Compendium of Urinalysis Urine Test Strips and Microscopy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WELLNESS SCREENING TEST EXPLANATION SHEET We Encourage You to Share All Lab Results with Your Primary Care Provider
WELLNESS SCREENING TEST EXPLANATION SHEET We encourage you to share all lab results with your primary care provider. EXPLANATION OF BLOOD TESTS HEMOGLOBIN A1C: A Hemoglobin A1c level is HEMATOLOGY WELLNESS: expressed as a percent and is used to evaluate the Blood counts are often used as a broad screening test average amount of glucose in the blood over the last to determine an individual’s general health status. 2 to 3 months. This test may be used to screen for and White blood cells are the cells that are part of the diagnose diabetes or risk of developing diabetes. body’s defense system against infections and cancer and also play a role in allergies and inflammation. ALT: This test is used to determine if a patient has Red blood cells are the cells that transport oxygen liver damage. In healthy individuals, ALT levels in the throughout the body. Hemoglobin measures the blood are low and they rise in various disease states. total amount of the oxygen-carrying protein in the blood, which generally reflects the number of red CALCIUM: A calcium test is ordered to screen for, blood cells in the blood. Hematocrit measures the diagnose and monitor a range of conditions percentage of a person’s total blood volume that relating to the bones, heart, nerves, kidneys and consists of red blood cells. Platelets are cell fragments teeth. The test may also be ordered if a person has that are vital for normal blood clotting. symptoms of parathyroid disorder, malabsorption or an overactive thyroid. FREE T4: Free T4 is used to help evaluate thyroid function, generally after determining the TSH is CREATININE: The creatinine blood test is used to abnormal. -

Hyperbilirubinemia
Porphyrins Porphyrins (Porphins) are cyclic tetrapyrol compounds formed by the linkage )). of four pyrrole rings through methenyl bridges (( HC In the reduced porphyrins (Porphyrinogens) the linkage of four pyrrole rings (tetrapyrol) through methylene bridges (( CH2 )) The characteristic property of porphyrins is the formation of complexes with the metal ion bound to nitrogen atoms of the pyrrole rings. e.g. Heme (iron porphyrin). Proteins which contain heme ((hemoproteins)) are widely distributed e.g. Hemoglobin, Myoglobin, Cytochromes, Catalase & Tryptophan pyrrolase. Natural porphyrins have substituent side chains on the eight hydrogen atoms numbered on the pyrrole rings. These side chains are: CH 1-Methyl-group (M)… (( 3 )) 2-Acetate-group (A)… (( CH2COOH )) 3-Propionate-group (P)… (( CH2CH2COOH )) 4-Vinyl-group (V)… (( CH CH2 )) Porphyrins with asymmetric arrangement of the side chains are classified as type III porphyrins while those with symmetric arrangement of the side chains are classified as type I porphyrins. Only types I & III are present in nature & type III series is more important because it includes heme. 1 Heme Biosynthesis Heme biosynthesis occurs through the following steps: 1-The starting reaction is the condensation between succinyl-CoA ((derived from citric acid cycle in the mitochondria)) & glycine, this reaction is a rate limiting reaction in the hepatic heme synthesis, it occurs in the mitochondria & is catalyzed by ALA synthase (Aminolevulinate synthase) enzyme in the presence of pyridoxal phosphate as a cofactor. The product of this reaction is α-amino-β-ketoadipate which is rapidly decarboxylated to form δ-aminolevulinate (ALA). 2-In the cytoplasm condensation reaction between two molecules of ALA is catalyzed by ALA dehydratase enzyme to form two molecules of water & one 2 molecule of porphobilinogen (PBG) which is a precursor of pyrrole. -
Basic Skills in Interpreting Laboratory Data
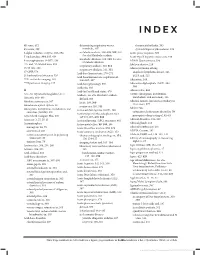
INDEX 4K score, 612 determining respiratory versus rheumatoid arthritis, 505 4Ts score, 399 metabolic, 307 systemic lupus erythematosus, 509 5-alpha reductase enzyme, 593–594 metabolic acidosis, 308–309, 309, 310. Acute phase response, 500 See also Metabolic acidosis 5' nucleotidase, 334, 335, 636 Acute type B hepatitis (minicase), 349 metabolic alkalosis, 309, 310. See also 6-mercaptopurine (6-MP), 138 ADAM Questionnaire, 596 Metabolic alkalosis 13C- and 14C-labeled urea, 353 Addison disease, 219 respiratory acidosis, 310, 311 15/15 rule, 208 Adenocarcinoma of lung respiratory alkalosis, 311, 311 17-OHP, 578 anaplastic lymphoma kinase, 526 Acid-base homeostasis, 270–271 21-hydroxylase deficiency, 526 EGFR and, 525 Acid-base homeostasis, regulation of, 99m Tc-sestamibi imaging, 165 306–307, 307 Adenosine, 164 201 TI perfusion imaging, 165 Acid-base physiology, 306 Adenosine diphosphate (ADP), 394, Acidemia, 303 394 A Acid-fast bacilli and stains, 470 Adenoviridae, 456 A1c. See Glycated hemoglobin (A1c) Acidosis. See also Metabolic acidosis ADME (absorption, distribution, metabolism, and excretion), 136 Abacavir, 468–469 defined, 303 Adnexal tumors, hirsutism secondary to Absolute neutropenia, 387 lactic, 308, 309 (minicase), 577 Absorbance optical system, 28 respiratory, 310, 311 Adolescents Absorption, distribution, metabolism, and Activated clotting time (ACT), 408 excretion (ADME), 136 categories of substances abused by, 70 Activated partial thromboplastin time prerequisite drug testing of, 82–83 Accu Check Compact Plus, 200 (aPTT), -

