Therapeutic Class Overview Fluoroquinolones
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A TWO-YEAR RETROSPECTIVE ANALYSIS of ADVERSE DRUG REACTIONS with 5PSQ-031 FLUOROQUINOLONE and QUINOLONE ANTIBIOTICS 24Th Congress Of
A TWO-YEAR RETROSPECTIVE ANALYSIS OF ADVERSE DRUG REACTIONS WITH 5PSQ-031 FLUOROQUINOLONE AND QUINOLONE ANTIBIOTICS 24th Congress of V. Borsi1, M. Del Lungo2, L. Giovannetti1, M.G. Lai1, M. Parrilli1 1 Azienda USL Toscana Centro, Pharmacovigilance Centre, Florence, Italy 2 Dept. of Neurosciences, Psychology, Drug Research and Child Health (NEUROFARBA), 27-29 March 2019 Section of Pharmacology and Toxicology , University of Florence, Italy BACKGROUND PURPOSE On 9 February 2017, the Pharmacovigilance Risk Assessment Committee (PRAC) initiated a review1 of disabling To review the adverse drugs and potentially long-lasting side effects reported with systemic and inhaled quinolone and fluoroquinolone reactions (ADRs) of antibiotics at the request of the German medicines authority (BfArM) following reports of long-lasting side effects systemic and inhaled in the national safety database and the published literature. fluoroquinolone and quinolone antibiotics that MATERIAL AND METHODS involved peripheral and central nervous system, Retrospective analysis of ADRs reported in our APVD involving ciprofloxacin, flumequine, levofloxacin, tendons, muscles and joints lomefloxacin, moxifloxacin, norfloxacin, ofloxacin, pefloxacin, prulifloxacin, rufloxacin, cinoxacin, nalidixic acid, reported from our pipemidic given systemically (by mouth or injection). The period considered is September 2016 to September Pharmacovigilance 2018. Department (PVD). RESULTS 22 ADRs were reported in our PVD involving fluoroquinolone and quinolone antibiotics in the period considered and that affected peripheral or central nervous system, tendons, muscles and joints. The mean patient age was 67,3 years (range: 17-92 years). 63,7% of the ADRs reported were serious, of which 22,7% caused hospitalization and 4,5% caused persistent/severe disability. 81,8% of the ADRs were reported by a healthcare professional (physician, pharmacist or other) and 18,2% by patient or a non-healthcare professional. -

AMEG Categorisation of Antibiotics
12 December 2019 EMA/CVMP/CHMP/682198/2017 Committee for Medicinal Products for Veterinary use (CVMP) Committee for Medicinal Products for Human Use (CHMP) Categorisation of antibiotics in the European Union Answer to the request from the European Commission for updating the scientific advice on the impact on public health and animal health of the use of antibiotics in animals Agreed by the Antimicrobial Advice ad hoc Expert Group (AMEG) 29 October 2018 Adopted by the CVMP for release for consultation 24 January 2019 Adopted by the CHMP for release for consultation 31 January 2019 Start of public consultation 5 February 2019 End of consultation (deadline for comments) 30 April 2019 Agreed by the Antimicrobial Advice ad hoc Expert Group (AMEG) 19 November 2019 Adopted by the CVMP 5 December 2019 Adopted by the CHMP 12 December 2019 Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2020. Reproduction is authorised provided the source is acknowledged. Categorisation of antibiotics in the European Union Table of Contents 1. Summary assessment and recommendations .......................................... 3 2. Introduction ............................................................................................ 7 2.1. Background ........................................................................................................ -

Use of Antipsychotic Medications in Nursing Facility Residents
POLICY Use of Antipsychotic Medications in Nursing Facility Residents Preamble The Office of Inspector General of the U. S. Department of Health and Human Services issued a report in May 2011 finding that 14% of elderly nursing home residents had Medicare claims for atypical antipsychotic drugs.1 In addition, 83% of the above Medicare claims for atypical antipsychotics for these elderly nursing home residents were for off---label indications. In 2005, the U. S. Food and Drug Administration required manufacturers of atypical antipsychotic medications to include a boxed warning that these antipsychotics may increase the risk of death in elderly persons with psychosis related to dementia. This warning was expanded to all antipsychotic drugs in 2008. The OIG report found that 88% of the use of atypical antipsychotics was in persons for whom this warning is applicable. As part of the report, OIG conducted medical record reviews on 600 elderly nursing facility residents. They found that 22% of the atypical antipsychotic medications were not administered in accordance with standards from the Centers for Medicare & Medicaid Services relating to unnecessary drug use in nursing homes. This controversial report from the OIG has generated concern about the use of antipsychotics in patients with dementia, and also criticism of the report itself.2 ---4 This document will provide additional background on this subject and a position statement from the American Society of Consultant Pharmacists. Background Understanding the findings and implications of the OIG report on use of atypical antipsychotics in nursing home residents requires placing the report findings into a proper context. Shown below are key points to understanding this report. -

