Management of Drug Overdose and Poisoning
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
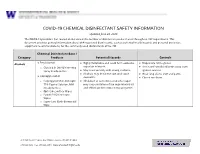
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -

Mapping the Dissociated Body
Lesley University DigitalCommons@Lesley Graduate School of Arts and Social Sciences Expressive Therapies Capstone Theses (GSASS) Spring 5-16-2020 Mapping the Dissociated Body Elizabeth Hough [email protected] Follow this and additional works at: https://digitalcommons.lesley.edu/expressive_theses Part of the Social and Behavioral Sciences Commons Recommended Citation Hough, Elizabeth, "Mapping the Dissociated Body" (2020). Expressive Therapies Capstone Theses. 239. https://digitalcommons.lesley.edu/expressive_theses/239 This Thesis is brought to you for free and open access by the Graduate School of Arts and Social Sciences (GSASS) at DigitalCommons@Lesley. It has been accepted for inclusion in Expressive Therapies Capstone Theses by an authorized administrator of DigitalCommons@Lesley. For more information, please contact [email protected], [email protected]. Running Head: MAPPING THE DISSOCIATED BODY 1 Mapping the Dissociated Body Elizabeth Hough Lesley University Running Head: MAPPING THE DISSOCIATED BODY 2 Abstract This capstone thesis explored the use of body mapping and body scans as a tool for assessing and tracking somatic dissociation and embodiment. The researcher utilized a client- centered approach and mindfulness-based interventions and theory to ground the work with the clients. While there were a variety of questionnaire-based tools for assessing dissociation with clients, many of them were lacking in the somatic component of dissociation. The available assessments were also exclusively self-reported and written or verbal, which had the potential to result in biased reporting. Clients may have also struggled to identify their level of somatic dissociation due to an inherent disconnection or dismissal of their somatic experience. This research described two case studies in which body scans and body mapping were utilized as a method to assess and track the client’s level of body dissociation and embodiment. -

Kava (Piper Methysticum) and Its Methysticin Constituents Protect Brain Tissue Against Ischemic Damage in Rodents
5 Refs: Arletti R et al, Stimulating property of Turnera diffusa and Pfaffia paniculata extracts on the sexual-behavior of male rats. Psychopharmacology 143(1), 15-19, 1999. Berger F, Handbuch der drogenkunde . Vol 2, Maudrich, Wien, 1950. Martinez M, Les plantas medicinales de Mexico . Cuarta Edicion Botas Mexico , p119, 1959. Tyler VE et al, Pharmacognosy , 9 th edition, Lea & Febiger, Philadelphia, 1988. KAVA ( Piper methysticum ) - A REVIEW The Kava plant (Piper methysticum) is a robust, well-branching and erect perennial shrub belonging to the pepper family (Piperaceae). The botanical origin remains unknown, although it is likely that early Polynesian explorers brought the plant with them from island to island. Numerous varieties of Kava exist, and today it is widely cultivated in several Pacific Island countries both for local use as well as the rapidly growing demand for pharmaceutical preparations. The dried rhizomes (roots) are normally used. The first description to the western world of the ceremonial use of an intoxicating beverage prepared from Kava was made by Captain James Cook following his Pacific voyage in 1768. The drink, prepared as an infusion in an elaborate manner after first chewing the root, is consumed on formal occasions or meetings of village elders and chiefs, as well as in reconciling with enemies and on a more social basis. It remains an important social custom in many Pacific Island countries today. Most of the islands of the Pacific possessed Kava prior to European contact, particularly those encompassed by Polynesia, Melanesia and Micronesia. After drinking the Kava beverage a pleasantly relaxed and sociable state develops, after which a deep and restful sleep occurs. -

