Nalidixic Acid, USP)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications
International Journal of Molecular Sciences Review Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications Daniel Fernández-Villa 1, Maria Rosa Aguilar 1,2 and Luis Rojo 1,2,* 1 Instituto de Ciencia y Tecnología de Polímeros, Consejo Superior de Investigaciones Científicas, CSIC, 28006 Madrid, Spain; [email protected] (D.F.-V.); [email protected] (M.R.A.) 2 Consorcio Centro de Investigación Biomédica en Red de Bioingeniería, Biomateriales y Nanomedicina, 28029 Madrid, Spain * Correspondence: [email protected]; Tel.: +34-915-622-900 Received: 18 September 2019; Accepted: 7 October 2019; Published: 9 October 2019 Abstract: Bacterial, protozoan and other microbial infections share an accelerated metabolic rate. In order to ensure a proper functioning of cell replication and proteins and nucleic acids synthesis processes, folate metabolism rate is also increased in these cases. For this reason, folic acid antagonists have been used since their discovery to treat different kinds of microbial infections, taking advantage of this metabolic difference when compared with human cells. However, resistances to these compounds have emerged since then and only combined therapies are currently used in clinic. In addition, some of these compounds have been found to have an immunomodulatory behavior that allows clinicians using them as anti-inflammatory or immunosuppressive drugs. Therefore, the aim of this review is to provide an updated state-of-the-art on the use of antifolates as antibacterial and immunomodulating agents in the clinical setting, as well as to present their action mechanisms and currently investigated biomedical applications. Keywords: folic acid antagonists; antifolates; antibiotics; antibacterials; immunomodulation; sulfonamides; antimalarial 1. -

A TWO-YEAR RETROSPECTIVE ANALYSIS of ADVERSE DRUG REACTIONS with 5PSQ-031 FLUOROQUINOLONE and QUINOLONE ANTIBIOTICS 24Th Congress Of
A TWO-YEAR RETROSPECTIVE ANALYSIS OF ADVERSE DRUG REACTIONS WITH 5PSQ-031 FLUOROQUINOLONE AND QUINOLONE ANTIBIOTICS 24th Congress of V. Borsi1, M. Del Lungo2, L. Giovannetti1, M.G. Lai1, M. Parrilli1 1 Azienda USL Toscana Centro, Pharmacovigilance Centre, Florence, Italy 2 Dept. of Neurosciences, Psychology, Drug Research and Child Health (NEUROFARBA), 27-29 March 2019 Section of Pharmacology and Toxicology , University of Florence, Italy BACKGROUND PURPOSE On 9 February 2017, the Pharmacovigilance Risk Assessment Committee (PRAC) initiated a review1 of disabling To review the adverse drugs and potentially long-lasting side effects reported with systemic and inhaled quinolone and fluoroquinolone reactions (ADRs) of antibiotics at the request of the German medicines authority (BfArM) following reports of long-lasting side effects systemic and inhaled in the national safety database and the published literature. fluoroquinolone and quinolone antibiotics that MATERIAL AND METHODS involved peripheral and central nervous system, Retrospective analysis of ADRs reported in our APVD involving ciprofloxacin, flumequine, levofloxacin, tendons, muscles and joints lomefloxacin, moxifloxacin, norfloxacin, ofloxacin, pefloxacin, prulifloxacin, rufloxacin, cinoxacin, nalidixic acid, reported from our pipemidic given systemically (by mouth or injection). The period considered is September 2016 to September Pharmacovigilance 2018. Department (PVD). RESULTS 22 ADRs were reported in our PVD involving fluoroquinolone and quinolone antibiotics in the period considered and that affected peripheral or central nervous system, tendons, muscles and joints. The mean patient age was 67,3 years (range: 17-92 years). 63,7% of the ADRs reported were serious, of which 22,7% caused hospitalization and 4,5% caused persistent/severe disability. 81,8% of the ADRs were reported by a healthcare professional (physician, pharmacist or other) and 18,2% by patient or a non-healthcare professional. -

