Blue Cross and Blue Shield October 2019 Multi-Tier Basic Drug List I How to Use This List Generic Drugs Are Shown in Lower-Case Boldface Type
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endothelin System and Therapeutic Application of Endothelin Receptor
xperim ACCESS Freely available online & E en OPEN l ta a l ic P in h l a C r m f o a c l a o n l o r g u y o J Journal of ISSN: 2161-1459 Clinical & Experimental Pharmacology Research Article Endothelin System and Therapeutic Application of Endothelin Receptor Antagonists Abebe Basazn Mekuria, Zemene Demelash Kifle*, Mohammedbrhan Abdelwuhab Department of Pharmacology, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia ABSTRACT Endothelin is a 21 amino acid molecule endogenous potent vasoconstrictor peptide. Endothelin is synthesized in vascular endothelial and smooth muscle cells, as well as in neural, renal, pulmonic, and inflammatory cells. It acts through a seven transmembrane endothelin receptor A (ETA) and endothelin receptor B (ETB) receptors belongs to G protein-coupled rhodopsin-type receptor superfamily. This peptide involved in pathogenesis of cardiovascular disorder like (heart failure, arterial hypertension, myocardial infraction and atherosclerosis), renal failure, pulmonary arterial hypertension and it also involved in pathogenesis of cancer. Potentially endothelin receptor antagonist helps the treatment of the above disorder. Currently, there are a lot of trails both per-clinical and clinical on endothelin antagonist for various cardiovascular, pulmonary and cancer disorder. Some are approved by FAD for the treatment. These agents are including both selective and non-selective endothelin receptor antagonist (ETA/B). Currently, Bosentan, Ambrisentan, and Macitentan approved -

2020 Prior Authorization Criteria
2020 PRIOR AUTHORIZATION CRITERIA TABLE OF CONTENTS abiraterone tablet ...................................................................................................................... 217 ABRAXANE .............................................................................................................................. 131 ACTIMMUNE .............................................................................................................................. 14 ADASUVE ................................................................................................................................... 27 ADEMPAS ................................................................................................................................ 197 AFINITOR ................................................................................................................................. 217 AFINITOR DISPERZ ................................................................................................................. 217 AIMOVIG ..................................................................................................................................... 15 ALECENSA ............................................................................................................................... 217 ALIMTA ..................................................................................................................................... 131 ALIQOPA ................................................................................................................................. -

Insulin Aspart Sanofi, If It Is Coloured Or It Has Solid Pieces in It
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 for how to report adverse reactions. 1. NAME OF THE MEDICINAL PRODUCT Insulin aspart Sanofi 100 units/ml solution for injection in vial Insulin aspart Sanofi 100 units/ml solution for injection in cartridge Insulin aspart Sanofi 100 units/ml solution for injection in pre-filled pen 2. QUALITATIVE AND QUANTITATIVE COMPOSITION One ml solution contains 100 units insulin aspart* (equivalent to 3.5 mg). Insulin aspart Sanofi 100 units/ml solution for injection in vial Each vial contains 10 ml equivalent to 1,000 units insulin aspart. Insulin aspart Sanofi 100 units/ml solution for injection in cartridge Each cartridge contains 3 ml equivalent to 300 units insulin aspart. Insulin aspart Sanofi 100 units/ml solution for injection in pre-filled pen Each pre-filled pen contains 3 ml equivalent to 300 units insulin aspart. Each pre-filled pen delivers 1-80 units in steps of 1 unit. *produced in Escherichia coli by recombinant DNA technology. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection (injection). Clear, colourless, aqueous solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Insulin aspart Sanofi is indicated for the treatment of diabetes mellitus in adults, adolescents and children aged 1 year and above. 4.2 Posology and method of administration Posology The potency of insulin analogues, including insulin aspart, is expressed in units, whereas the potency of human insulin is expressed in international units. -