Paper I and II)
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1335 Constraints on up-regulation of drug efflux in the evolution of ciprofloxacin resistance LISA PRASKI ALZRIGAT ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6206 ISBN 978-91-554-9923-5 UPPSALA urn:nbn:se:uu:diva-320580 2017 Dissertation presented at Uppsala University to be publicly examined in B22, BMC, Husargatan 3, Uppsala, Friday, 9 June 2017 at 09:00 for the degree of Doctor of Philosophy (Faculty of Medicine). The examination will be conducted in English. Faculty examiner: Professor Fernando Baquero (Departamento de Microbiología, Hospital Universitario Ramón y Cajal, Instituto Ramón y Cajal de Investigación Sanitaria (IRYCIS), Madrid, Spain). Abstract Praski Alzrigat, L. 2017. Constraints on up-regulation of drug efflux in the evolution of ciprofloxacin resistance. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1335. 48 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-554-9923-5. The crucial role of antibiotics in modern medicine, in curing infections and enabling advanced medical procedures, is being threatened by the increasing frequency of resistant bacteria. Better understanding of the forces selecting resistance mutations could help develop strategies to optimize the use of antibiotics and slow the spread of resistance. Resistance to ciprofloxacin, a clinically important antibiotic, almost always involves target mutations in DNA gyrase and Topoisomerase IV. Because ciprofloxacin is a substrate of the AcrAB-TolC efflux pump, mutations causing pump up-regulation are also common. Studying the role of efflux pump-regulatory mutations in the development of ciprofloxacin resistance, we found a strong bias against gene-inactivating mutations in marR and acrR in clinical isolates. -

AVELOX Or Other Quinolones (4, 5.6) AVELOX® Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------------CONTRAINDICATIONS----------------------------- These highlights do not include all the information needed to use Known hypersensitivity to AVELOX or other quinolones (4, 5.6) AVELOX® safely and effectively. See full prescribing information for AVELOX. -----------------------WARNINGS AND PRECAUTIONS----------------------- AVELOX® (moxifloxacin hydrochloride) Tablet, film-coated • Increased risk of tendinitis and tendon rupture. This risk is further increased AVELOX® (moxifloxacin hydrochloride) Injection, solution for IV use in older patients usually over 60 years of age, in patients taking Initial U.S. Approval: 1999 corticosteroids, and in patients with kidney, heart or lung transplants. To reduce the development of drug-resistant bacteria and maintain the Discontinue if pain or inflammation in a tendon occurs. (5.1, 8.5) effectiveness of AVELOX and other antibacterial drugs, AVELOX should be • Prolongation of the QT interval and isolated cases of torsade de pointes has used only to treat or prevent infections that are proven or strongly suspected to been reported. Avoid use in patients with known prolongation, hypokalemia, be caused by susceptible bacteria. and with drugs that prolong the QT interval. (5.2, 7.4, 8.5). Use caution in patients with proarrhythmic conditions such as clinically significant bradycardia or acute myocardial ischemia. (5.2) WARNING: • Serious and sometimes fatal hypersensitivity reactions, including Fluoroquinolones, including AVELOX®, are associated with an anaphylactic reactions, may occur after first or subsequent doses. increased risk of tendinitis and tendon rupture in all ages. This risk is Discontinue drug use at first sign of skin rash, jaundice or any other sign of further increased in older patients usually over 60 years of age, in hypersensitivity. -

