SAM-Pointed Domain ETS Factor Mediates Epithelial Cell–Intrinsic Innate Immune Signaling During Airway Mucous Metaplasia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Apoptotic Cells Inflammasome Activity During the Uptake of Macrophage
Downloaded from http://www.jimmunol.org/ by guest on September 29, 2021 is online at: average * The Journal of Immunology , 26 of which you can access for free at: 2012; 188:5682-5693; Prepublished online 20 from submission to initial decision 4 weeks from acceptance to publication April 2012; doi: 10.4049/jimmunol.1103760 http://www.jimmunol.org/content/188/11/5682 Complement Protein C1q Directs Macrophage Polarization and Limits Inflammasome Activity during the Uptake of Apoptotic Cells Marie E. Benoit, Elizabeth V. Clarke, Pedro Morgado, Deborah A. Fraser and Andrea J. Tenner J Immunol cites 56 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription http://www.jimmunol.org/content/suppl/2012/04/20/jimmunol.110376 0.DC1 This article http://www.jimmunol.org/content/188/11/5682.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2012 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 29, 2021. The Journal of Immunology Complement Protein C1q Directs Macrophage Polarization and Limits Inflammasome Activity during the Uptake of Apoptotic Cells Marie E. -

Rna-Sequencing Applications: Gene Expression Quantification and Methylator Phenotype Identification
The Texas Medical Center Library DigitalCommons@TMC The University of Texas MD Anderson Cancer Center UTHealth Graduate School of The University of Texas MD Anderson Cancer Biomedical Sciences Dissertations and Theses Center UTHealth Graduate School of (Open Access) Biomedical Sciences 8-2013 RNA-SEQUENCING APPLICATIONS: GENE EXPRESSION QUANTIFICATION AND METHYLATOR PHENOTYPE IDENTIFICATION Guoshuai Cai Follow this and additional works at: https://digitalcommons.library.tmc.edu/utgsbs_dissertations Part of the Bioinformatics Commons, Computational Biology Commons, and the Medicine and Health Sciences Commons Recommended Citation Cai, Guoshuai, "RNA-SEQUENCING APPLICATIONS: GENE EXPRESSION QUANTIFICATION AND METHYLATOR PHENOTYPE IDENTIFICATION" (2013). The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access). 386. https://digitalcommons.library.tmc.edu/utgsbs_dissertations/386 This Dissertation (PhD) is brought to you for free and open access by the The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences at DigitalCommons@TMC. It has been accepted for inclusion in The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access) by an authorized administrator of DigitalCommons@TMC. For more information, please contact [email protected]. RNA-SEQUENCING APPLICATIONS: GENE EXPRESSION QUANTIFICATION AND METHYLATOR PHENOTYPE IDENTIFICATION -

HIT'ndrive: Patient-Specific Multidriver Gene Prioritization for Precision Oncology
Downloaded from genome.cshlp.org on October 4, 2021 - Published by Cold Spring Harbor Laboratory Press Method HIT’nDRIVE: patient-specific multidriver gene prioritization for precision oncology Raunak Shrestha,1,2,10 Ermin Hodzic,3,10 Thomas Sauerwald,4 Phuong Dao,5 Kendric Wang,2 Jake Yeung,2 Shawn Anderson,2 Fabio Vandin,6 Gholamreza Haffari,7 Colin C. Collins,2,8 and S. Cenk Sahinalp2,3,9 1Bioinformatics Training Program, University of British Columbia, Vancouver, British Columbia, Canada V6T 1Z4; 2Laboratory for Advanced Genome Analysis, Vancouver Prostate Centre, Vancouver, British Columbia, Canada V6H 3Z6; 3School of Computing Science, Simon Fraser University, Burnaby, British Columbia, Canada V5A 1S6; 4Computer Laboratory, University of Cambridge, Cambridge CB3 0FD, United Kingdom; 5National Center for Biotechnology Information, National Library of Medicine, National Institutes of Health, Bethesda, Maryland 20894, USA; 6Department of Information Engineering, University of Padova, 35131 Padova, Italy; 7Faculty of Information Technology, Monash University, Melbourne 3800, Australia; 8Department of Urologic Sciences, University of British Columbia, Vancouver, British Columbia, Canada V5Z 1M9; 9School of Informatics and Computing, Indiana University, Bloomington, Indiana 47408, USA Prioritizing molecular alterations that act as drivers of cancer remains a crucial bottleneck in therapeutic development. Here we introduce HIT’nDRIVE, a computational method that integrates genomic and transcriptomic data to identify a set of patient-specific, sequence-altered genes, with sufficient collective influence over dysregulated transcripts. HIT’nDRIVE aims to solve the “random walk facility location” (RWFL) problem in a gene (or protein) interaction network, which differs from the standard facility location problem by its use of an alternative distance measure: “multihitting time,” the expected length of the shortest random walk from any one of the set of sequence-altered genes to an expression-altered target gene. -

