical Jurisprudence In
© 2014 Michele Rotunda ALL RIGHTS RESERVED “DRUNKENNESS IS NO EXCUSE FOR CRIME” – ALCOHOL, MURDER, AND MEDICAL JURISPRUDENCE IN NINETEENTH- CENTURY AMERICA by MICHELE ROTUNDA A Dissertation submitted to the Graduate School – New Brunswick Rutgers, The State University of New Jersey in partial fulfillment of the requirements for the degree of Doctor of Philosophy Graduate Program in History Written under the direction of Susan R. Schrepfer And approved by ___________________________________________ ___________________________________________ ___________________________________________ ___________________________________________ New Brunswick, New Jersey May 2014 ABSTRACT OF THE DISSERTATION “DRUNKENNESS IS NO EXCUSE FOR CRIME” – ALCOHOL, MURDER, AND MEDICAL JURISPRUDENCE IN NINETEENTH-CENTURY AMERICA BY MICHELE ROTUNDA Dissertation Director: Susan R. Schrepfer Using a variety of court cases as evidence, this study focuses on several competing, and often unresolved, models of responsibility for crimes related to intoxication that emerged in nineteenth century America. Drunkenness truly was “no excuse” for crime in the early years of the nineteenth century; however, changes in the fields of medicine, the law, and society created the circumstances under which such a defense became more viable, and certainly more prevalent, if only intermittently successful, by mid-century. American courts began, in the 1820s, to accord an expanded exculpatory value to intoxication due to several factors: 1. The medicalization of alcohol use from delirium tremens to dipsomania to inebriety created categories of mental illness from which to argue for limited or even absent responsibility under the law. 2. American law, beginning in 1794, allowed for a greater recognition of the issue of intent in crimes, in particular, creating statutory degrees of violent crimes that were dependent on establishing appropriate mens rea. -

Problem Drinking – Management in General Practice FOCUS
Current issues in alcohol Problem drinking Apo Demirkol Katherine Conigrave Management in general practice Paul Haber Problem drinking has similar characteristics to many of Background the chronic conditions routinely managed in the general Management of problem drinking presents the general practice setting. The management of chronic conditions practitioner with similar challenges and rewards to those associated with the management of other chronic can at times be challenging and time consuming. conditions. However, the majority of Australian general practitioners find dealing with chronic conditions more rewarding and Objective satisfactory if they have clear treatment goals.1 This article presents a framework for managing alcohol problems in general practice based on national guidelines Management of drinking problems presents the GP with similar for the treatment of alcohol problems. opportunities for challenging and rewarding practice.2,3 The Discussion approach described in this article is based on the Guidelines for General practitioners are well placed to undertake the treatment of alcohol problems published by the Australian the management of drinking problems following an Government Department of Health and Ageing (see Resources).4 assessment of the amount of alcohol taken and the risks An algorithm for the management of problem drinking is shown this poses for the individual and the people around them. in Figure 1. This assessment starts the process of engagement and reflection on drinking habits and will inform the appropriate The management of drinking problems starts with an assessment management approach. Brief interventions can result of the amount of alcohol taken and the risks this poses for both in reduction in drinking in nondependent drinkers. -