List of Approved Ndas for Biological Products That Were Deemed to Be Blas on March 23, 2020
List of Approved NDAs for Biological Products That Were Deemed to be BLAs on March 23, 2020 On March 23, 2020, an approved application for a biological product under section 505 of the Federal Food, Drug, and Cosmetic Act (FD&C Act) was deemed to be a license for the biological product under section 351 of the Public Health Service Act (PHS Act) (see section 7002(e)(4)(A) of the Biologics Price Competition and Innovation Act of 2009). To enhance transparency and facilitate planning for the March 23, 2020, transition date, FDA compiled a preliminary list of approved applications for biological products under the FD&C Act that were listed in FDA’s Approved Drug Products with Therapeutic Equivalence Evaluations (the Orange Book) and that would be affected by this transition provision. FDA posted this list on the FDA website in December 2018, and periodically updated this list before the March 23, 2020, transition date. The September 2019 update to this preliminary list added certain administratively closed applications related to approved applications for biological products that were on the December 2018 version of this list. The January 2020 update to the preliminary list reflected a change to the definition of “biological product” made by the Further Consolidated Appropriations Act, 2020, which was enacted on December 20, 2019. Section 605 of this Act further amended the definition of a “biological product” in section 351(i) of the PHS Act to remove the parenthetical “(except any chemically synthesized polypeptide)” from the statutory category of “protein.” FDA has provided below a list of each approved application for a biological product under the FD&C Act that was deemed to be a license (i.e., an approved biologics license application (BLA)) for the biological product on March 23, 2020. -

DRUGS REQUIRING PRIOR AUTHORIZATION in the MEDICAL BENEFIT Page 1
Effective Date: 08/01/2021 DRUGS REQUIRING PRIOR AUTHORIZATION IN THE MEDICAL BENEFIT Page 1 Therapeutic Category Drug Class Trade Name Generic Name HCPCS Procedure Code HCPCS Procedure Code Description Anti-infectives Antiretrovirals, HIV CABENUVA cabotegravir-rilpivirine C9077 Injection, cabotegravir and rilpivirine, 2mg/3mg Antithrombotic Agents von Willebrand Factor-Directed Antibody CABLIVI caplacizumab-yhdp C9047 Injection, caplacizumab-yhdp, 1 mg Cardiology Antilipemic EVKEEZA evinacumab-dgnb C9079 Injection, evinacumab-dgnb, 5 mg Cardiology Hemostatic Agent BERINERT c1 esterase J0597 Injection, C1 esterase inhibitor (human), Berinert, 10 units Cardiology Hemostatic Agent CINRYZE c1 esterase J0598 Injection, C1 esterase inhibitor (human), Cinryze, 10 units Cardiology Hemostatic Agent FIRAZYR icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent HAEGARDA c1 esterase J0599 Injection, C1 esterase inhibitor (human), (Haegarda), 10 units Cardiology Hemostatic Agent ICATIBANT (generic) icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent KALBITOR ecallantide J1290 Injection, ecallantide, 1 mg Cardiology Hemostatic Agent RUCONEST c1 esterase J0596 Injection, C1 esterase inhibitor (recombinant), Ruconest, 10 units Injection, lanadelumab-flyo, 1 mg (code may be used for Medicare when drug administered under Cardiology Hemostatic Agent TAKHZYRO lanadelumab-flyo J0593 direct supervision of a physician, not for use when drug is self-administered) Cardiology Pulmonary Arterial Hypertension EPOPROSTENOL (generic) -