Depo-Provera Contraceptive Injection Should Not Be Used As a Long
HIGHLIGHTS OF PRESCRIBING INFORMATION • Known hypersensitivity to Depo-Provera CI (medroxyprogesterone These highlights do not include all the information needed to use DEPO- acetate or any of its other ingredients). (4) PROVERA CI safely and effectively. See full prescribing information for • Significant liver disease. (4) DEPO-PROVERA CI. • Undiagnosed vaginal bleeding. (4) DEPO-PROVERA CI (medroxyprogesterone acetate) injectable ------------------------------WARNINGS AND PRECAUTIONS----------------- suspension, for intramuscular use Thromboembolic Disorders: Discontinue Depo-Provera CI in patients who develop thrombosis (5.2) Initial U.S. Approval: 1959 Cancer Risks: Monitor women with breast nodules or a strong family WARNING: LOSS OF BONE MINERAL DENSITY history of breast cancer carefully. (5.3) • Women who use Depo-Provera Contraceptive Injection (Depo- Ectopic Pregnancy: Consider ectopic pregnancy if a woman using Provera CI) may lose significant bone mineral density. Bone loss is Depo-Provera CI becomes pregnant or complains of severe abdominal greater with increasing duration of use and may not be completely pain. (5.4) reversible. (5.1) Anaphylaxis and Anaphylactoid Reactions: Provide emergency medical • It is unknown if use of Depo-Provera Contraceptive Injection during treatment. (5.5) adolescence or early adulthood, a critical period of bone accretion, Liver Function: Discontinue Depo-Provera CI if jaundice or will reduce peak bone mass and increase the risk for osteoporotic disturbances of liver function develop (5.6) Carbohydrate Metabolism: Monitor diabetic patients carefully. (5.11) fracture in later life. (5.1) • Depo-Provera Contraceptive Injection should not be used as a long- ----------------------------------ADVERSE REACTIONS--------------------------- term birth control method (i.e., longer than 2 years) unless other Most common adverse reactions (incidence >5%) are: menstrual irregularities birth control methods are considered inadequate. -

Black Box Warnings 2
First Quarter 2014 P&T Update Vol. XI, Issue 1 Formulary Addition/Deletion Special Points of 1. Argatroban - Argatroban is a selective and short-acting direct thrombin inhibitor FDA Interest: approved for the prophylaxis or treatment of thrombosis or venous thromboembolism in patients with heparin-induced thrombocytopenia (HIT), and of coronary artery • P&T Update-Formulary Addition/Deletion thrombosis during percutaneous coronary intervention in patients at risk of HIT. The formulary addition request was submitted by the Pharmacy Department with • Policy and Procedures/ endorsement from Cardiology and Hematology representatives. Floorstock Update Formulary addition – approved • Black Box Warnings 2. Argatroban dosing nomogram – approved • New Guidelines Released by 3. Dinoprostone 0.5mg gel (Prepidil®) – The Obstetrics, Gynecology, and Women’s Health Joint National Committee Department no longer use dinoprostone gel for cervical ripening. The request to (JNC) 8 for High Blood remove dinoprostone from the formulary was approved. Pressure Management in Formulary deletion – approved. Adults 4. Hydroxocobalamin (Cyanokit®) - Hydroxocobalamin is indicated for treating cyanide toxicity. The UH ED department recommended adding hydroxocobalamin to the formulary in place of Cyanide antidote kit. The committee voted to approve the formulary addition of hydroxocobalamin. A mini-FMEA on hydroxocobalamin was also submitted. Formulary addition – approved 5. Cyanide antidote kit (Sodium Nitrate + Amyl Nitrate + Sodium Thiosulfate) - Cyanide antidote kit has been manufacturer discontinued. The committee voted to delete this product from the formulary. Formulary deletion – approved 6. Pertuzumab (Perjeta®) – Pertuzumab is a monoclonal antibody approved by the FDA to use in combination with trastuzumab and docetaxel as first-line therapy for HER2- positive metastatic breast cancer. -

