Comprehensive Cancer Centers ; a Relevant Model in France ?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Formations 3A 2012-2013 01/10/2012 E.N.G.E.E.S
E.N.G.E.E.S. - Formation d'ingénieurs Promotion 2010/2013 - HERAULT Formations 3A 2012/2013 au 11/09/2012 Nom-Prénom Filière Statut Formation 3A Césure 1 MAUGERI Antonin MP C césure 2 OLLAGNON Pauline MP C césure encadrée Masters cohabilités sigle 5 masters cohabilités - 6 spécialités (double diplôme) Master Sciences de la terre, de l'univers et de l'environnement – spécialité Ingénierie et ISiE Sciences pour l'Environnement Master Sciences pour l’Ingénieur - spécialité Mécanique Numérique en Ingénierie / MNI computational engineering Master Géographie Environnementale - spécialité Systèmes Géographiques et GE-SGE Environnement Master Génie Civil, Constructions et Ouvrages durables - spécalité Géotechnique, Eau, GC- COD/GER Nancy Risques GE-OTG Master Géographie Environnementale - spécialité Observation de la Terre et Géomatique Master Administration Economique et Sociale - spécialité Gestion et Droit des Energies et GDEDD Développement Durable Nom-Prénom Filière Statut Formation 3A 1 FREYDIER Perrine PSI C ISiE 2 POLLET Marion BCPST C ISiE 3 BELLAHCEN Salma MP C MNI 4 HOUBRON Roman BCPST C MNI 5 LE MOËL Romain MP C MNI 6 MOUTAHIR Amine IAV Maroc E MNI de BORTOLI 7 PC C GE-SGE Jean-Christophe GE-SGE 8 MOTTO Alexandre BCPST C GC COD/GER 9 ABBASSI SABER Anas IAV Maroc E option Géotechnique Autres masters recherche - pro - à l'étranger sigle formation Institut universitaire Master Science de la mer et du littoral - mention Expertise et gestion du Littoral (EGEL) de la mer - Brest double diplôme Master Recherche Réseau Sciences du Territoire - spécialité Systèmes territoriaux, aide à Univ J. Fourier - Grenoble la décision, environnement (STADE) double diplôme EHESP Rennes Master of Public Health MPH double diplôme Univ Sorbonne Master Sciences de la Terre et de l'Environnement - spécialité Eau, climat, environnement Univ J. -
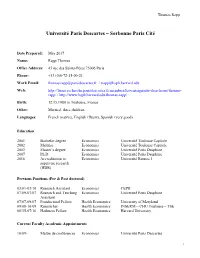
Cv Thomas Rapp
Thomas Rapp Université Paris Descartes – Sorbonne Paris Cité Date Prepared: May 2017 Name: Rapp Thomas Office Address: 45 rue des Saints-Pères 75006 Paris Phone: +33 (0)6-72-15-00-21 Work Email: [email protected] / [email protected] Web: http://liraes.recherche.parisdescartes.fr/membres/les-enseignants-chercheurs/thomas- rapp/ / http://www.hsph.harvard.edu/thomas-rapp/ Birth: 12.15.1980 in Toulouse, France Other: Married, three children Languages: French (native), English (fluent), Spanish (very good) Education 2001 Bachelor degree Economics Université Toulouse Capitole 2002 Maîtrise Economics Université Toulouse Capitole 2003 Master’s degree Economics Université Paris Dauphine 2007 Ph.D. Economics Université Paris Dauphine 2016 Accreditation to Economics Université Rennes 1 supervise research (HDR) Previous Positions (Pre & Post doctoral) 03/01-03/10 Research Assistant Economics CEPII 07/09-07/07 Research and Teaching Economics Université Paris Dauphine Assistant 07/07-09/07 Postdoctoral Fellow Health Economics University of Maryland 09/08-10/09 Researcher Health Economics INSERM – CHU Toulouse – TSE 08/15-07/16 Harkness Fellow Health Economics Harvard University Current Faculty Academic Appointments 10/09- Maître de conférences Economics Université Paris Descartes 1 Thomas Rapp Invited research stays 07/15-08/16 Research fellow (12 months), Harvard University (USA) 04/17 Visiting Scholar (2 weeks), Columbia University (USA) 05/17 Visiting Professor (2 weeks), Catholic University of Rome (Italy) Editorial Activities -

