Downloaded from the TCGA Portal Maintained by GDC
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genome-Wide Analysis of Androgen Receptor Binding and Gene Regulation in Two CWR22-Derived Prostate Cancer Cell Lines
Endocrine-Related Cancer (2010) 17 857–873 Genome-wide analysis of androgen receptor binding and gene regulation in two CWR22-derived prostate cancer cell lines Honglin Chen1, Stephen J Libertini1,4, Michael George1, Satya Dandekar1, Clifford G Tepper 2, Bushra Al-Bataina1, Hsing-Jien Kung2,3, Paramita M Ghosh2,3 and Maria Mudryj1,4 1Department of Medical Microbiology and Immunology, University of California Davis, 3147 Tupper Hall, Davis, California 95616, USA 2Division of Basic Sciences, Department of Biochemistry and Molecular Medicine, Cancer Center and 3Department of Urology, University of California Davis, Sacramento, California 95817, USA 4Veterans Affairs Northern California Health Care System, Mather, California 95655, USA (Correspondence should be addressed to M Mudryj at Department of Medical Microbiology and Immunology, University of California, Davis; Email: [email protected]) Abstract Prostate carcinoma (CaP) is a heterogeneous multifocal disease where gene expression and regulation are altered not only with disease progression but also between metastatic lesions. The androgen receptor (AR) regulates the growth of metastatic CaPs; however, sensitivity to androgen ablation is short lived, yielding to emergence of castrate-resistant CaP (CRCaP). CRCaP prostate cancers continue to express the AR, a pivotal prostate regulator, but it is not known whether the AR targets similar or different genes in different castrate-resistant cells. In this study, we investigated AR binding and AR-dependent transcription in two related castrate-resistant cell lines derived from androgen-dependent CWR22-relapsed tumors: CWR22Rv1 (Rv1) and CWR-R1 (R1). Expression microarray analysis revealed that R1 and Rv1 cells had significantly different gene expression profiles individually and in response to androgen. -

Apoptotic Cells Inflammasome Activity During the Uptake of Macrophage
Downloaded from http://www.jimmunol.org/ by guest on September 29, 2021 is online at: average * The Journal of Immunology , 26 of which you can access for free at: 2012; 188:5682-5693; Prepublished online 20 from submission to initial decision 4 weeks from acceptance to publication April 2012; doi: 10.4049/jimmunol.1103760 http://www.jimmunol.org/content/188/11/5682 Complement Protein C1q Directs Macrophage Polarization and Limits Inflammasome Activity during the Uptake of Apoptotic Cells Marie E. Benoit, Elizabeth V. Clarke, Pedro Morgado, Deborah A. Fraser and Andrea J. Tenner J Immunol cites 56 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription http://www.jimmunol.org/content/suppl/2012/04/20/jimmunol.110376 0.DC1 This article http://www.jimmunol.org/content/188/11/5682.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2012 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 29, 2021. The Journal of Immunology Complement Protein C1q Directs Macrophage Polarization and Limits Inflammasome Activity during the Uptake of Apoptotic Cells Marie E. -

Rna-Sequencing Applications: Gene Expression Quantification and Methylator Phenotype Identification
The Texas Medical Center Library DigitalCommons@TMC The University of Texas MD Anderson Cancer Center UTHealth Graduate School of The University of Texas MD Anderson Cancer Biomedical Sciences Dissertations and Theses Center UTHealth Graduate School of (Open Access) Biomedical Sciences 8-2013 RNA-SEQUENCING APPLICATIONS: GENE EXPRESSION QUANTIFICATION AND METHYLATOR PHENOTYPE IDENTIFICATION Guoshuai Cai Follow this and additional works at: https://digitalcommons.library.tmc.edu/utgsbs_dissertations Part of the Bioinformatics Commons, Computational Biology Commons, and the Medicine and Health Sciences Commons Recommended Citation Cai, Guoshuai, "RNA-SEQUENCING APPLICATIONS: GENE EXPRESSION QUANTIFICATION AND METHYLATOR PHENOTYPE IDENTIFICATION" (2013). The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access). 386. https://digitalcommons.library.tmc.edu/utgsbs_dissertations/386 This Dissertation (PhD) is brought to you for free and open access by the The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences at DigitalCommons@TMC. It has been accepted for inclusion in The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access) by an authorized administrator of DigitalCommons@TMC. For more information, please contact [email protected]. RNA-SEQUENCING APPLICATIONS: GENE EXPRESSION QUANTIFICATION AND METHYLATOR PHENOTYPE IDENTIFICATION -