Baclofen Overdose D
Postgraduate Medical Journal (February 1980) 56, 108-109 Postgrad Med J: first published as 10.1136/pgmj.56.652.108 on 1 February 1980. Downloaded from Baclofen overdose D. J. LIPSCOMB* T. J. MEREDITHt M.B.. M.R.C.P. M.A., M.R.C.P. *Department of Medicine, Peterborough District Hospital, Peterborough PE3 6DA, and tPoisons Unit, Guy's Hospital, London SE] 9RT Summary Case report A 57-year-old woman suffering from multiple sclerosis A 51-year-old woman, who had suffered from took an estimated 1500 mg of baclofen. She became multiple sclerosis for 15 years, was prescribed baclo- deeply unconscious with generalized flaccid muscle fen 40 mg daily as part of her treatment for spastic paralysis and absent tendon reflexes. Toxicological paraplegia. One morning, she was found lying in analysis confirmed the presence of baclofen together bed unconscious and was admitted to hospital. with small amounts of paracetamol and glutethimide. Information given by her husband suggested that an Supportive therapy, including assisted ventilation for overdose of baclofen (consisting of 152 10-mg 3 days, led to complete recovery; anticonvulsant tablets) had been taken about 2 5 hr before being drugs were necessary for the treatment of grand mal found unconscious. On arrival in hospital 90 min fits. The clinical features and treatment of baclofen later, she was deeply unconscious and unresponsive overdose are discussed. to painful stimuli. Respiration was depressed and the cough reflex was absent. She was intubated without Introduction resistance and ventilated; gastric lavage was per-Protected by copyright. Baclofen (Lioresal, Ciba) is widely used in the formed but no tablets were returned in the lavage treatment of muscle spasticity. -

Consumer Medicine Information
New Zealand Datasheet Name of Medicine DOZILE Doxylamine Succinate 25 mg Capsules Presentation Liquid filled soft gel capsules, purple, containing 25 mg doxylamine succinate. Uses Actions Doxylamine succinate is a white or creamy white powder with a characteristic odour and has solubilities of approximately 1 g/mL in water and 500 mg/mL in alcohol at 25°C. It has a pKa of 5.8 and 9.3. A 1% aqueous solution has a pH of 4.8 - 5.2. Doxylamine succinate is an ethanolamine derivative antihistamine. Because of its sedative effect, it is used for the temporary relief of sleeplessness. The drug is also used in combination with antitussives and decongestants for the temporary relief of cold and cough symptoms. It is not structurally related to the cyclic antidepressants. It is an antihistamine with hypnotic, anticholinergic, antimuscarinic and local anaesthetic effects. Duration of action is 6-8 hours. Pharmacokinetics Following oral administration of a single 25 mg dose of doxylamine succinate in healthy adults, mean peak plasma concentrations of about 100 ng/mL occur within 2- 3 hours after administration. The drug has an elimination half-life of about 10 hours in healthy adults. Absorption It is easily absorbed from the gastrointestinal tract. Following an oral dose of 25 mg the mean peak plasma level is 99 ng/mL 2.4 hours after ingestion. This level declines to 28 ng/mL at 24 hours and 10 ng/mL at 36 hours. Distribution The apparent volume of distribution is 2.5 L/kg. Metabolism The major metabolic pathways are N-demethylation, N-oxidation, hydroxylation, N- acetylation, N-desalkylation and ether cleavage. -