Diagnosis of Insulinoma in a Maine Coon
JOR0010.1177/2055116919894782Journal of Feline Medicine and Surgery Open ReportsGifford et al 894782research-article2020 Case Report Journal of Feline Medicine and Surgery Open Reports Diagnosis of insulinoma in 1 –10 © The Author(s) 2020 Article reuse guidelines: a Maine Coon cat sagepub.com/journals-permissions DOI:https://doi.org/10.1177/2055116919894782 10.1177/2055116919894782 journals.sagepub.com/home/jfmsopenreports This paper was handled and processed by the American Editorial Office (AAFP) 1 2 3 Carol H Gifford , Anita P Morris , Kurt J Kenney and for publication in JFMS Open Reports J Scot Estep4 Abstract Case summary A 9-year-old male neutered Maine Coon cat presented with a 6-month history of polyphagia and one recent episode of tremors and weakness. Blood work revealed profound hypoglycemia and results of a paired insulin glucose test were consistent with an insulinoma. Abdominal ultrasound revealed a solitary pancreatic mass, and results of a fine-needle aspirate (FNA) gave further support for the location of the neuroendocrine tumor. After unsuccessful medical management of the hypoglycemia, the mass was surgically removed. Immunohistochemistry confirmed that it was an insulinoma. At the time of writing, the patient had been in clinical remission for 9 months. Relevance and novel information Feline insulinomas are rare and there is very little information on their behavior, clinical course and histologic characteristics. This is the first reported case of an insulinoma in a Maine Coon cat and the first to describe results of an ultrasound-guided FNA of the mass. In addition, the progression of disease, histopathology and immunohistochemistry results add to the currently minimal database for feline insulinomas. -

Modelling of Red Blood Cell Morphological and Deformability Changes During In-Vitro Storage
applied sciences Article Modelling of Red Blood Cell Morphological and Deformability Changes during In-Vitro Storage Nadeeshani Geekiyanage 1 , Emilie Sauret 1,*, Suvash Saha 2 , Robert Flower 3 and YuanTong Gu 1 1 School of Mechanical, Medical and Process Engineering, Science and Engineering Faculty, Queensland University of Technology (QUT), Brisbane City, QLD 4000, Australia; [email protected] (N.G.); [email protected] (Y.G.) 2 School of Mechanical and Mechatronic Engineering, University of Technology Sydney (UTS), Ultimo, NSW 2007, Australia; [email protected] 3 Research and Development, Australian Red Cross Lifeblood, Kelvin Grove, QLD 4059, Australia; [email protected] * Correspondence: [email protected] Received: 28 February 2020; Accepted: 27 April 2020; Published: 4 May 2020 Featured Application: Red blood cell (RBC) storage lesion is a critical issue facing transfusion treatments, and significant changes in RBC morphology and deformability are observed due to the storage lesion. RBCs require high deformability to sustain in-vivo circulation, and impaired deformability leads to several post-transfusion adverse outcomes. Therefore, improved understanding of the interrelation between the morphological and deformability changes and the quality and viability of the stored RBCs is essential to prevent or reduce the transfusion related adverse outcomes. To support this requisite, the influence on RBC deformability due to several aspects of the storage lesion, namely, the changes in cell morphology, surface area and volume, RBC membrane biomechanics, and cytoskeletal structural integrity are explored numerically in this study. Abstract: Storage lesion is a critical issue facing transfusion treatments, and it adversely affects the quality and viability of stored red blood cells (RBCs). -