Curriculum Vitae
Youssef Oulhote, MEng, PhD Assistant Professor of Epidemiology Department of Biostatistics and Public Health, SPHHS University of Massachusetts Amherst 715, N Pleasant Street, Arnold House Room 432 Amherst, MA 01003 Tel No: +1.413.545.0845 / E-mail: [email protected] EDUCATION 2012 PhD Epidemiology / Public Health Lorraine University/EHESP, Rennes, France 2008 MSc Bio-contaminants risk assessment AgroParisTech, Paris, France 2006 State Engineer Food & Agricultural technologies Agronomic & Veterinary Institute, Morocco RESEARCH & PROFESSIONAL EXPERIENCE Department of Biostatistics and Epidemiology, School of Public Health 09/2018 - Assistant Professor and Health Sciences, UMASS - Amherst Environmental and Occupational Medicine & Epidemiology Program, 02/2015 - Research Scientist Harvard T.H. Chan School of Public Health, Boston. 09/2014 - Adjunct Epidemiologist Department of Psychiatry, McGill University, Montreal, Quebec, Canada Department of Environmental and Occupational Health, 06/2012 - 09/2014 Postdoctoral Fellow Université de Montréal, Canada. Exposure, Epidemiology & Risk program, Harvard T.H. Chan School of 2011 Visiting Fellow Public Health, Boston. 2008 – 2012 Doctoral Fellow EHESP - French National School of Public Health, Rennes. Joint team bioMérieux-CEA (Atomic Energy Commission), Grenoble, 2008 Research trainee France. 2007 Food Safety Manager Morocco Gum Industry, Sidi Slimane, Morocco 2005 – 2006 Research engineer Olive oil research center - Agropole, Meknes, Morocco. HONORS & AWARDS 2019 Outstanding Abstract award, International -

Top Universities by Google Scholar Citations
SEARCH HOME NORTH AMERICA LATIN AMERICA EUROPE ASIA AFRICA ARAB WORLD OCEANIA RANKING BY AREAS Consejo Superior de Investigaciones Cientificas ‹ › Home » TRANSPARENT RANKING: Top Universities by Google... Current edition TRANSPARENT RANKING: Top Universities by Google January 2017 Edition: 2017.1.1 (final) Scholar Citations Fourth Edition (July 2017 version 4.01 beta!) About Us Last year we used the institutional profiles introduced by Google Scholar Citations for providing a ranking of universities according About Us to the information provided for the groups of scholars sharing the same standardized name and email address of an institution. The total Contact Us open in browser PRO version Are you a developer? Try out the HTML to PDF API pdfcrowd.com Contact Us number of individual profiles in GSC is probably close to one million, while the number of these universities profiles is over 5000. Google Scholar is working for extending the world coverage of the institutional profiles to (almost) all the academic organizations. Unfortunately About the Ranking their resources are limited and there is no final date for finishing the task. We are still committed to the use of this key source, so we decided to collect the same data (citations) in the same fashion (top 10 excluding the most cited) for the lists obtained from filtering GSC Methodology profiles by the institutional web domains used in the Ranking Web. Objectives FAQs This ranking is an experiment for testing the suitability of including GSC data in the Rankings Web, but it is still in beta. The current Notes methodology is simple: Previous editions 1. -

CV Jonathan Sicsic
Jonathan SICSIC Paris Institute of Technology, 143 Avenue de Versailles, Bureau B511, 75016 Paris LIRAES, Centre Universitaire des Saints-Pères, 45 rue des Saint-Pères, 75006 Paris [email protected] August 2020 Personal information Date of birth: October 3, 1988 Citizenship: French Research expertise: Applied econometrics, Health economics & policy evaluation, Non-market valuation BIOGRAPHY Current positions Assistant professor, Paris Institute of Technology (IUT) Sept. 2019- Researcher in the applied health economics research unit (LIRAES, EA4470) Past professional experiences Postdoctoral researcher, LIRAES, Paris Descartes University, Paris, France 2017-2019 Visiting fellow, Health Economics Research Unit, University of Aberdeen, Scotland 2017 (Jan-Jui) Postdoctoral researcher, University of Lyon 1 & Centre Léon Bérard, Lyon 2015-2017 Research engineer, CESP Inserm U1018, University Paris-Sud, Villejuif 2015 (Jan-Aug) Research assistant, Cermes3, UMR 8211 (CNRS, Inserm, EHESS), Villejuif, France 2011-2014 Education Ph.D in Economics, Paris-Dauphine University 2011-2014 Dissertation topic: “Impact of economic incentives in general practice” Supervisor: C. FRANC (researcher, Inserm) Jury: B. DORMONT, K. JANUS, L. LETRILLIART, N. MOUMJID, C. PEYRON Special training to access data from the French National Health Data System (SNDS) 2013 M.Sc in Statistics and Econometrics, ENSAI (Ecole Nationale de la Statistique, 2008-2011 et de l’Analyse de l’Information), Rennes B.A in Literature and Social Sciences (B/L), Marseille 2006-2008 RESEARCH GRANTS AND AWARDS Main investigator (PI or co-holder) - Université de Paris / King’s College London Joint Research Award 2020-2021 “The impact of Long-Term Care policies on frailty risk for older people in Europe and the UK“ (joint with T. -