A Review of Enrofloxacin for Veterinary Use Tessa Trouchon, Sebastien Lefebvre
A Review of Enrofloxacin for Veterinary Use Tessa Trouchon, Sebastien Lefebvre To cite this version: Tessa Trouchon, Sebastien Lefebvre. A Review of Enrofloxacin for Veterinary Use. Open Journal of Veterinary Medicine, 2016, 6 (2), pp.40-58. 10.4236/ojvm.2016.62006. hal-01503397 HAL Id: hal-01503397 https://hal.archives-ouvertes.fr/hal-01503397 Submitted on 7 Apr 2017 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Distributed under a Creative Commons Attribution - NoDerivatives| 4.0 International License Open Journal of Veterinary Medicine, 2016, 6, 40-58 Published Online February 2016 in SciRes. http://www.scirp.org/journal/ojvm http://dx.doi.org/10.4236/ojvm.2016.62006 A Review of Enrofloxacin for Veterinary Use Tessa Trouchon, Sébastien Lefebvre USC 1233 INRA-Vetagro Sup, Veterinary School of Lyon, Marcy l’Etoile, France Received 12 January 2016; accepted 21 February 2016; published 26 February 2016 Copyright © 2016 by authors and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract This review outlines the current knowledge on the use of enrofloxacin in veterinary medicine from biochemical mechanisms to the use in the field conditions and even resistance and ecotoxic- ity. -

AMEG Categorisation of Antibiotics
12 December 2019 EMA/CVMP/CHMP/682198/2017 Committee for Medicinal Products for Veterinary use (CVMP) Committee for Medicinal Products for Human Use (CHMP) Categorisation of antibiotics in the European Union Answer to the request from the European Commission for updating the scientific advice on the impact on public health and animal health of the use of antibiotics in animals Agreed by the Antimicrobial Advice ad hoc Expert Group (AMEG) 29 October 2018 Adopted by the CVMP for release for consultation 24 January 2019 Adopted by the CHMP for release for consultation 31 January 2019 Start of public consultation 5 February 2019 End of consultation (deadline for comments) 30 April 2019 Agreed by the Antimicrobial Advice ad hoc Expert Group (AMEG) 19 November 2019 Adopted by the CVMP 5 December 2019 Adopted by the CHMP 12 December 2019 Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2020. Reproduction is authorised provided the source is acknowledged. Categorisation of antibiotics in the European Union Table of Contents 1. Summary assessment and recommendations .......................................... 3 2. Introduction ............................................................................................ 7 2.1. Background ........................................................................................................ -

Nitroaromatic Antibiotics As Nitrogen Oxide Sources
Review biomolecules Nitroaromatic Antibiotics as Nitrogen Oxide Sources Review Allison M. Rice, Yueming Long and S. Bruce King * Nitroaromatic Antibiotics as Nitrogen Oxide Sources Department of Chemistry and Biochemistry, Wake Forest University, Winston-Salem, NC 27101, USA; Allison M. Rice , Yueming [email protected] and S. Bruce (A.M.R.); King [email protected] * (Y.L.) * Correspondence: [email protected]; Tel.: +1-336-702-1954 Department of Chemistry and Biochemistry, Wake Forest University, Winston-Salem, NC 27101, USA; [email protected]: Nitroaromatic (A.M.R.); [email protected] antibiotics (Y.L.) show activity against anaerobic bacteria and parasites, finding * Correspondence: [email protected]; Tel.: +1-336-702-1954 use in the treatment of Heliobacter pylori infections, tuberculosis, trichomoniasis, human African trypanosomiasis, Chagas disease and leishmaniasis. Despite this activity and a clear need for the Abstract: Nitroaromatic antibiotics show activity against anaerobic bacteria and parasites, finding usedevelopment in the treatment of new of Heliobacter treatments pylori forinfections, these conditio tuberculosis,ns, the trichomoniasis, associated toxicity human Africanand lack of clear trypanosomiasis,mechanisms of action Chagas have disease limited and their leishmaniasis. therapeutic Despite development. this activity Nitroaro and a clearmatic need antibiotics for require thereductive development bioactivation of new treatments for activity for theseand this conditions, reductive the associatedmetabolism toxicity can convert -