Characterisation of Bilirubin Metabolic Pathway in Hepatic Mitochondria Siti Nur Fadzilah Muhsain M.Sc
Characterisation of Bilirubin Metabolic Pathway in Hepatic Mitochondria Siti Nur Fadzilah Muhsain M.Sc. (Medical Research) 2005 Universiti Sains Malaysia Postgrad. Dip. (Toxicology) 2003 University of Surrey B.Sc.(Biomed. Sc.) 2000 Universiti Putra Malaysia A thesis submitted for the degree of Doctor of Philosophy at The University of Queensland in 2014 School of Medicine ABSTRACT Bilirubin (BR), a toxic waste product of degraded haem, is a potent antioxidant at physiological concentrations. To achieve the maximum benefit of BR, its intracellular level needs to be carefully regulated. A system comprising of two enzymes, haem oxygenase-1 (HMOX1) and cytochrome P450 2A5 (CYP2A5) exists in the endoplasmic reticulum (ER), responsible for regulating BR homeostasis. This system is induced in response to oxidative stress. In this thesis, oxidative stress caused accumulation of these enzymes in mitochondria — major producers and targets of reactive oxygen species (ROS) — is demonstrated. To understand the significance of this intracellular targeting, properties of microsomal and mitochondrial BR metabolising enzymes were compared and the capacity of mitochondrial CYP2A5 to oxidise BR in response to oxidative stress is reported. Microsomes and mitochondrial fractions were isolated from liver homogenates of DBA/2J mice, administered with sub-toxic dose of pyrazole, an oxidant stressor. The purity of extracted organelles was determined by analysing the expressions and activities of their respective marker enzymes. HMOX1 and CYP2A5 were significantly increased in microsomes and even more so in mitochondria in response to pyrazole-induced oxidative stress. By contrast, the treatment did not increase either microsomes or mitochondrial Uridine-diphosphate-glucuronosyltransferase 1A1 (UGT1A1), the sole enzyme that catalyses BR elimination through glucuronidation. -

Bilirubin (Urine) Interpretive Summary
Bilirubin (Urine) Interpretive Summary Description: Bilirubinuria is an indicator of conjugated bilirubin in the urine. Excessive bilirubinuria in a dog or any bilirubinuria in a cat is an indication to evaluate serum bilirubin concentrations. Decreased Bilirubin Common Causes Normal Artifact o Exposure to UV light or room air o Delayed analysis o Centrifugation of urine prior to analysis o Ascorbic acid (Vitamin C) Increased Bilirubin Common Causes Normal dogs (especially males with concentrated urine) Liver disease, bile duct obstruction RBC destruction (hemolysis) o Immune-mediated hemolytic anemia o Zinc or onion toxicity o RBC parasites Uncommon Causes Hemoglobinuria Fever Prolonged anorexia False positive reactions due to medications o Phenothiazines (e.g., chlorpromazine) o Etodolac Related Findings Liver disease, biliary obstruction o Increased serum bilirubin, ALT, ALP, GGT, AST o Increased serum bile acids o Decreased albumin, cholesterol, BUN and glucose in severe cases o Abnormalities in liver and/or biliary tract on abdominal ultrasound RBC destruction o Decreased hematocrit, RBC, hemoglobin o Increased reticulocytes, increased MCV and decreased MCHC, polychromasia o Increased serum bilirubin o Spherocytosis (in dogs), autoagglutination o Hemoglobinuria o Positive Coombs or saline agglutination test may or may not be present with IMHA Generated by VetConnect® PLUS: Bilirubin (Urine) Page 1 of 2 Additional Information Physiology Conjugated bilirubin passes freely through the glomerular filtration barrier and is excreted in urine. Unconjugated bilirubin is bound to albumin and does not normally pass through the glomerular filtration barrier. Therefore, it is not detectable in urine (unless albuminuria or glomerular disease is present). Bilirubinuria usually precedes hyperbilirubinemia and icterus Dogs: Clinically normal dogs (especially males) may have detectable bilirubinuria in concentrated urine due to a low renal threshold for bilirubin. -