Pharmacokinetics, Pharmacodynamics and Drug
pharmaceutics Review Pharmacokinetics, Pharmacodynamics and Drug–Drug Interactions of New Anti-Migraine Drugs—Lasmiditan, Gepants, and Calcitonin-Gene-Related Peptide (CGRP) Receptor Monoclonal Antibodies Danuta Szkutnik-Fiedler Department of Clinical Pharmacy and Biopharmacy, Pozna´nUniversity of Medical Sciences, Sw.´ Marii Magdaleny 14 St., 61-861 Pozna´n,Poland; [email protected] Received: 28 October 2020; Accepted: 30 November 2020; Published: 3 December 2020 Abstract: In the last few years, there have been significant advances in migraine management and prevention. Lasmiditan, ubrogepant, rimegepant and monoclonal antibodies (erenumab, fremanezumab, galcanezumab, and eptinezumab) are new drugs that were launched on the US pharmaceutical market; some of them also in Europe. This publication reviews the available worldwide references on the safety of these anti-migraine drugs with a focus on the possible drug–drug (DDI) or drug–food interactions. As is known, bioavailability of a drug and, hence, its pharmacological efficacy depend on its pharmacokinetics and pharmacodynamics, which may be altered by drug interactions. This paper discusses the interactions of gepants and lasmiditan with, i.a., serotonergic drugs, CYP3A4 inhibitors, and inducers or breast cancer resistant protein (BCRP) and P-glycoprotein (P-gp) inhibitors. In the case of monoclonal antibodies, the issue of pharmacodynamic interactions related to the modulation of the immune system functions was addressed. It also focuses on the effect of monoclonal antibodies on expression of class Fc gamma receptors (FcγR). Keywords: migraine; lasmiditan; gepants; monoclonal antibodies; drug–drug interactions 1. Introduction Migraine is a chronic neurological disorder characterized by a repetitive, usually unilateral, pulsating headache with attacks typically lasting from 4 to 72 h. -

A Critical Appraisal of the Role of Insulin Analogues in the Management of Diabetes Mellitus Ralph Oiknine, Marla Bernbaum and Arshag D
Drugs 2005; 65 (3): 325-340 REVIEW ARTICLE 0012-6667/05/0003-0325/$39.95/0 2005 Adis Data Information BV. All rights reserved. A Critical Appraisal of the Role of Insulin Analogues in the Management of Diabetes Mellitus Ralph Oiknine, Marla Bernbaum and Arshag D. Mooradian Division of Endocrinology, Department of Internal Medicine, Diabetes, and Metabolism, St Louis University School of Medicine, St Louis, Missouri, USA Contents Abstract ....................................................................................325 1. Physiology of Insulin Secretion .............................................................326 2. Conventional Insulin Preparations ..........................................................327 3. Insulin Analogues ........................................................................328 3.1 Rapid-Acting Insulin Analogues .......................................................328 3.1.1 Insulin Lispro ...................................................................328 3.1.2 Insulin Aspart ..................................................................329 3.1.3 Insulin Glulisine .................................................................329 3.1.4 Clinical Utility of Rapid-Acting Insulin Analogues ...................................330 3.2 Premixed Insulins and Insulin Analogues ................................................331 3.3 Basal Insulin Analogues ...............................................................331 3.3.1 Insulin Glargine ................................................................331 -

Onglyza (Saxagliptin) Uses, Dosage, Side Effects - Drugs.Com 04/07/2015 Insulin Pump – Tubeless Feel the Freedom for Yourself! Learn About the Omnipod®
Onglyza (saxagliptin) Uses, Dosage, Side Effects - Drugs.com 04/07/2015 Insulin Pump – Tubeless Feel The Freedom For Yourself! Learn About The OmniPod®. Browse all medications A B C D E F G H I J K L M N O P Q R S T U V W X Y Z Advanced Search Phonetic Search Drugs A-Z Pill Identifier Interactions Checker News Health Professionals Q & A Mednotes Apps Home → Conditions → Diabetes, Type 2 → Onglyza Print Share Sign In or Register Onglyza Related Information Availability Pregnancy Category Generic Name: saxagliptin (SAX a GLIP tin) Prescription only No proven risk in Brand Names: Onglyza humans CSA Schedule Not a controlled drug Approval History Drug history at FDA Overview Side Effects Dosage Interactions For Professionals More Reviews Average User Rating Insulin Pump – Tubeless Feel The Freedom For Yourself! Learn About The 9 User Reviews 7.6 Rate it! OmniPod® Drug Class What is Onglyza? Dipeptidyl peptidase 4 inhibitors Onglyza (saxagliptin) is an oral diabetes medicine that helps control blood sugar levels . It works by regulating Related Drugs the levels of insulin your body produces after Diabetes, Type 2 eating. metformin Onglyza is for people with type 2 diabetes. It is insulin aspart Januvia sometimes used in combination with other glipizide diabetes medications, but is not for treating glimepiride type 1 diabetes . Lantus Onglyza may also be used for purposes not Invokana listed in this medication guide. Victoza glyburide Levemir Humalog Actos Important information Janumet You should not use Onglyza if you are in a state of diabetic ketoacidosis (call your doctor for Glucophage treatment with insulin). -