Zmiz1a Zebrafish Mutants Have Defective Erythropoiesis, Altered Expression Of
bioRxiv preprint doi: https://doi.org/10.1101/2021.05.14.444216; this version posted May 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. zmiz1a zebrafish mutants have defective erythropoiesis, altered expression of autophagy genes, and a deficient response to vitamin D Francisco Castillo-Castellanos1, Laura Ramírez1, and Hilda Lomelí1* 1Departamento de Genética del Desarrollo y Fisiología Molecular. Instituto de Biotecnología, Universidad Nacional Autónoma de México, *Corresponding author [email protected] Key words: erythropoiesis, zebrafish, autophagy, vitamin D response, ZMIZ1 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.05.14.444216; this version posted May 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. ABSTRACT ZMIZ1 is a transcriptional coactivator that is related to members of the protein inhibitor of activated STAT (PIAS) family. ZMIZ1 regulates the activity of various transcription factors including the androgen receptor, p53, and Smad3. ZMIZ1 also interacts with Notch1 and selectively regulates Notch1 target genes relevant for T cell development and leukemogenesis in mammals. Human ZMIZ1 is additionally characterized as a latitude- dependent autoimmune disease (LDAD) risk gene, as it is responsive to vitamin D and has been associated with at least eleven blood cell traits. To address the function of ZMIZ1 in fish, we introduced CRISPR/Cas9 mutations in the zmiz1a gene in zebrafish. We observed that inactivation of zmiz1a in developing zebrafish larvae results in lethality at 15 dpf and delayed erythroid maturation. -

Upregulation of 15 Antisense Long Non-Coding Rnas in Osteosarcoma
G C A T T A C G G C A T genes Article Upregulation of 15 Antisense Long Non-Coding RNAs in Osteosarcoma Emel Rothzerg 1,2 , Xuan Dung Ho 3 , Jiake Xu 1 , David Wood 1, Aare Märtson 4 and Sulev Kõks 2,5,* 1 School of Biomedical Sciences, The University of Western Australia, Perth, WA 6009, Australia; [email protected] (E.R.); [email protected] (J.X.); [email protected] (D.W.) 2 Perron Institute for Neurological and Translational Science, QEII Medical Centre, Nedlands, WA 6009, Australia 3 Department of Oncology, College of Medicine and Pharmacy, Hue University, Hue 53000, Vietnam; [email protected] 4 Department of Traumatology and Orthopaedics, University of Tartu, Tartu University Hospital, 50411 Tartu, Estonia; [email protected] 5 Centre for Molecular Medicine and Innovative Therapeutics, Murdoch University, Murdoch, WA 6150, Australia * Correspondence: [email protected]; Tel.: +61-(0)-8-6457-0313 Abstract: The human genome encodes thousands of natural antisense long noncoding RNAs (lncR- NAs); they play the essential role in regulation of gene expression at multiple levels, including replication, transcription and translation. Dysregulation of antisense lncRNAs plays indispensable roles in numerous biological progress, such as tumour progression, metastasis and resistance to therapeutic agents. To date, there have been several studies analysing antisense lncRNAs expression profiles in cancer, but not enough to highlight the complexity of the disease. In this study, we investi- gated the expression patterns of antisense lncRNAs from osteosarcoma and healthy bone samples (24 tumour-16 bone samples) using RNA sequencing. -