Use of Ceftaroline Fosamil in Children: Review of Current Knowledge and Its Application
Infect Dis Ther (2017) 6:57–67 DOI 10.1007/s40121-016-0144-8 REVIEW Use of Ceftaroline Fosamil in Children: Review of Current Knowledge and its Application Juwon Yim . Leah M. Molloy . Jason G. Newland Received: November 10, 2016 / Published online: December 30, 2016 Ó The Author(s) 2016. This article is published with open access at Springerlink.com ABSTRACT infections, CABP caused by penicillin- and ceftriaxone-resistant S. pneumoniae and Ceftaroline is a novel cephalosporin recently resistant Gram-positive infections that fail approved in children for treatment of acute first-line antimicrobial agents. However, bacterial skin and soft tissue infections and limited data are available on tolerability in community-acquired bacterial pneumonia neonates and infants younger than 2 months (CABP) caused by methicillin-resistant of age, and on pharmacokinetic characteristics Staphylococcus aureus, Streptococcus pneumoniae in children with chronic medical conditions and other susceptible bacteria. With a favorable and those with invasive, complicated tolerability profile and efficacy proven in infections. In this review, the microbiological pediatric patients and excellent in vitro profile of ceftaroline, its mechanism of action, activity against resistant Gram-positive and and pharmacokinetic profile will be presented. Gram-negative bacteria, ceftaroline may serve Additionally, clinical evidence for use in as a therapeutic option for polymicrobial pediatric patients and proposed place in therapy is discussed. Enhanced content To view enhanced content for this article go to http://www.medengine.com/Redeem/ 1F47F0601BB3F2DD. Keywords: Antibiotic resistance; Ceftaroline J. Yim (&) fosamil; Children; Methicillin-resistant St. John Hospital and Medical Center, Detroit, MI, Staphylococcus aureus; Streptococcus pneumoniae USA e-mail: [email protected] L. -

Alternative Treatments for Depression and Anxiety
2019 PCB Conference: Strickland Benzodiazepines (BZDs), Herbal and Alternative Treatments for Anxiety & Depression BZD Learning Objectives • List at least three uses for benzodiazepines • Discuss at least two risk factors associated with benzodiazepine prescriptions Craig Strickland, PhD, Owner Biobehavioral Education and Consultation https://sites.google.com/site/bioedcon 1 2 BZD Pharmacokinetics Clinical Uses of BZDs Generic Name Trade Name Rapidity ½ Life Dose (mg) • Treat a variety of anxiety disorders alprazolam Xanax Intermediate Short 0.75-4 • Hypnotics • Muscle relaxants chlordiaze- Librium Intermediate Long 15-100 poxide • To produce anterograde amnesia clonazepam Klonopin Intermediate Long 0.5-4 • Alcohol & other CNS depressant withdrawal • Anti-convulsant therapy diazepam Valium Rapid Long 4-40 triazolam Halcion Intermediate Very short 0.125-0.5 temazepam Restoril Short Short 7.5-30 3 4 1 2019 PCB Conference: Strickland Issues with BZDs Herbal Medication and Alternative Therapies Used in the Treatment of Depression and Anxiety • Addictive potential • Confusion between “anti-anxiety” effects and the “warm-fuzzy) • Large dose ranges • Comparison of BZDs with medications like Buspar, etc. • They work, they work well and they work quickly 5 6 Alternative Tx. Learning Objectives Background Information on herbals: Natural does not necessarily mean “safe” • List several amino acid treatments for depression • Side-effects and adverse reactions • List at least three of the most common herbal – Herbal medications are “drugs” although -

Adansonia Digitata L
Veterinary World, EISSN: 2231-0916 RESEARCH ARTICLE Available at www.veterinaryworld.org/Vol.7/July-2014/10.pdf Open Access Antidiarrhoeal effect of the crude methanol extract of the dried fruit of Adansonia digitata L. (Malvaceae) Mohammed Musa Suleiman1111 , Mohammed Mamman , Ibrahim Hassan , Shamsu Garba , Mohammed Umaru Kawu21 and Patricia Ishaku Kobo 1. Department of Pharmacology and Toxicology, Faculty of Veterinary Medicine, Ahmadu Bello University, Zaria, Nigeria; 2. Department of Physiology, Faculty of Veterinary Medicine, Ahmadu Bello University, Zaria, Nigeria. Corresponding author: Mohammed Musa Suleiman, email:[email protected] MM: [email protected], IH: [email protected], SG: [email protected], MUK: [email protected], PIK: [email protected] Received:06-04-2014, Revised: 12-06-2014, Accepted: 14-06-2014, Published online: 19-07-2014 doi: 10.14202/vetworld.2014.495-500 How to cite this article: Suleiman MM, Mamman M, Hassan I, Garba S, Kawu MUand Kobo PI (2014) Antidiarrhoeal effect of the crude methanol extract of the dried fruit ofAdansonia digitata L. (Malvaceae), Veterinary World 7(7): 495-500. Abstract Aim: The study was designed to evaluate the antidiarrhoeal property of the methanol extract of the fruit of Adansonia digitata using laboratory animal models. Materials and Methods : The acute oral toxicity (LD50 ) of the extract was determined in mice, while the antidiarrhoeal effect of different doses of the extract was evaluated in both mice and rats. The effect of the extract at doses of 300, 700 and 1000 mg/kg were tested against intestinal transit time, magnesium sulphate-induced gastrointestinal motility test and castor oil- induced diarrhoea in mice. -