Therapeutic Class Overview Fluoroquinolones
Therapeutic Class Overview Fluoroquinolones INTRODUCTION The fluoroquinolones are broad-spectrum antibiotics grouped into generations based on their spectrum of activity (Bolon 2011). ○ First generation agents, which are structurally quinolones rather than fluoroquinolones, possess activity against aerobic gram-negative bacteria but are not effective against aerobic gram-positive bacteria or anaerobes. The first generation agents (eg, nalidixic acid, cinoxacin) are no longer on the market. ○ Second generation agents, the original fluoroquinolones, contain a fluorine atom at position C-6. These agents offer improved coverage against gram-negative bacteria and moderately improved gram-positive coverage. The available second generation fluoroquinolones include ciprofloxacin, levofloxacin, and ofloxacin. Lomefloxacin and norfloxacin are second generation agents which are no longer on the market. ○ Third generation agents achieve greater potency against gram-positive bacteria, particularly pneumococci, and also possess good activity against anaerobes. All 3 of the third generation agents, gatifloxacin, grepafloxacin, and sparfloxacin, were removed from the market due to toxicities. ○ Fourth generation fluoroquinolones have superior coverage against pneumococci and anaerobes. The available agent is moxifloxacin. Trovafloxacin, was removed from the market due to toxicities, and there is a drug shortage of gemifloxacin. ○ The most recently approved fluoroquinolone, delafloxacin, has an even broader spectrum of antibiotic activity and is commonly referred to as a “next generation” fluoroquinolone. The fluoroquinolones have been used to treat a variety of infections including urinary tract infections, sinusitis, lower respiratory tract infections, intra-abdominal infections, infectious diarrhea, skin and skin structure infections, sexually transmitted diseases, and bacterial prostatitis. A few of the agents also have Food and Drug Administration (FDA) approval for inhalational anthrax and plague. -

Which Antibiotics for UTI?
RESEARCH HIGHLIGHTS INFECTION PROSTATE CANCER Which antibiotics Surfaceome profiling for NEPC for UTI? target antigens Prostate adenocarcinoma and was enriched in NEPC. Comparison A multinational, open-label, analyst- blinded, randomized neuroendocrine prostate cancer of the genes to identify molecular clinical trial has shown that 5-day nitrofurantoin is more (NEPC) have distinct surfaceomes, functions showed that those enriched likely to result in clinical and microbiological resolution of which can be used to discriminate in NEPC were related to neural acute, uncomplicated lower urinary tract infection (UTI) than between the subtypes and might provide function, including synaptic signalling, single- dose fosfomycin. These results could influence future target antigens for immunotherapy. nervous system development, treatment decisions for managing UTI. The advent of CAR T cell therapy and neurotransmitter transport, This study included 513 women aged >18 years who were shows the potential of targeting whereas those of adenocarcinoma not pregnant and had at least one symptom of acute lower UTI treatment to cell-surface markers. were involved in secretion, immune (including dysuria, urgency, frequency, and/or suprapubic However, identifying target antigens response, and inflammatory response, tenderness), a positive urine dipstick test, and no known in prostate tumours — NEPC in enabling differentiation of the subtypes. colonization or previous infection with antibiotic-resistant particular — is problematic, as markers RNA sequencing (RNA- seq) uropathogens. Participants were randomly assigned 1:1 to upregulated in adenocarcinoma gene expression analysis of receive 100 mg nitrofurantoin orally three times a day for 5 days are often downregulated in human prostate cancer cell lines or 3 g fosfomycin orally as a single dose. -

The Nitroimidazole Family of Drugs
Br J Vener Dis: first published as 10.1136/sti.54.2.69 on 1 April 1978. Downloaded from British Journal of Venereal Diseases, 1978, 54, 69-71 Editorial The nitroimidazole family of drugs In 1955 an antibiotic complex isolated from a operative infection caused by susceptible anaerobes, strain of Streptomyces on the island of Reunion particularly in gynaecological surgery, appendi- was found by research workers of Rhone-Poulenc in cectomy, and colonic surgery. Paris to contain a trichomonacidal antibiotic- Real innovations in chemotherapy, such as azomycin. It had previously been isolated in Japan metronidazole, always attract attention from other (Maeda et al., 1953) and identified as 2-nitroimi- research groups. Although interest was slow to dazole (Ia see Table) (Nakamura, 1955). At the develop, research workers have sought analogous, time, and for some years after, this remarkably structurally-modified compounds which might afford simple compound defied synthesis, but it stimulated some advantage in clinical use-for example, the workers at Rhone-Poulenc to prepare and test greater potency, better tolerance and freedom from the activity of the more readily accessible isomeric side effects, a broader spectrum of action, a longer 5-nitroimidazoles (II). It was their good fortune in duration of action, or in some other characteristic. 1957 to find that these isomers were more active This effort has been concerned with important antiprotozoal agents than the natural product veterinary uses of 5-nitroimidazoles as well as the (Cosar and Julou, 1959). In a series of 150 related applications in human medicine. compounds, the one with a P-hydroxyethyl group Metronidazole has been a difficult target to in the 1-position gave the best compromise between improve upon, but several other drugs of this activity and toxicity and this brand of metroni- chemical family have been introduced to clinical dazole was introduced as Flagyl. -