Zestril® (Lisinopril) Tablets Label
HIGHLIGHTS OF PRESCRIBING INFORMATION • Hypersensitivity (4) These highlights do not include all the information needed to use • Co-administration of aliskiren with Zestril in patients with diabetes (4, ZESTRIL safely and effectively. See full prescribing information for 7.4) ZESTRIL ----------------------- WARNINGS AND PRECAUTIONS --------------------- Zestril® (lisinopril) tablets, for oral use Initial U.S. Approval: 1988 • Angioedema: Discontinue Zestril, provide appropriate therapy and monitor until resolved (5.2) WARNING: FETAL TOXICITY • Renal impairment: Monitor renal function periodically (5.3) See full prescribing information for complete boxed warning. • Hypotension: Patients with other heart or renal diseases have increased • When pregnancy is detected, discontinue Zestril as soon as possible. risk, monitor blood pressure after initiation (5.4) (5.1) • Hyperkalemia: Monitor serum potassium periodically (5.5) • Drugs that act directly on the rennin-angiotensin system can cause • injury and death to the developing fetus. (5.1) Cholestatic jaundice and hepatic failure: Monitor for jaundice or signs of liver failure (5.6) ------------------------------ ADVERSE REACTIONS ---------------------------- --------------------------- INDICATIONS AND USAGE -------------------------- Common adverse reactions (events 2% greater than placebo) by use: Zestril is an angiotensin converting enzyme (ACE) inhibitor indicated for: • Hypertension: headache, dizziness and cough (6.1) • Treatment of hypertension in adults and pediatric patients 6 years of age • Heart Failure: hypotension and chest pain (6.1) and older (1.1) • Acute Myocardial Infarction: hypotension (6.1) • Adjunct therapy for heart failure (1.2) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca • Treatment of Acute Myocardial Infarction (1.3) Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION --------------------- www.fda.gov/medwatch. -

Customs Tariff - Schedule
CUSTOMS TARIFF - SCHEDULE 99 - i Chapter 99 SPECIAL CLASSIFICATION PROVISIONS - COMMERCIAL Notes. 1. The provisions of this Chapter are not subject to the rule of specificity in General Interpretative Rule 3 (a). 2. Goods which may be classified under the provisions of Chapter 99, if also eligible for classification under the provisions of Chapter 98, shall be classified in Chapter 98. 3. Goods may be classified under a tariff item in this Chapter and be entitled to the Most-Favoured-Nation Tariff or a preferential tariff rate of customs duty under this Chapter that applies to those goods according to the tariff treatment applicable to their country of origin only after classification under a tariff item in Chapters 1 to 97 has been determined and the conditions of any Chapter 99 provision and any applicable regulations or orders in relation thereto have been met. 4. The words and expressions used in this Chapter have the same meaning as in Chapters 1 to 97. Issued January 1, 2019 99 - 1 CUSTOMS TARIFF - SCHEDULE Tariff Unit of MFN Applicable SS Description of Goods Item Meas. Tariff Preferential Tariffs 9901.00.00 Articles and materials for use in the manufacture or repair of the Free CCCT, LDCT, GPT, UST, following to be employed in commercial fishing or the commercial MT, MUST, CIAT, CT, harvesting of marine plants: CRT, IT, NT, SLT, PT, COLT, JT, PAT, HNT, Artificial bait; KRT, CEUT, UAT, CPTPT: Free Carapace measures; Cordage, fishing lines (including marlines), rope and twine, of a circumference not exceeding 38 mm; Devices for keeping nets open; Fish hooks; Fishing nets and netting; Jiggers; Line floats; Lobster traps; Lures; Marker buoys of any material excluding wood; Net floats; Scallop drag nets; Spat collectors and collector holders; Swivels. -
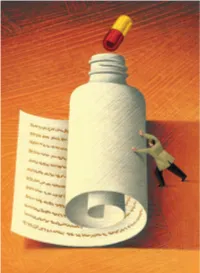
BLACK-BOX WARNINGS: How They Can Improve Your Clinical Practice a Better Understanding of These Warnings Leads to Safer, More Effective Prescribing
BLACK-BOX WARNINGS: How they can improve your clinical practice A better understanding of these warnings leads to safer, more effective prescribing Matthew A. Schreiber, MD, PhD ecently, the FDA issued “black-box” warnings, its most promi- Staff Psychiatrist 1 Puget Sound VA Health Care System nent drug safety statements, for esketamine, which is indicated Seattle, Washington for treatment-resistant depression, and the Z-drugs, which are Assistant Professor R 2 indicated for insomnia (Table 1, page 20). A black-box warning also Department of Psychiatry and Behavioral Sciences University of Washington School of Medicine comes with brexanolone, which was recently approved for postpar- Seattle, Washington tum depression.3 While these newly issued warnings serve as a timely Michelle Wiese, MD, MPH reminder of the importance of black-box warnings, older black-box PGY-3 Psychiatry Resident warnings also cover large areas of psychiatric prescribing, including all University of Washington School of Medicine Seattle, Washington medications indicated for treating psychosis or schizophrenia (increased mortality in patients with dementia), and all psychotropic medications Disclosures The authors report no financial relationships with any with a depression indication (suicidality in younger people). company whose products are mentioned in this article, or with In this article, we help busy prescribers navigate the landscape manufacturers of competing products. The views expressed are of black-box warnings by providing a concise review of how to use those of the authors and do not reflect the official policy of the Department of Veterans Affairs or the US Government. them in clinical practice, and where to find information to keep up-to-date. -