Colorectal Cancer Risk Genes Are Functionally Enriched in Regulatory
www.nature.com/scientificreports OPEN Colorectal cancer risk genes are functionally enriched in regulatory pathways Received: 07 January 2016 Xi Lu1,*, Mingming Cao2,*, Su Han3, Youlin Yang1 & Jin Zhou4 Accepted: 12 April 2016 Colorectal cancer (CRC) is a common complex disease caused by the combination of genetic variants Published: 05 May 2016 and environmental factors. Genome-wide association studies (GWAS) have been performed and reported some novel CRC susceptibility variants. However, the potential genetic mechanisms for newly identified CRC susceptibility variants are still unclear. Here, we selected 85 CRC susceptibility variants with suggestive association P < 1.00E-05 from the National Human Genome Research Institute GWAS catalog. To investigate the underlying genetic pathways where these newly identified CRC susceptibility genes are significantly enriched, we conducted a functional annotation. Using two kinds of SNP to gene mapping methods including the nearest upstream and downstream gene method and the ProxyGeneLD, we got 128 unique CRC susceptibility genes. We then conducted a pathway analysis in GO database using the corresponding 128 genes. We identified 44 GO categories, 17 of which are regulatory pathways. We believe that our results may provide further insight into the underlying genetic mechanisms for these newly identified CRC susceptibility variants. Colorectal cancer (CRC) is the third most common form of cancer and the second leading cause of cancer-related death in the western world and1,2. CRC is a leading cause of cancer-related deaths in the United States, and its lifetime risk in the United States is about 7%1,3. CRC is a common complex disease caused by the combination of genetic variants and environmental factors1. -

HIT'ndrive: Patient-Specific Multidriver Gene Prioritization for Precision Oncology
Downloaded from genome.cshlp.org on October 4, 2021 - Published by Cold Spring Harbor Laboratory Press Method HIT’nDRIVE: patient-specific multidriver gene prioritization for precision oncology Raunak Shrestha,1,2,10 Ermin Hodzic,3,10 Thomas Sauerwald,4 Phuong Dao,5 Kendric Wang,2 Jake Yeung,2 Shawn Anderson,2 Fabio Vandin,6 Gholamreza Haffari,7 Colin C. Collins,2,8 and S. Cenk Sahinalp2,3,9 1Bioinformatics Training Program, University of British Columbia, Vancouver, British Columbia, Canada V6T 1Z4; 2Laboratory for Advanced Genome Analysis, Vancouver Prostate Centre, Vancouver, British Columbia, Canada V6H 3Z6; 3School of Computing Science, Simon Fraser University, Burnaby, British Columbia, Canada V5A 1S6; 4Computer Laboratory, University of Cambridge, Cambridge CB3 0FD, United Kingdom; 5National Center for Biotechnology Information, National Library of Medicine, National Institutes of Health, Bethesda, Maryland 20894, USA; 6Department of Information Engineering, University of Padova, 35131 Padova, Italy; 7Faculty of Information Technology, Monash University, Melbourne 3800, Australia; 8Department of Urologic Sciences, University of British Columbia, Vancouver, British Columbia, Canada V5Z 1M9; 9School of Informatics and Computing, Indiana University, Bloomington, Indiana 47408, USA Prioritizing molecular alterations that act as drivers of cancer remains a crucial bottleneck in therapeutic development. Here we introduce HIT’nDRIVE, a computational method that integrates genomic and transcriptomic data to identify a set of patient-specific, sequence-altered genes, with sufficient collective influence over dysregulated transcripts. HIT’nDRIVE aims to solve the “random walk facility location” (RWFL) problem in a gene (or protein) interaction network, which differs from the standard facility location problem by its use of an alternative distance measure: “multihitting time,” the expected length of the shortest random walk from any one of the set of sequence-altered genes to an expression-altered target gene. -