Ras Signaling Requires Dynamic Properties of Ets1 for Phosphorylation-Enhanced Binding to Coactivator CBP
Ras signaling requires dynamic properties of Ets1 for phosphorylation-enhanced binding to coactivator CBP Mary L. Nelsona,1, Hyun-Seo Kangb,1, Gregory M. Leeb, Adam G. Blaszczaka, Desmond K. W. Laub, Lawrence P. McIntoshb,2, and Barbara J. Gravesa,2 aDepartment of Oncological Sciences, University of Utah School of Medicine, Huntsman Cancer Institute, University of Utah, Salt Lake City, UT, 84112; and bDepartment of Biochemistry and Molecular Biology, Department of Chemistry, and the Michael Smith Laboratories, University of British Columbia, Vancouver, BC, Canada V6T 1Z3 Edited by Peter E. Wright, The Scripps Research Institute, La Jolla, CA, and approved April 8, 2010 (received for review January 4, 2010) Ras/MAPK signaling is often aberrantly activated in human can- Here we describe the coupled roles of the PNT domain and an cers. The downstream effectors are transcription factors, including adjacent disordered region bearing both Thr38 and a previously those encoded by the ETS gene family. Using cell-based assays and unrecognized phosphoacceptor, Ser41, in the ERK2-enhanced biophysical measurements, we have determined the mechanism by binding of the CBP TAZ1 domain by Ets1. Phosphorylation plays which Ras/MAPK signaling affects the function of Ets1 via phos- a dual role by altering a conformational equilibrium of a dynamic phorylation of Thr38 and Ser41. These ERK2 phosphoacceptors helix H0 that tethers the flexible phosphorylated region of Ets1 to lie within the unstructured N-terminal region of Ets1, immediately the core PNT domain and by augmenting electrostatic forces that adjacent to the PNT domain. NMR spectroscopic analyses demon- drive TAZ1 recognition. In this integrated model, structured ele- strated that the PNT domain is a four-helix bundle (H2–H5), resem- ments with intrinsic flexibility provide a scaffold for responsive- bling the SAM domain, appended with two additional helices ness to a signaling pathway. -
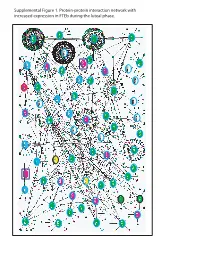
Supplemental Figure 1. Protein-Protein Interaction Network with Increased Expression in Fteb During the Luteal Phase
Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during luteal phase. LEGENDS TO SUPPLEMENTAL FIGURES Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with increased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. Genes encoding proteins shown as large ovals highlighted in blue were exclusively found in the first comparison (Manuscript Figure 2), whereas those highlighted in red were only found in the second comparison (Manuscript Figure 3). Genes encoding proteins shown as large ovals highlighted in black were found in both comparisons. The color of each node indicates the ontology of the corresponding protein as determined by the Online Predicted Human Interaction Database (OPHID) link with the NAViGaTOR software. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with decreased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. -