Komboglyze, INN-Saxagliptin, Metformin
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT Komboglyze 2.5 mg/850 mg film-coated tablets Komboglyze 2.5 mg/1,000 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Komboglyze 2.5 mg/850 mg film-coated tablets Each tablet contains 2.5 mg of saxagliptin (as hydrochloride) and 850 mg of metformin hydrochloride. Komboglyze 2.5 mg/1,000 mg film-coated tablets Each tablet contains 2.5 mg of saxagliptin (as hydrochloride) and 1,000 mg of metformin hydrochloride. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet (tablet). Komboglyze 2.5 mg/850 mg film-coated tablets Light brown to brown, biconvex, round, film-coated tablets, with “2.5/850” printed on one side and “4246” printed on the other side, in blue ink. Komboglyze 2.5 mg/1,000 mg film-coated tablets Pale yellow to light yellow, biconvex, oval shaped, film-coated tablets, with “2.5/1000” printed on one side and “4247” printed on the other side, in blue ink. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Komboglyze is indicated in adults with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: in patients inadequately controlled on their maximally tolerated dose of metformin alone in combination with other medicinal products for the treatment of diabetes, including insulin, in patients inadequately controlled with metformin and these medicinal products (see sections 4.4, 4.5 and 5.1 for available data on different combinations) in patients already being treated with the combination of saxagliptin and metformin as separate tablets. -

Endothelin-Receptor Antagonists Are Proapoptotic and Antiproliferative in Human Colon Cancer Cells
British Journal of Cancer (2003) 88, 788 – 795 & 2003 Cancer Research UK All rights reserved 0007 – 0920/03 $25.00 www.bjcancer.com Endothelin-receptor antagonists are proapoptotic and antiproliferative in human colon cancer cells 1 1 ,1 L Peduto Eberl , R Bovey and L Juillerat-Jeanneret* 1 University Institute of Pathology, CHUV, University of Lausanne, Bugnon 25, CH1011 Lausanne, Switzerland Endothelin (ET)-1 can act as an autocrine/paracrine growth factor or an antiapoptotic factor in human cancers. To study the role of ET-1 in human colon cancer, proliferation and apoptosis of colon carcinoma cells was investigated using human HT-29 and SW480 colon carcinoma cells. ET-1 was secreted by these cells. Treatment of cells with bosentan, a dual ETA/B-receptor antagonist, decreased cell number. Inhibition of DNA synthesis by bosentan was observed only in the presence of serum. Exogenously added ET-1 did not increase DNA synthesis in serum-deprived cells. SW480 cells were sensitive and HT-29 cells were resistant to FasL- induced apoptosis. Bosentan sensitised resistant HT-29 cells to FasL-induced, caspase-mediated apoptosis, but not to TNF-a-induced apoptosis. Bosentan and/or FasLigand (FasL) did not modulate the expression of caspase-8 or FLIP. Bosentan sensitisation to À13 À10 À9 À7 apoptosis was reversed by low concentrations (10 –10 M), but not by high concentrations (10 –10 M) of ET-1. These results suggest that the binding of ET-1 to high-affinity sites inhibits FasL-induced apoptosis, while the binding of either ET-1 or receptor antagonists to low-affinity sites promotes FasL-induced apoptosis. -