Strater Diagnostic Territorial
STRATER Aix-Marseille Provence Méditerranée Juin 2018 Note liminaire L’objectif des diagnostics territoriaux « Strater » est de proposer, sous l’angle d’une vision globale des sites, un état des lieux de l’enseignement supérieur, de la recherche et de l’innovation par une présentation des grands chiffres, des tendances, et de la structuration des acteurs. Ces documents apportent des éléments de diagnostic sur lesquels les acteurs concernés, à différents niveaux, peuvent appuyer leurs choix stratégiques en matière d’enseignement supérieur, de recherche et d’innovation. Ils font, préalablement à leur publication, l’objet d’échanges avec les établissements d’enseignement supérieur et de recherche concernés. Les territoires considérés Le diagnostic territorial a été construit à l’échelle académique ou inter-académique, selon l’organisation territoriale choisie par le regroupement, conformément aux dispositions de la loi relative à l’enseignement supérieur et à la recherche du 22 juillet 2013. En conséquence, les données présentées portent sur le périmètre académique (ou-inter-académique) dans lequel s’inscrit le regroupement. Lorsqu’elles ne sont pas disponibles à cette échelle, le périmètre retenu peut être celui de l’établissement en charge de la coordination territoriale. Pour l’Île-de-France, ont été pris en compte les établissements membres des communautés d’universités et d’établissements (COMUE) et leurs partenaires associés en fonction des données recueillies. 26 sites de regroupement ont été analysés correspondant aux territoires de 7 associations et de 19 COMUE constituées. Le diagnostic relatif à la Corse a également été mis à jour ainsi que ceux concernant les territoires d’Outre-mer (StraTOM). -

Nolwenn Le Meur
Nolwenn Le Meur EHESP Avenue du Professeur L´eonBernard CS 74312 35043 Rennes Cedex France Tel: +33 (0) 2 99 02 25 14 [email protected] Research EHESP Rennes, FR Associate professor in Biostatistics November 2010 { present Deciphering patients' care trajectory using graph theory and data mining INSERM-IRISA-Biogenouest Rennes, FR Post-Doctoral Research Associate March 2008 { October 2010 Coordinator of the Biogenouest Integrative Genomics Project. Dynamic modeling of TGF-beta signaling pathways in the control of cell proliferation. Dr N. Th´eret,IRSET EA 4427 SeRAIC. Fred Hutchinson Cancer Center Research Seattle, USA Post-Doctoral Research Associate Jul. 2005{Fev. 2008 The role of multiprotein complexes in determining phenotype in Yeast. Quality assessment of flow cytometry data. Dr R. Gentleman, Computational Biology Group, Public Health Department. Education 2001-2005 Ph.D. in Bioinformatics, INSERM U533, Supervisor Jean L´eger,University of Nantes, France. 2000-2001 Master in Genomics and Bioinformatics, University of Rennes I, France. 1997-2000 Engineering School of Microbiology and Food Safety, Brest, France. 1996-1997 Biology Diploma, University of Brest, France. Expertise Reviewer for • Bioinformatics, BMC bioinformatics, Plos Computational Biology • BMC genomics, Cytometry A • Young Researchers ANR (2012) Main publications N. Le Meur. Computational methods for evaluation of cell-based data assessment-Bioconductor. Curr Opin Biotechnol. 2012 Oct 9. doi: 10.1016/j.copbio.2012.09.003. N. Le Meur et al. R and Bioconductor packages in Bioinformatics: toward systems biology. In Statistical Bioinformatics: A Guide for Life and Biomedical Science researchers. John Wiley & Sons (2010). N. LeMeur* , F. Hahne* et al. flowCore: a Bioconductor package for high throughput flow cytometry. -