SPDEF (NM 001252294) Human Tagged ORF Clone Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for RG232468 SPDEF (NM_001252294) Human Tagged ORF Clone Product data: Product Type: Expression Plasmids Product Name: SPDEF (NM_001252294) Human Tagged ORF Clone Tag: TurboGFP Symbol: SPDEF Synonyms: bA375E1.3; PDEF Vector: pCMV6-AC-GFP (PS100010) E. coli Selection: Ampicillin (100 ug/mL) Cell Selection: Neomycin ORF Nucleotide >RG232468 representing NM_001252294 Sequence: Red=Cloning site Blue=ORF Green=Tags(s) TTTTGTAATACGACTCACTATAGGGCGGCCGGGAATTCGTCGACTGGATCCGGTACCGAGGAGATCTGCC GCCGCGATCGCC ATGGGCAGCGCCAGCCCGGGTCTGAGCAGCGTATCCCCCAGCCACCTCCTGCTGCCCCCCGACACGGTGT CGCGGACAGGCTTGGAGAAGGCGGCAGCGGGGGCAGTGGGTCTCGAGAGACGGGACTGGAGTCCCAGTCC ACCCGCCACGCCCGAGCAGGGCCTGTCCGCCTTCTACCTCTCCTACTTTGACATGCTGTACCCTGAGGAC AGCAGCTGGGCAGCCAAGGCCCCTGGGGCCAGCAGTCGGGAGGAGCCACCTGAGGAGCCTGAGCAGTGCC CGGTCATTGACAGCCAAGCCCCAGCGGGCAGCCTGGACTTGGTGCCCGGCGGGCTGACCTTGGAGGAGCA CTCGCTGGAGCAGGTGCAGTCCATGGTGGTGGGCGAAGTGCTCAAGGACATCGAGACGGCCTGCAAGCTG CTCAACATCACCGCAGATCCCATGGACTGGAGCCCCAGCAATGTGCAGAAGTGGCTCCTGTGGACAGAGC ACCAATACCGGCTGCCCCCCATGGGCAAGGCCTTCCAGGAGCTGGCGGGCAAGGAGCTGTGCGCCATGTC GGAGGAGCAGTTCCGCCAGCGCTCGCCCCTGGGTGGGGATGTGCTGCACGCCCACCTGGACATCTGGAAG TCAGCCTCGACCAGTGAGGAGAGCTGGACCGACAGCGAGGTGGACTCATCATGCTCCGGGCAGCCCATCC ACCTGTGGCAGTTCCTCAAGGAGTTGCTACTCAAGCCCCACAGCTATGGCCGCTTCATTAGGTGGCTCAA CAAGGAGAAGGGCATCTTCAAAATTGAGGACTCAGCCCAGGTGGCCCGGCTGTGGGGCATCCGCAAGAAC CGTCCCGCCATGAACTACGACAAGCTGAGCCGCTCCATCCGCCAGTATTACAAGAAGGGCATCATCCGGA -

Efficient RNP-Directed Human Gene Targeting Reveals SPDEF Is Required for IL-13-Induced Mucostasis
bioRxiv preprint doi: https://doi.org/10.1101/716670; this version posted July 28, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Efficient RNP-directed human gene targeting reveals SPDEF is required for IL-13-induced mucostasis Kyung Duk Koh1,2*, Sana Siddiqui3*, Dan Cheng1,2,5*, Luke R. Bonser1,2, Dingyuan I. Sun4, Lorna T. Zlock4, Walter E. Finkbeiner4, Prescott G. Woodruff2,3, and David J. Erle1,2,3 1Lung Biology Center, 2Cardiovascular Research Institute, 3Division of Pulmonary, Critical Care, Sleep, and Allergy, and 4Department of Pathology, University of California San Francisco, San Francisco, CA 94143 and 5Department of Respiratory and Critical Care Medicine, Renmin Hospital of Wuhan University, Wuhan, China 430060 *Equal contributions Address correspondence to: David J. Erle, MD University of California San Francisco, CVRI - MC: 3118 San Francisco, CA 94158-9001 Tel 415-514-4370; Fax 415-514-1173 E-mail: [email protected] Author contributions: KDK, SS, LRB, PGW, and DJE contributed to study conception and design. KDK and SS developed novel experimental methods. KDK, DC, LRB, DIS, and LTZ performed experiments. KDK and DC analyzed data. KDK, SS, DC, LRB, and DJE interpreted data. WEF, PGW, and DJE supervised study execution. KDK drafted the manuscript. KDK, SS, DC, LRB, DIS, LTZ, WEF, PGW, and DJE revised the manuscript. Support: National Institutes of Health grants U19 AI 077439, R35 HL145235, and R01 HL138424 (DJE). National Institutes of Health grant DK072517 and Cystic Fibrosis Foundation grant DR613-CR11 (WEF). -