New Drug Update: Not All That Glitters Is Gold Idaho Society of Health‐System Pharmacists 2018 Fall Meeting Sun Valley, Idaho September 30, 2018
9/23/2018 New Drug Update: Not All That Glitters is Gold Idaho Society of Health‐System Pharmacists 2018 Fall Meeting Sun Valley, Idaho September 30, 2018 PRESENTERS: Boise VA Medical Center Idaho State University PGY2 Ambulatory Care Residents: PGY2 Pharmacotherapy Resident: Audra Wilson, PharmD; Kat Liu, PharmD; Kailee Morton, PharmD Nitz Bankova, PharmD St. Luke’s Health System Infectious Disease Pharmacy Fellow: PGY2 Oncology Pharmacy Residents: Benjamin Pontefract, PharmD Andrew Li, PharmD; Amanda Wright, PharmD; Bryce Benson, PharmD PGY2 Mental Health Pharmacy Resident: Samantha Patton, PharmD Disclosures No conflicts of interest to disclose Learning Objectives • Describe clinical scenarios where newly approved medications are beneficial. • Compare newly approved medications with current standards of care. • Identify investigational new drugs and their potential clinical applications. 1 9/23/2018 Overview of Topics • Infectious Disease • Ambulatory Care • Diabetes Mellitus • Women’s Health • Anticoagulation • Pain Management • Oncology • Acute Myeloid Leukemia (AML) Infectious Disease: Plazomicin Delafloxacin Benjamin Pontefract, PharmD Plazomicin (Zemdri®):Overview • Systemic antibiotic in the aminoglycoside family • MoA: disrupts the 30s ribosome to prevent protein synthesis • Concentration dependent bactericidal activity • Approved to treat UTIs caused by E. coli, K. pneumoniae, Proteus spp, and Enterobacter cloaecae 2 9/23/2018 Aminoglycoside Shortcomings Toxicities Resistance • Nephrotoxicity • Decreased cell permeability • Ototoxicity • Altered ribosome binding sites • Therapeutic drug monitoring • AMG‐modifying enzymes (AME) Plazomicin: Efficacy • Study 009: • RCT comparing plazomicin IV to meropenem IV for cUTI caused by enterobactereceae • Plazomicin group was non‐inferior to meropenem group • Study 007: • RCT comparing plazomicin IV to polymyxin E IV for BSI cause by carbapenem‐resistant Enterobacteriaceae (CRE) • Plazomicin was associated with less mortality compared to polymyxin E Connolly L, Achaogen, Inc. -
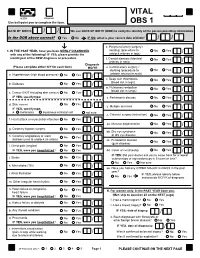
VITAL Jan 2019 Follow-Up
VITAL 6308 Request Use ball-point pen to complete the form. OBS 1 DATE OF BIRTH: / / We use DATE OF BIRTH (DOB) to verify the identity of the person providing information. Is the DOB above correct? Yes No IF NO, what is your correct date of birth? / / s. Peripheral artery surgery / 1. IN THE PAST YEAR, have you been NEWLY DIAGNOSED stenting (procedure to No Yes / with any of the following? IF YES, please provide the unblock arteries in legs) month/year of the NEW diagnosis or procedure. t. Carotid stenosis (blocked No Yes Answer NO/YES on each line. arteries in neck) / Diagnosis (Please complete either N/Y for each item) MO/YR u. Carotid artery surgery / stenting (procedure to No Yes / a. Hypertension (high blood pressure) No Yes / unblock arteries in neck) v. Deep vein thrombosis No Yes (blood clot in legs) / b. Diabetes No Yes / w. Pulmonary embolism No Yes (blood clot in lungs) / c. Cancer (NOT including skin cancer) No Yes / IF YES, specify type: _______________________ x. Parkinson's disease No Yes / d. Skin cancer No Yes / y. Multiple sclerosis No Yes IF YES, specify type: / e. melanoma squamous or basal cell not sure z. Cataract surgery (extraction) No Yes / f. Heart attack or myocardial infarction No Yes / aa. Macular degeneration No Yes / g. Coronary bypass surgery No Yes / bb. Dry eye syndrome No Yes or dry eye disease / h. Coronary angioplasty or stent No Yes (balloon used to unblock an artery) / cc. Periodontal disease No Yes (gum disease) / i. Chest pain (angina) No Yes / IF YES, were you hospitalized? No Yes dd.