Th European Meeting of EHESP School of Public Health November
th European COPENHAGEN 4meeting of November 9, 2011 EHESP School MANAGEMENT IN PUBLIC HEALTH of Public Health AND HEALTHCARE ORGANIZATIONS From theory to practice Management in health is in crisis: budget cuts, in health. You will also have the opportunity to human resources shortages, globalization, aging network with scholars, professionals and policy population and new technology are only a few is- makers. sues faced by healthcare organizations and public This one day meeting will take place in Copenha- health policy makers. It is in dire needs of new so- gen on the 9th of November 2011 from 8:30 am to lutions, methods, and strategies. We need to shift 5 pm. The event will be held in English and as a the many theories into effective and efficient prac- pre-conference to the 4th European Health Confe- tices. rence. The EHESP School of Advanced Studies in Public Health is organizing a conference on present and Registration: future issues, methods and strategies in Manage- ment in the field of Public Health. http://www.eupha.org This conference offers the opportunity to listen to http://www.eupha.org/cgi-files/mem_db.cgi?action=startreg internationally renowned speakers and presen- ters and debate crucial problems in management Costs: 150 euros For more information: [email protected] Bruno COTARD +33 (0)2 99 02 28 81 Venue : The Bella Centre, Center Boulevard 5 - Copenhagen Ecole des hautes études en santé publique Avenue du Professeur-Léon-Bernard CS 74312 - 35043 Rennes cedex - France Tél. : +33 (0)2 99 02 22 00 www.ehesp.fr -

List of Participants & Exhibition Staff
LIST OF PARTICIPANTS & EXHIBITION STAFF This list is based on registrations received by 07 September 2019. Participants indicating they did not wish their data to be made available have not been included. Albania Albania Ms Barbara LUNG Australia Director, International Bedër University Academic Assembly, Inc Mrs Ilda SHYTAJ Mr Paul NICHOLLS Dr Gretchen DOBSON Lecturer Director, Research Partnerships President, Global Alumni Relations Mrs Hannah WILKINSON Andorra AIM Overseas Director, Student Engagement EDUopinions Ms Marine HAUTEMONT Mr Nikos FILIPPAKIS CEO Deakin University Chief Operating Officer Mrs Martine LANGDON APAIE (Asia-Pacific Association Regional Marketing Manager Europe University of Andorra for International Education) Ms Ursula LORENTZEN Mr John ZVEREFF Ms Louise KINNAIRD Director, Deakin Europe President's Delegate for Internationalisation Director Mr John MOLONY Argentina Australian Catholic University Pro Vice-Chancellor (International) CRUP - Consejo de Rectores de Mr Kirk DOYLE Associate Director, International Relations Ms Anika SCHNEIDER Universidades Privadas Acting Manager Global Student Mobility Mrs Andrea HASSEN Australian National University Lic. Relaciones Internacionales Prof Dr Wei SHEN Ms Kristina TAN Associate Pro Vice-Chancellor (International Relations) Fundacion UADE Global Programs, Outbound Exchange Dr Ly TRAN Ms Paula IGLESIAS Australian Trade Commission Coordinator Associate Professor Ms Henriette POOK ITBA - Instituto Tecnológico de Senior Education Manager Education Queensland Buenos Aires Ms -