Alphabetical Listing of ATC Drugs & Codes
Alphabetical Listing of ATC drugs & codes. Introduction This file is an alphabetical listing of ATC codes as supplied to us in November 1999. It is supplied free as a service to those who care about good medicine use by mSupply support. To get an overview of the ATC system, use the “ATC categories.pdf” document also alvailable from www.msupply.org.nz Thanks to the WHO collaborating centre for Drug Statistics & Methodology, Norway, for supplying the raw data. I have intentionally supplied these files as PDFs so that they are not quite so easily manipulated and redistributed. I am told there is no copyright on the files, but it still seems polite to ask before using other people’s work, so please contact <[email protected]> for permission before asking us for text files. mSupply support also distributes mSupply software for inventory control, which has an inbuilt system for reporting on medicine usage using the ATC system You can download a full working version from www.msupply.org.nz Craig Drown, mSupply Support <[email protected]> April 2000 A (2-benzhydryloxyethyl)diethyl-methylammonium iodide A03AB16 0.3 g O 2-(4-chlorphenoxy)-ethanol D01AE06 4-dimethylaminophenol V03AB27 Abciximab B01AC13 25 mg P Absorbable gelatin sponge B02BC01 Acadesine C01EB13 Acamprosate V03AA03 2 g O Acarbose A10BF01 0.3 g O Acebutolol C07AB04 0.4 g O,P Acebutolol and thiazides C07BB04 Aceclidine S01EB08 Aceclidine, combinations S01EB58 Aceclofenac M01AB16 0.2 g O Acefylline piperazine R03DA09 Acemetacin M01AB11 Acenocoumarol B01AA07 5 mg O Acepromazine N05AA04 -

A Review on Antibiotic Resistance and Way of Combating Antimicrobial Resistance
A review on antibiotic resistance and way of combating antimicrobial resistance Shifa Begum1, Tofa Begum2, Naziza Rahman 3 and Ruhul A. Khan4, * 1Department of Genetic Engineering and Biotechnology, University of Chittagong, Chittagong, Bangladesh. 2Research Laboratories in Sciences Applied to Food, Canadian Irradiation Center, INRS-Institut Armand-Frappier, 531, Boulevard des Prairies, Laval, Quebec, Canada, H7V 1B7. 3Department of Microbiology, University of Dhaka, Bangladesh. 4Institute of Radiation and Polymer Technology, Atomic Energy Research Establishment, Savar, Dhaka, Bangladesh. GSC Biological and Pharmaceutical Sciences, 2021, 14(02), 087–097 Publication history: Received on 13 January 2021; revised on 07 February 2021; accepted on 09 February 2021 Article DOI: https://doi.org/10.30574/gscbps.2021.14.2.0037 Abstract Antibiotics are widely used most effective medication since the twentieth century against bacterial infections (Tetanus, Strep Throat, Urinary Tract Infections, etc.) and thus save one’s life. Before 20th-century infectious disease played the main role in the death. Thus, antibiotics opened a revolutionary era in the field of medication. These cannot fight against viral infections. Antibiotics are also known as an antibacterial that kill or slow down bacterial growth and prohibit the bacteria to harm. Resistance comes as a curse with antibiotics that occurs when bacteria change in some way that reduces or eliminates the effectiveness of drugs, chemicals or other agents designed to cure or prevent infections. It is now a significant threat to public health that is affecting humans worldwide outside the environment of the hospital. When a bacterium once become resistant to antibiotic then the bacterial infections cannot be cured with that antibiotic.