Drugs Used in the Treatment of the Alcoholic
22 September 1962 S.A. TYDSKRIF VIR GENEESKUNDE 791 For the treatment of the acute 'drying out' period, once The clo ed group offers a deeper identification and again simplicity of methods should be aimed at. My per participation than does the open one. The group becomes sonal opinion is that complete withdrawal of alcohol makes a miniature cosmos and, through it, hostilities and conflicts the handling of cases infinitely easier than 'tapering'. There may be acted out, behaviour patterns revealed and com is little evidence that tapering reduces the onset of delirium prehended, and interper onal relationships widened; and tremens and much to show that it confuses the picture through communication the barren sense of alienation can further and lengthens the time taken before the patient be broken down. Group therapy is not an ea y way out becomes mentally clear. The drug treatment of the acute of difficulties; no change can be completely painless and phase and aversion treatment once the acute phase is over, group sessions go through changes that can be painful, are discussed on page 788 of this issue of the Journal. humiliating and exasperating, but in the end the members develop graduaUy an awareness of the meaning of reality Psychotherapy and of the immensity of the problems of life - facts which Psychotherapeutic procedures in the treatment of alco they had never faced up to before. holism may be considered under several headings: in Alcoholism is a disorder of living, and no therapy, dividual therapy, group therapy, rehabilitative measures, whether it be individual or group therapy, acts as a and social strategies. -
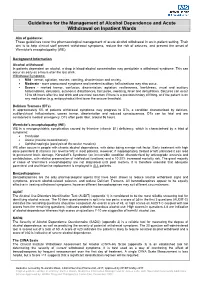
Guidelines for the Management of Alcohol Dependence and Acute Withdrawal on Inpatient Wards
Guidelines for the Management of Alcohol Dependence and Acute Withdrawal on Inpatient Wards Aim of guidance: These guidelines cover the pharmacological management of acute alcohol withdrawal in an in-patient setting. Their aim is to help clinical staff prevent withdrawal symptoms, reduce the risk of seizures, and prevent the onset of Wernicke’s encephalopathy (WE). Background Information Alcohol withdrawal In patients dependent on alcohol, a drop in blood-alcohol concentration may precipitate a withdrawal syndrome. This can occur as early as 6 hours after the last drink. Withdrawal Symptoms: Mild - tremor, agitation, nausea, vomiting, disorientation and anxiety. Moderate - more pronounced symptoms and transient auditory hallucinations may also occur. Severe - marked tremor, confusion, disorientation, agitation, restlessness, fearfulness, visual and auditory hallucinations, delusions, autonomic disturbances, fast pulse, sweating, fever and dehydration. Seizures can occur 12 to 48 hours after the last drink and are more common if there is a previous history of fitting, or if the patient is on any medication (e.g. antipsychotics) that lower the seizure threshold. Delirium Tremens (DTs) In approximately 5% of patients withdrawal symptoms may progress to DTs, a condition characterised by delirium, auditory/visual hallucinations, coarse tremor, disorientation and reduced consciousness. DTs can be fatal and are considered a medical emergency. DTs often peak later, around 96 hours. Wernicke’s encephalopathy (WE) WE is a neuropsychiatric complication caused by thiamine (vitamin B1) deficiency, which is characterised by a triad of symptoms: Confusion Ataxia (muscle incoordination) Ophthalmoplegia (paralysis of the ocular muscles) WE often occurs in people with chronic alcohol dependence, with detox being a major risk factor. -

Delirium Tremens PROPHYLAXIS Protocol Reference Text Use of This Protocol Requires MD Authorization
Delirium Tremens PROPHYLAXIS Protocol Reference Text Use of this protocol requires MD authorization. This protocol is intended for the PREVENTION of Alcohol Withdrawal Syndrome, and is NOT for the treatment of ACTIVE Alcohol Withdrawal Syndrome. ----------------------------------------------------------------------------------------------------------------------- DTs occur when early alcohol withdrawal symptoms are not promptly recognized and treated. Treatment with benzodiazepines should reduce or eliminate withdrawal symptoms. Patient Care Orders: > Implement Alcohol Withdrawal Syndrome (DT) Precautions > Riker Score Assessment q4h. > Riker score should also be documented prior to administration of any DT medication doses, Scheduled or PRN. > Riker Score Goal: 4 > DO NOT administer ANY doses if patient is sedated or Riker score is less than 4. Contact MD if Riker score is 2 or less. > NOTIFY MD: If patient begins to experience alcohol withdrawal delirium (Delirium Tremens) or continues to have symptoms despite prophylaxis regimen, NOTIFY MD immediately for initiation of Delirium Tremens TREATMENT Protocol and need to transfer to ICU for DT Treatment. > NOTIFY MRT: If MD does not respond within 10 minutes of the onset of Delirium Tremens (acute alcohol withdrawal) Call MRT. Medication Orders: Patient at LOW RISK for alcohol withdrawal delirium: n Lorazepam 1 mg PO q1h PRN for early withdrawal symptoms or Riker score greater than or equal to 5. (Treatment Duration: 10 days) *Per Protocol- may place order and administer IV Lorazepam if patient unable to take PO. Comment: DO NOT administer ANY doses if patient is sedated or Riker score is less than 4. Contact MD if Riker score is 2 or less. Patient at HIGH RISK for alcohol withdrawal delirium: n Scheduled Lorazepam PO for High Risk DT PROPHYLAXIS: Days 1 and 2: Lorazepam 2 mg PO q4h X 12 doses Days 3 and 4: Lorazepam 1 mg PO q6h X 8 doses *Per Protocol- may place order and administer IV Lorazepam if patient unable to take PO. -