Document Choose France File Pdf 2.33 MB
CHOOSE FRANCE UNITED KINGDOM THE NETHERLANDS BELGIUM FRANCE SWITZERLAND France is PORTUGAL the world’s fourth-largest SPAIN destination for international students and the leading non-English- speaking destination 2 CHOOSE FRANCE p.4 Introduction p.8 Degrees p.10 Vocational education: national diplomas at the L2 and L3 levels p.12 Doctoral programs p.14 Universities p.16 The Grandes Écoles and Écoles supérieures • programs in engineering • programs in GERMANY business and management p.18 Schools of art p.20 Schools of architecture, specialized schools STUDYINGIN FRANCE p.22 Introduction p.24 Choosing a program p.26 Enrolling in a French institution p.28 Grants and financial aid p.30 Applying for a visa ITA LY LIVING IN FRANCE p.32 Introduction GREECE p.34 Housing p.36 Work, Insurance p.38 Cultural life p.40 Clubs ans special-interest groups p.41 France Alumni p.42 Prices p.44 About Campus France p.46 ON THE WEB 3 Choose France WELCOME TO FRANCE French institutions of higher education are firmly committed to internationalization. By building a period of work or study abroad into academic programs, offering programs in English, devising joint degrees, participating in mobility programs (such as Erasmus+), obtaining various forms of international recognition, and setting up branch campuses abroad, they offer their students, French and international alike, numerous opportunities to widen the international aspect of their program of study. 4 Choose France CHOOSE FRANCE France is the destination for more than 323,933 international students making up 12% of total postsecondary enrollments. ADVANCED RESEARCH France benefits from a long, proud tradition of scientific and technological research and innovation that underpins the nation’s achie- vements in fields such as aeronautics and space, transportation, electronics, telecom- munications, chemistry, biotechnologies, health, and mathematics. -
[Infographie] Qu'évalue Le Hcéres En 2017-2018
Qu'évalue le Hcéres en 2017 - 2018 ? Liste prévisionnelle des évaluations pour la vague D Évaluations institutionnelles Établissements d'enseignement supérieur et de recherche publics et privés (sous contrat avec l'État) 41 dont 4 COMUE Institut de Physique du Globe de Paris (IPGP) A Arts et Métiers ParisTech (ENSAM) Institut Mines Telecom Institut national des langues et civilisations orientales (INALCO) C Centre de Formation des Journalistes (CFJ), Institut national d'histoire de l'art (INHA) Chimie ParisTech Institut Protestant de théologie Collège de France Conservatoire national des arts et métiers (CNAM) M Mines ParisTech Muséum national d'Histoire naturelle (MNHN) E École des hautes études en santé publique (EHESP) École des hautes études en sciences sociales O Observatoire de Paris (EHESS) École nationale des chartes École Nationale Supérieure d'Architecture Paris La Villette (ENSA) École nationale supérieure d'architecture P Paris Sciences et Lettres (PSL - Comue) Paris Val de Seine (ENSA) École normale supérieure (ENS Ulm) École Pratique des Hautes Études (EPHE) École Spéciale d'Architecture de Paris (ESA), S SciencesPo (IEP Paris) École supérieure de physique et de chimie Sorbonne Universités (Comue) industrielles de la ville de Paris (ESPCI Paris) F Faculté libre de philosophie comparée (IPC) Université Paris 1 Panthéon-Sorbonne Fondation Maison des sciences de U Université Paris 13 l'homme (FMSH Paris) Université Paris Descartes H Université Paris Diderot HeSam Université (Comue) Université Paris II Panthéon-Assas Université -

Février 2009 PROJET « UNIVERSITE PARIS CITE »
Paris, Ville Universitaire OPERATION CAMPUS Février 2009 PROJET « UNIVERSITE PARIS CITE » 1 2 3 S O M M A I R E PRES UNIVERSITE PARIS CITE Signatures des déposants 2 Sommaire 5 Les territoires Campus parisiens 7 Sites et disciplines du Campus 9 I. Introduction 11 I.1 Pourquoi un PRES 11 I.2 Quelle stratégie d’ensemble ? 12 I.3. Quels projets communs ? 13 II. Présentation du projet 15 II.1. Les partenaires 15 II.2. Les territoires Campus 22 II.3. La gouvernance : Projets de statuts du PRES 27 III. Les projets pédagogiques et scientifiques du PRES 33 III.1. Biologie – Médecine 33 III.2. Santé et société 36 III.3 Le Centre de Santé Publique de l’Hôtel Dieu de Paris 38 III.4 Langues et civilisations 39 III.5. La formation technologique 39 III.6 Autres projets de formations communes 40 IV. Les projets transversaux coopératifs 47 IV.1. Développement de stratégies communes de valorisation du PRES 47 IV.2. Politique et promotion internationale du PRES 48 IV.3. Mutualisation des fonctions supports 50 IV.4. Valorisation du patrimoine immobilier 51 IV.5. Systèmes d’information et TICE 52 IV.6. Bibliothèques – PRES – Université Paris Cité 54 V. Vie et Santé étudiante 55 V.I. Logements et installations sportives 55 V.2. La santé étudiante 55 VI. Conclusion 57 VII. Annexes 59 VII.I. Projets vie étudiante (Paris Ville Universitaire) 59 VII.2. Projets propres au PRES 65 VII.3 Récapitulatif des projets immobiliers propres au PRES 67 VII.4. Récapitulatif des projets immobiliers communes Paris Ville Universitaire, opérations 69 d’intérêt pour le PRES « Université Paris Cité ».