Genome-Wide Analysis Reveals Mucociliary Remodeling of the Nasal Airway Epithelium Induced by Urban PM2.5 Michael T
ORIGINAL RESEARCH Genome-Wide Analysis Reveals Mucociliary Remodeling of the Nasal Airway Epithelium Induced by Urban PM2.5 Michael T. Montgomery1, Satria P. Sajuthi1, Seung-Hyun Cho2, Jamie L. Everman1, Cydney L. Rios1, Katherine C. Goldfarbmuren1, Nathan D. Jackson1, Benjamin Saef1, Meghan Cromie1, Celeste Eng3, Vivian Medina4, Jennifer R. Elhawary3, Sam S. Oh3, Jose Rodriguez-Santana4, Eszter K. Vladar5,6, Esteban G. Burchard3,7, and Max A. Seibold1,5,8 1Center for Genes, Environment, and Health, and 8Department of Pediatrics, National Jewish Health, Denver, Colorado; 2RTI International, Research Triangle Park, North Carolina; 3Department of Medicine and 7Department of Bioengineering and Therapeutic Sciences, University of California San Francisco, San Francisco, California; 4Centro de Neumologıa´ Pediatrica, ´ San Juan, Puerto Rico; and 5Division of Pulmonary Sciences and Critical Care Medicine, Department of Medicine and 6Department of Cell and Developmental Biology, University of Colorado School of Medicine, Aurora, Colorado ORCID IDs: 0000-0002-6748-2329 (M.T.M.); 0000-0001-9821-6667 (S.-H.C.); 0000-0002-1935-4672 (J.L.E.); 0000-0001-8774-7454 (K.C.G.); 0000-0003-3326-1680 (J.R.E.); 0000-0002-2815-6037 (S.S.O.); 0000-0002-4160-8894 (E.K.V.); 0000-0001-7475-2035 (E.G.B.); 0000-0002-8685-4263 (M.A.S.). Abstract mucus secretory expression program (.100 genes), which included transcriptional drivers of mucus metaplasia (SPDEF , FOXA3 fi Air pollution particulate matter 2.5 mm (PM2.5) exposure is and ). Exposure to a higher OE dose modi ed the associated with poor respiratory outcomes. Mechanisms underlying expression of 1,240 genes and further exacerbated expression PM2.5-induced lung pathobiology are poorly understood but likely responses observed at the moderate dose, including the mucus involve cellular and molecular changes to the airway epithelium. -

Genome-Scale Analysis of DNA Methylation in Lung Adenocarcinoma and Integration with Mrna Expression
Downloaded from genome.cshlp.org on September 30, 2021 - Published by Cold Spring Harbor Laboratory Press Research Genome-scale analysis of DNA methylation in lung adenocarcinoma and integration with mRNA expression Suhaida A. Selamat,1 Brian S. Chung,1 Luc Girard,2 Wei Zhang,2 Ying Zhang,3 Mihaela Campan,1 Kimberly D. Siegmund,3 Michael N. Koss,4 Jeffrey A. Hagen,5 Wan L. Lam,6 Stephen Lam,6 Adi F. Gazdar,2 and Ite A. Laird-Offringa1,7 1Department of Surgery, Department of Biochemistry and Molecular Biology, Norris Comprehensive Cancer Center, Keck School of Medicine, University of Southern California, Los Angeles, California 90089-9176, USA; 2The Hamon Center for Therapeutic Oncology Research and Department of Pathology, University of Texas Southwestern Medical Center, Dallas, Texas 75390, USA; 3Department of Preventive Medicine, Keck School of Medicine, University of Southern California, Los Angeles, California 90089-9176, USA; 4Department of Pathology, Keck School of Medicine, University of Southern California, Los Angeles, California 90089-9176, USA; 5Department of Surgery, Keck School of Medicine, University of Southern California, Los Angeles, California 90089-9176, USA; 6BC Cancer Research Center, BC Cancer Agency, Vancouver, BC V521L3, Canada Lung cancer is the leading cause of cancer death worldwide, and adenocarcinoma is its most common histological subtype. Clinical and molecular evidence indicates that lung adenocarcinoma is a heterogeneous disease, which has important implications for treatment. Here we performed genome-scale DNA methylation profiling using the Illumina Infinium HumanMethylation27 platform on 59 matched lung adenocarcinoma/non-tumor lung pairs, with genome-scale verifi- cation on an independent set of tissues. -

Immature Truncated O-Glycophenotype of Cancer Directly
Immature truncated O-glycophenotype of cancer PNAS PLUS directly induces oncogenic features Prakash Radhakrishnana,1, Sally Dabelsteenb,c,1, Frey Brus Madsenb,c, Chiara Francavillad, Katharina L. Koppb, Catharina Steentoftb, Sergey Y. Vakhrushevb, Jesper V. Olsend, Lars Hansenb, Eric P. Bennettb, Anders Woetmanne, Guangliang Yinf, Longyun Chenf, Haiyan Songf, Mads Bakb, Ryan A. Hladya, Staci L. Petersa, Rene Opavskya, Christenze Thodec, Klaus Qvortrupg, Katrine T.-B. G. Schjoldagerb, Henrik Clausenb, Michael A. Hollingswortha, and Hans H. Wandallb,2 aEppley Institute for Research in Cancer, Fred and Pamela Buffet Cancer Center, University of Nebraska Medical Center, Omaha, NE 68198-5950; bCopenhagen Center for Glycomics, Department of Cellular and Molecular Medicine, cDepartment of Pathology and Medicine, School of Dentistry, dProtein Center, gDepartment of Biomedical Sciences/Core Facility for Integrated Microscopy, and eDepartment of Immunology, Faculty of Health Sciences, University of Copenhagen, DK-2200 Copenhagen N, Denmark; and fBGI-Tech, BGI-Shenzhen, Shenzhen 518083, China Edited by Stuart A. Kornfeld, Washington University School of Medicine, St. Louis, MO, and approved July 21, 2014 (received for review April 11, 2014) Aberrant expression of immature truncated O-glycans is a character- nontemplate fashion, orchestrate the diversity of glycan struc- istic feature observed on virtually all epithelial cancer cells, and a very tures found on cells in a surprisingly well-defined manner (12). high frequency is observed in early epithelial premalignant lesions Mucin-type (GalNAc-type) O-glycosylation of proteins is an that precede the development of adenocarcinomas. Expression of the abundant and diverse form of posttranslational modification that truncated O-glycan structures Tn and sialyl-Tn is strongly associated is initiated by a family of up to 20 polypeptide GalNAc-trans- with poor prognosis and overall low survival. -