The Use of Intravenous Baclofen As Therapy for the Γ-Hydroxybutyric Acid Withdrawal Syndrome
Research Article Remedy Open Access Published: 12 Jun, 2017 The Use of Intravenous Baclofen as Therapy for the γ-hydroxybutyric Acid Withdrawal Syndrome Marc Sabbe1*, Francis Desmet1 and Sabrina Dewinter2 1Department of Emergency Medicine, University Hospitals, Catholic University of Leuven, Belgium 2Department of Pharmacy, University Hospitals, Catholic University of Leuven, Belgium Abstract Introduction: In this case series with three patients, we introduced baclofen, a γ-aminobutyric acid type B(GABA-B) receptor agonist, for treatment of the γ-hydroxybutyric acid (GHB) withdrawal syndrome. Materials and Methods: Single center case series performed on three patientswith a GHB withdrawal syndrome. They initially received massive doses of benzodiazepines, without sufficient effect. Two patients also received an unsuccessful continuous dexmedetomidine drip. In all patients, intravenous baclofen was started, with an intravenous loading dose between 0.5 and 2 milligrams (mg) to achieve a therapeutic level. Thereafter a continuous intravenous dose between 0.5 and 1 mg per hour for 12 h was administered to maintain a steady state. After that, baclofen was substituted orally with a daily oral dose varying between 20 mg and 40 mg which could be downgraded and stopped over the next days. They all continued to receive a standard benzodiazepine regimen during the baclofen trial. Results and Discussion: Main outcome measurements were the degree of withdrawal symptoms and the need for benzodiazepines during baclofen treatment. In all patients, a significant reduction of the GHB withdrawal syndrome was noted. A standard daily regimen of baseline benzodiazepine dosing between 40 mg and 80 mg diazepam was sufficient. Adverse effects of baclofen use were absent. -

In Vivo Evaluation of Antidiarrhoeal Activity of the Leaves of Azima Tetracantha Linn
Vol.5(8), pp. 140-144, December, 2013 DOI: 10.5897/IJNAM2013.0152 International Journal of Nutrition and ISSN 2141-2340 ©2013 Academic Journals http://www.academicjournals.org/IJNAM Metabolism Full Length Research Paper In vivo evaluation of antidiarrhoeal activity of the leaves of Azima tetracantha Linn V. Hazeena Begum*, M. Dhanalakshmi and P. Muthukumaran Department of Siddha Medicine, Faculty of Science, Tamil University, Vakaiyur, Thanjavur 613 010, Tamilnadu, India. Accepted 3 October, 2013 The aqueous crude extract of the leaves of Azima tetracantha was studied for its phytochemical constituents and antidiarrhoeal activity using castor oil-induced diarrhoea and castor oil-induced enteropooling in rats. The phytochemical studies of the aqueous extract revealed the presence of alkaloids, flavonoids, tannins and saponins. The extract showed significant (p < 0.001) protection against castor oil-induced diarrhoea and castor oil-induced enteropooling at (100 mg/kg). The presence of some of the phytochemicals in the root extract may be responsible for the observed effects, and also the basis for its use in traditional medicine as antidiarrhoeal drug. Key words: Azima tetracantha, enteropooling, anti-diarrhoeal. INTRODUCTION Diarrhoea is characterized by increased frequency of powerful diuretic given in rheumatism, dropsy, dyspepsia bowel movement, wet stool and abdominal pain and chronic diarrhoea and as a stimulant tonic after (Ezekwesili et al., 2004). It is a leading cause of confinement (Nadkarni, 1976). A. tetracantha as efficient malnutrition and death among children in the developing acute phase anti-inflammatory drug is traditionally used countries of the world today (Victoria et al., 2000). Many by Indian medical practitioners (Ismail et al., 1997). -