Interpretation of Canine and Feline Urinalysis
$50. 00 Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Preface Urine is that golden body fluid that has the potential to reveal the answers to many of the body’s mysteries. As Thomas McCrae (1870-1935) said, “More is missed by not looking than not knowing.” And so, the authors would like to dedicate this handbook to three pioneers of veterinary nephrology and urology who emphasized the importance of “looking,” that is, the importance of conducting routine urinalysis in the diagnosis and treatment of diseases of dogs and cats. To Dr. Carl A. Osborne , for his tireless campaign to convince veterinarians of the importance of routine urinalysis; to Dr. Richard C. Scott , for his emphasis on evaluation of fresh urine sediments; and to Dr. Gerald V. Ling for his advancement of the technique of cystocentesis. Published by The Gloyd Group, Inc. Wilmington, Delaware © 2004 by Nestlé Purina PetCare Company. All rights reserved. Printed in the United States of America. Nestlé Purina PetCare Company: Checkerboard Square, Saint Louis, Missouri, 63188 First printing, 1998. Laboratory slides reproduced by permission of Dennis J. Chew, DVM and Stephen P. DiBartola, DVM. This book is protected by copyright. ISBN 0-9678005-2-8 Table of Contents Introduction ............................................1 Part I Chapter 1 Sample Collection ...............................................5 -

A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening
Kobe J. Med. Sci., Vol. 56, No. 4, pp. E165-E172, 2010 A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening NATSUKO MAKIHARA1, MINEO YAMASAKI1,2, HIROKI MORITA1, and HIDETO YAMADA1* 1Division of Obstetrics and Gynecology, Department of Surgery-related, and 2Division of Integrated Medical Education, Department of Community Medicine and Social Healthcare Science, Kobe University Graduate School of Medicine, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe, 650-0017, Japan. Received 12 July 2010/ Accepted 20 August 2010 Key Words: dipstick test, pregnancy proteinuria, protein/creatinine ratio, urine specific gravity Proteinuria screening using a semi-quantitative dipstick test of the spot urine in antenatal clinic is known to have high false-positive rates. The aim of this study was to assess availability of a dipstick test combined with the urine specific gravity for the determination of pathological proteinuria. A dipstick test was performed on 582 urine samples obtained from 283 pregnant women comprising 260 with normal blood pressure and 23 with pregnancy-induced hypertension. The urine protein (P) and creatinine (C) concentrations, specific gravity (SG), P/C ratio were determined, and compared with dipstick test results. The P concentration increased along the stepwise augmentations in dipstick test result. Frequencies of the urine samples with 0.265 or more P/C ratio were 0.7% with − dipstick test result, 0.7% with the ± result, 3.3% with the 1+ result, and 88.9% with the ≥2+ result. However, if the urine specific gravity was low, frequencies of the high P/C ratio were 5.0% with ± dipstick test result and 9.3% with the 1+ result. -

A Brief Overview of Urology's Development
A brief overview of urology’s development Milestones in urology show evolutionary growth Prof. Manuel Mendes upper urinary tract diseases, namely kidney disease, Modern advances Silva with Albarran’s invention of a moveable “lever” for Advances continue to be made, not only in Former president adjusting the cystoscope, making it possible to insert fundamental aspects of the basic sciences, but also in Portuguese tubes (catheters) up into the ureters and kidneys. This new and sophisticated methods of diagnosis and Association of Urology made it possible to analyse the urine produced by treatment. These include computerised imaging Lisbon (PT) each kidney separately, thereby facilitating lateral techniques: ultrasound, computed axial tomography diagnosis. The most common diseases of the time, of (CAT), magnetic resonance imaging (MRI), digital and which tuberculosis was the most prevalent, were very Doppler angiography, radioactive isotopes; analytical, mmendessilva@ different from those we see today. immunological, genetic and pathology-based sapo.pt methods of diagnosis; sophisticated tools for studying urodynamics; new methods of endoscopic and laser “...it was only toward the end of the diagnosis and treatment, such as endourology Urinary and genital diseases have been around since century, after electricity came into (ureterorenoscopy, percutaneous surgery), internal time immemorial. We know this from the evidence and external shockwave lithotripsy, laparoscopy and left behind –urinary stones discovered in Egyptian use, that Max Nitze (1877) achieved laparoscopic surgery, and robotic surgery and mummies and alongside numerous skeletal remains- a good quality cystoscopy using a telesurgery; control of infection with vaccines and and in vestiges of ancient civilisations such as new generation antibiotics; new techniques for paintings and writing tablets. -