Paper I and II)
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1335 Constraints on up-regulation of drug efflux in the evolution of ciprofloxacin resistance LISA PRASKI ALZRIGAT ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6206 ISBN 978-91-554-9923-5 UPPSALA urn:nbn:se:uu:diva-320580 2017 Dissertation presented at Uppsala University to be publicly examined in B22, BMC, Husargatan 3, Uppsala, Friday, 9 June 2017 at 09:00 for the degree of Doctor of Philosophy (Faculty of Medicine). The examination will be conducted in English. Faculty examiner: Professor Fernando Baquero (Departamento de Microbiología, Hospital Universitario Ramón y Cajal, Instituto Ramón y Cajal de Investigación Sanitaria (IRYCIS), Madrid, Spain). Abstract Praski Alzrigat, L. 2017. Constraints on up-regulation of drug efflux in the evolution of ciprofloxacin resistance. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1335. 48 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-554-9923-5. The crucial role of antibiotics in modern medicine, in curing infections and enabling advanced medical procedures, is being threatened by the increasing frequency of resistant bacteria. Better understanding of the forces selecting resistance mutations could help develop strategies to optimize the use of antibiotics and slow the spread of resistance. Resistance to ciprofloxacin, a clinically important antibiotic, almost always involves target mutations in DNA gyrase and Topoisomerase IV. Because ciprofloxacin is a substrate of the AcrAB-TolC efflux pump, mutations causing pump up-regulation are also common. Studying the role of efflux pump-regulatory mutations in the development of ciprofloxacin resistance, we found a strong bias against gene-inactivating mutations in marR and acrR in clinical isolates. -
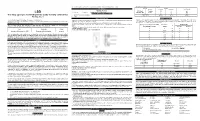
(LSD) Test Dip Card (Urine) • Specimen Collection Container % Agreement 98.8% 99
frozen and stored below -20°C. Frozen specimens should be thawed and mixed before testing. GC/MS. The following results were tabulated: Method GC/MS MATERIALS Total Results Results Positive Negative Materials Provided LSD Rapid Positive 79 1 80 LSD • Test device • Desiccants • Package insert • Urine cups Test Dip card Negative 1 99 100 Materials Required But Not Provided Total Results 80 100 180 One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) • Specimen collection container % Agreement 98.8% 99. % 98.9% • Timer Package Insert DIRECTIONS FOR USE Analytical Sensitivity This Instruction Sheet is for testing of Lysergic acid diethylamide. Allow the test device, and urine specimen to come to room temperature [15-30°C (59-86°F)] prior to testing. A drug-free urine pool was spiked with LSD at the following concentrations: 0 ng/mL, -50%cutoff, -25%cutoff, cutoff, A rapid, one step test for the qualitative detection of Lysergic acid diethylamide and its metabolites in human urine. 1) Remove the test device from the foil pouch. +25%cutoff and +50%cutoff. The result demonstrates >99% accuracy at 50% above and 50% below the cut-off For forensic use only. 2) Remove the cap from the test device. Label the device with patient or control identifications. concentration. The data are summarized below: INTENDED USE 3) Immerse the absorbent tip into the urine sample for 10-15 seconds. Urine sample should not touch the plastic Lysergic acid diethylamide (LSD) Percent of Visual Result The One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) is a lateral flow chromatographic device. -

WHO Report on Surveillance of Antibiotic Consumption: 2016-2018 Early Implementation ISBN 978-92-4-151488-0 © World Health Organization 2018 Some Rights Reserved
WHO Report on Surveillance of Antibiotic Consumption 2016-2018 Early implementation WHO Report on Surveillance of Antibiotic Consumption 2016 - 2018 Early implementation WHO report on surveillance of antibiotic consumption: 2016-2018 early implementation ISBN 978-92-4-151488-0 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons. org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non- commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. WHO report on surveillance of antibiotic consumption: 2016-2018 early implementation. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data.