Episode 87 Alcohol Withdrawal & Delrium Tremens
General Approach to the Management of Patients with Alcohol Withdrawal The ideal management of alcohol withdrawal involves 4 steps: Episode 87 – Alcohol Withdrawal & Delirium 1. Identify which patients actually have alcohol withdrawal and Tremens require treatment 2. Use a standardized, symptom guided approach to assess symptom severity and guide treatment With Drs. Mel Kahan, Sara Gray, Bjug Borgundvaag 3. Ensure that patients are fully treated prior to ED discharge 4. Provide a pathway to support patients who are trying to quit Prepared by Dr. Keerat Grewal, edited by Dr. Anton Helman, Oct 2016 Step 1: Identify which patients actually have alcohol withdrawal and require treatment. Alcohol withdrawal is everywhere. We see over half a million patients in US ED’s for alcohol withdrawal every year. Despite these huge Alcohol withdrawal is a clinical diagnosis and a diagnosis of exclusion. volumes of patients and the diagnosis of alcohol withdrawal seeming Patients with alcohol withdrawal often have a characteristic tremor, relatively straightforward, it’s actually missed more often than we’d which is an intention tremor: at rest there is no tremor, but when you like to admit, being confused with things like drug intoxication or sepsis ask the patient to extend their hands or arms you will see a fine motor - or it’s not even on our radar when an older patient presents with tremor (typically 7-12Hz) that is constant and does not fatigue with delirium. The differential diagnosis is enormous - and no blood test on time. Other symptoms associated with alcohol withdrawal include: the planet will help us diagnose alcohol withdrawal. -

Alcohol Withdrawal and Delirium in the Intensive Care Unit
Netherlands Journal of Critical Care Copyright © 2012, Nederlandse Vereniging voor Intensive Care. All Rights Reserved. Received April 2011; accepted February 2012 REVIEW Alcohol withdrawal and delirium in the intensive care unit M Paupers*, A Schiemann*, CD Spies * Marco Paupers and Alexander Schiemann contributed equally to this article Universitätsklinik für Anästhesiologie mit Schwerpunkt operative Intensivmedizin, Charité -Universitätsmedizin Berlin, Berlin, Germany Abstract - In intensive care patients, delirium triggered by alcohol withdrawal is underestimated despite the fact that it occurs in approximately 10% of all ICU patients. Alcohol withdrawal delirium is the most serious manifestation of alcohol withdrawal and it is associated with even more complications and poor outcome. Therefore, it should be prevented; if it does occur it should be treated as early as possible to avoid negative sequelae, in particular infections, cardiac complications and long-term cognitive dysfunction. In this article we summarize strategies to detect alcohol use disorders and alcohol withdrawal and those for treating alcoholic withdrawal and delirium tremens. Keywords - ICU, withdrawal, alcohol, delirium, alcohol withdrawal syndrome (AWS) Introduction This article gives an overview on how to reduce and treat this Besides nicotine, alcohol is the most abused drug worldwide [1- potentially life-threatening complication [18] in critically ill patients 4]. About one-fifth of the patients seen in clinical practice present with an underlying AUD. with an alcohol use disorder (AUD) [2,5]. The prevalence of AUD, i.e. alcohol abuse or harmful use and alcohol dependence Alcohol use disorders among patients undergoing surgical or diagnostic procedures Alcohol use disorders (AUD) include a wide range of drinking is seen in approximately 20% of cases and nearly half of the behaviours from hazardous use of alcohol to alcohol abuse, surgical patients with AUD have alcohol dependence [6]. -

Pathophysiology and Treatment of Alcohol Withdrawal Syndrome: a Review
PATHOPHYSIOLOGY AND TREATMENT OF ALCOHOL WITHDRAWAL SYNDROME: A REVIEW Dana Bartlett, BSN, MSN, MA, CSPI Dana Bartlett is a professional nurse and author. His clinical experience includes 16 years of ICU and ER experience and over 20 years of as a poison control center information specialist. Dana has published numerous CE and journal articles, written NCLEX material and textbook chapters, and done editing and reviewing for publishers such as Elsevier, Lippincott, and Thieme. He has written widely about toxicology and was recently named a contributing editor, toxicology section, for Critical Care Nurse journal. He is currently employed at the Connecticut Poison Control Center and is actively involved in lecturing and mentoring nurses, emergency medical residents and pharmacy students. ABSTRACT Alcohol withdrawal can be mild and self-limiting but patients can also suffer serious complications and death. Providing care for a patient who is going through alcohol withdrawal is very challenging. Health clinicians with specialized knowledge, including a basic understanding of the pathophysiology of the syndrome, and an ability to make judicious decisions about medication administration are best able to support patients experiencing alcohol withdrawal. Clinicians knowledgeable about alcohol use and withdrawal need to show flexibility to change their approach to patient care as the clinical condition evolves. 1 nursece4less.com nursece4less.com nursece4less.com nursece4less.com Policy Statement This activity has been planned and implemented in accordance with the policies of NurseCe4Less.com and the continuing nursing education requirements of the American Nurses Credentialing Center's Commission on Accreditation for registered nurses. It is the policy of NurseCe4Less.com to ensure objectivity, transparency, and best practice in clinical education for all continuing nursing education (CNE) activities.