Adverse Drug Reactions Sample Chapter
Sample copyright Pharmaceutical Press www.pharmpress.com 5 Drug-induced skin reactions Anne Lee and John Thomson Introduction Cutaneous drug eruptions are one of the most common types of adverse reaction to drug therapy, with an overall incidence rate of 2–3% in hos- pitalised patients.1–3 Almost any medicine can induce skin reactions, and certain drug classes, such as non-steroidal anti-inflammatory drugs (NSAIDs), antibiotics and antiepileptics, have drug eruption rates approaching 1–5%.4 Although most drug-related skin eruptions are not serious, some are severe and potentially life-threatening. Serious reac- tions include angio-oedema, erythroderma, Stevens–Johnson syndrome and toxic epidermal necrolysis. Drug eruptions can also occur as part of a spectrum of multiorgan involvement, for example in drug-induced sys- temic lupus erythematosus (see Chapter 11). As with other types of drug reaction, the pathogenesis of these eruptions may be either immunological or non-immunological. Healthcare professionals should carefully evalu- ate all drug-associated rashes. It is important that skin reactions are identified and documented in the patient record so that their recurrence can be avoided. This chapter describes common, serious and distinctive cutaneous reactions (excluding contact dermatitis, which may be due to any external irritant, including drugs and excipients), with guidance on diagnosis and management. A cutaneous drug reaction should be suspected in any patient who develops a rash during a course of drug therapy. The reaction may be due to any medicine the patient is currently taking or has recently been exposed to, including prescribed and over-the-counter medicines, herbal or homoeopathic preparations, vaccines or contrast media. -

Benzodiazepine & Alcohol Co-Ingestion
The Journal of COLLEGIATE EMERGENCY MEDICAL SERVICES ISSN: 2576-3687 (Print) 2576-3695 (Online) Journal Website: https://www.collegeems.com Benzodiazepine & Alcohol Co-Ingestion: Implications for Collegiate-Based Emergency Medical Services David Goroff & Alexander Farinelli Keywords: alcohol, benzodiazepines, collegiate-based emergency medical services, toxicology Citation (AMA Style): Goroff D, Farinelli A. Benzodiazepine and Alcohol Co-In- gestion. J Coll Emerg Med Serv. 2018; 1(2): 19-23. https://doi.org/10.30542/ JCEMS.2018.01.02.04 Electronic Link: https://doi.org/10.30542/JCEMS.2018.01.02.04 Published Online: August 8, 2018 Published in Print: August 13, 2018 (Volume 1: Issue 2) Copyright: © 2018 Goroff & Farinelli. This is an OPEN ACCESS article distributed under the terms of the Creative Commons Attribu- tion 4.0 International (CC BY 4.0) License, which permits unrestrict- ed use, distribution, and reproduction in any medium, provided the original author and source are credited. The full license is available at: https://creativecommons.org/licenses/by/4.0/ CLINICAL REVIEW Benzodiazepine & Alcohol Co-Ingestion: Implications for Collegiate-Based Emergency Medical Services David Goroff, MS, NRP & Alexander Farinelli, BS, NRP ABSTRACT KEYWORDS: alcohol, The co-ingestion of benzodiazepines and alcohol presents a unique challenge to colle- benzodiazepines, collegiate- giate EMS providers, due to the pharmacological interaction of the two substances and based emergency medical the variable patient presentations. Given the likelihood that collegiate EMS providers services, toxicology will be called to treat a patient who has co-ingested benzodiazepines and alcohol, this Corresponding Author and review discusses the relevant pharmacology, clinical presentation, and treatment of these Author Affiliations:Listed co-ingestion patients.