Downloaded from the TCGA Portal Maintained by GDC
www.nature.com/scientificreports OPEN Identifcation of a Radiosensitivity Molecular Signature Induced by Enzalutamide in Hormone-sensitive Received: 13 November 2018 Accepted: 29 May 2019 and Hormone-resistant Prostate Published: xx xx xxxx Cancer Cells Maryam Ghashghaei1,2, Tamim M. Niazi1,3, Adriana Aguilar-Mahecha4, Kathleen Oros Klein1, Celia M. T. Greenwood 5,6,7,8, Mark Basik4,9 & Thierry M. Muanza1,2,3 Prostate cancer (PCa) is the most common cancer amongst men. A novel androgen receptor (AR) antagonist, enzalutamide (ENZA) has recently been demonstrated to enhance the efect of radiation (XRT) by impairing the DNA damage repair process. This study aimed to identify a radiosensitive gene signature induced by ENZA in the PCa cells and to elucidate the biological pathways which infuence this radiosensitivity. We treated LNCaP (AR-positive, hormone-sensitive PCa cells) and C4-2 (AR-positive, hormone-resistant PCa cells) cells with ENZA alone and in combination with androgen deprivation therapy (ADT) and XRT. Using one-way ANOVA on the gene expression profling, we observed signifcantly diferentially expressed (DE) genes in infammation-and metabolism-related genes in hormone-sensitive and hormone-resistant PCa cell lines respectively. Survival analysis in both the TCGA PRAD and GSE25136 datasets suggested an association between the expression of these genes and time to recurrence. These results indicated that ENZA alone or in combination with ADT enhanced the efect of XRT through immune and infammation-related pathways in LNCaP cells and metabolic-related pathways in C4-2 cells. Kaplan–Meier analysis and Cox proportional hazard models showed that low expression of all the candidate genes except for PTPRN2 were associated with tumor progression and recurrence in a PCa cohort. -

Anti-SPDEF (Full Length) Polyclonal Antibody (DPAB-DC1241) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-SPDEF (full length) polyclonal antibody (DPAB-DC1241) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description The protein encoded by this gene belongs to the ETS family of transcription factors. It is highly expressed in the prostate epithelial cells, and functions as an androgen-independent transactivator of prostate-specific antigen (PSA) promoter. Higher expression of this protein has also been reported in brain, breast, lung and ovarian tumors, compared to the corresponding normal tissues, and it shows better tumor-association than other cancer-associated molecules, making it a more suitable target for developing specific cancer therapies. Alternatively spliced transcript variants encoding different isoforms have been found for this gene. Immunogen SPDEF (AAH21299, 1 a.a. ~ 335 a.a) full-length recombinant protein with GST tag. The sequence is MGSASPGLSSVSPSHLLLPPDTVSRTGLEKAAAGAVGLERRDWSPSPPATPEQGLSAFYLSYF DMLYPEDSSWAAKAPGASSREEPPEEPEQCPVIDSQAPAGSLDLVPGGLTLEEHSLEQVQSMV VGEVLKDIETACKLLNITADPMDWSPSNVQKWLLWTEHQYRLPPMGKAFQELAGKELCAMSEE QFRQRSPLGGDVLHAHLDIWKSAAWMKERTSPGAIHYCASTSEESWTDSEVDSSCSGQPIHLW QFLKELLLKPHSYGRFIRWLNKEKGIFKIEDSAQVARLWGIRKNRPAMNYDKLSRSIRQYYKKGII RKPDISQRLVYQFVHPI Source/Host Mouse Species Reactivity Human Conjugate Unconjugated Applications WB (Cell lysate), WB (Cell lysate), WB (Recombinant protein), ELISA, Size 50 μl Buffer 50 % glycerol Preservative None Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. GENE INFORMATION