Usmle Rx Qbank 2017 Step 1 Renal
Item: 1 of 24 ~ 1 • M k -<:J 1>- Jil ~· !:';-~ QIO: 4749 ..L a r Previous Next Labfli!llues Not es Calculat o r • 1 & & A 67-year-old man admitted for postoperative recovery is found to be oliguric. Laboratory studies show a blood urea nitrogen level of 200 • 2 mg/dl and a serum creatinine level of 6 mg/dl. Urinalysis shows: • 3 Specific gravity: 1.050 · 4 Urine osmolality: 670 mOsm/kg • 5 Sodium: 14 mEq/L BUN/Creatinine ratio: 56 • 6 Fractional excretion of Na: 0.54% • 7 Protein: negative Casts: negative · 8 . 9 • 10 Which of the following is the most likely cause of this patient's oliguria? • 11 : • 12 A. Acute interstitial nephritis • 13 B. Acute tubular necrosis • 14 C. Bladder calculus • 15 • 16 D. Heart failure • 17 E. Nephrotic syndrome • 18 • 19 • 20 • 21 • a s 8 Lock Suspend End Block Item: 1of24 ~ . , . M k <:] t> al ~· ~ QIO: 4749 .l. ar Previous Next Lab'lifllues Notes Calculator 1 • The correct a nswer is 0. 4 80/o c hose t his. • 2 This patient's laboratory tests confirm the classic criteria for d iagnosing prerenal azotemia. Prerenal azotemia is caused by a reduction of the • 3 g lomerular filtration rate (GFR} provoked by an insult to the vascular supply to the kidney. Causes of prerenal azotemia include heart failure, sepsis, and renal artery stenosis. The reduction in GFR increases the accumulation of both blood urea nitrogen (BUN} and creatinine (Cr} in the • 4 blood, but because the BUN concentration in blood is determined by both g lomerular filtration and reabsorption (in contrast to Cr, which is • 5 limited to filtration and not reabsorbed}, the BUN level rises out of proportion to the Cr leveL This therefore elevates the BUN :Cr ratio. -

The Effect of Medicine, in Particular the Ideas About Renal Diseases, on the “Well-Being” of Byzantine Citizens
93 A TH A N A SIOS D I A M A N D OPOULOS The Effect of Medicine, in particular the Ideas about Renal Diseases, on the “Well-being” of Byzantine Citizens At first sight it is rather strange that a conference on “Material Culture and Well-Being in Byzantium” should include a topic about a medical specialty. Medicine, tiptoeing hesitantly between the realm of sci- ences and that of humanities, is not automatically classified as “Material Culture”. On second thoughts, there are arguments from medicine’s past and present, which plead in favour of such an inclusion. The most famous of all the existing ancient medical Greek codices is the Materia Medica, which was written by the 1st cent. AD medical writer Dioscurides, and then copied in Constantinople, at the beginning of the 6th cent1. As its title shows, medicine cannot be practised without the use of material substances, the medicaments, which are minutely listed in the text. It is tempting, however, to add, that Galen the most pro- lific and most self-assured of all ancient medical writers, found Dioscurides᾽s Greek grossly inferior, but he, at least, accepted that the medical information in Materia Medica was correct. On the other hand the over-all aim of medicine is to prevent the destruction of people’s sense of well-being and to restore it when in decline during times of a disease. Hence, I think that such a topic is relevant to the conference. Before we proceed to the specific role of nephrology (i.e. the medical specialty dealing with kidney ailments) I will present some general characteristics of Byzantine medicine, and I will outline why an interest in it has arisen3.