ZMIZ1 Preferably Enhances the Transcriptional Activity of Androgen Receptor with Short Polyglutamine Tract
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central ZMIZ1 Preferably Enhances the Transcriptional Activity of Androgen Receptor with Short Polyglutamine Tract Xiaomeng Li1,2,3*, Chunfang Zhu1,2, William H. Tu1, Nanyang Yang3, Hui Qin3, Zijie Sun1,2* 1 Department of Urology, Stanford University School of Medicine, Stanford, California, United States of America, 2 Department of Genetics, Stanford University School of Medicine, Stanford, California, United States of America, 3 The Key Laboratory of Molecular Epigenetics of MOE, Institute of Genetics and Cytology, Northeast Normal University, Changchun, The People’s Republic of China Abstract The androgen receptor (AR) is a ligand-induced transcription factor and contains the polyglutamine (polyQ) tracts within its N-terminal transactivation domain. The length of polyQ tracts has been suggested to alter AR transcriptional activity in prostate cancer along with other endocrine and neurologic disorders. Here, we assessed the role of ZMIZ1, an AR co- activator, in regulating the activity of the AR with different lengths of polyQ tracts as ARQ9, ARQ24, and ARQ35 in prostate cancer cells. ZMIZ1, but not ZMIZ2 or ARA70, preferably augments ARQ9 induced androgen-dependent transcription on three different androgen-inducible promoter/reporter vectors. A strong protein-protein interaction between ZMIZ1 and ARQ9 proteins was shown by immunoprecipitation assays. In the presence of ZMIZ1, the N and C-terminal interaction of the ARQ9 was more pronounced than ARQ24 and ARQ35. Both Brg1 and BAF57, the components of SWI/SNF complexes, were shown to be involved in the enhancement of ZMIZ1 on AR activity. -

Ras Signaling Requires Dynamic Properties of Ets1 for Phosphorylation-Enhanced Binding to Coactivator CBP
Ras signaling requires dynamic properties of Ets1 for phosphorylation-enhanced binding to coactivator CBP Mary L. Nelsona,1, Hyun-Seo Kangb,1, Gregory M. Leeb, Adam G. Blaszczaka, Desmond K. W. Laub, Lawrence P. McIntoshb,2, and Barbara J. Gravesa,2 aDepartment of Oncological Sciences, University of Utah School of Medicine, Huntsman Cancer Institute, University of Utah, Salt Lake City, UT, 84112; and bDepartment of Biochemistry and Molecular Biology, Department of Chemistry, and the Michael Smith Laboratories, University of British Columbia, Vancouver, BC, Canada V6T 1Z3 Edited by Peter E. Wright, The Scripps Research Institute, La Jolla, CA, and approved April 8, 2010 (received for review January 4, 2010) Ras/MAPK signaling is often aberrantly activated in human can- Here we describe the coupled roles of the PNT domain and an cers. The downstream effectors are transcription factors, including adjacent disordered region bearing both Thr38 and a previously those encoded by the ETS gene family. Using cell-based assays and unrecognized phosphoacceptor, Ser41, in the ERK2-enhanced biophysical measurements, we have determined the mechanism by binding of the CBP TAZ1 domain by Ets1. Phosphorylation plays which Ras/MAPK signaling affects the function of Ets1 via phos- a dual role by altering a conformational equilibrium of a dynamic phorylation of Thr38 and Ser41. These ERK2 phosphoacceptors helix H0 that tethers the flexible phosphorylated region of Ets1 to lie within the unstructured N-terminal region of Ets1, immediately the core PNT domain and by augmenting electrostatic forces that adjacent to the PNT domain. NMR spectroscopic analyses demon- drive TAZ1 recognition. In this integrated model, structured ele- strated that the PNT domain is a four-helix bundle (H2–H5), resem- ments with intrinsic flexibility provide a scaffold for responsive- bling the SAM domain, appended with two additional helices ness to a signaling pathway. -
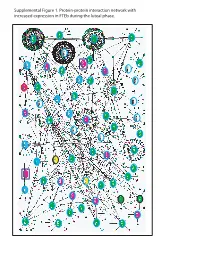
Supplemental Figure 1. Protein-Protein Interaction Network with Increased Expression in Fteb During the Luteal Phase
Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during luteal phase. LEGENDS TO SUPPLEMENTAL FIGURES Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with increased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. Genes encoding proteins shown as large ovals highlighted in blue were exclusively found in the first comparison (Manuscript Figure 2), whereas those highlighted in red were only found in the second comparison (Manuscript Figure 3). Genes encoding proteins shown as large ovals highlighted in black were found in both comparisons. The color of each node indicates the ontology of the corresponding protein as determined by the Online Predicted Human Interaction Database (OPHID) link with the NAViGaTOR software. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with decreased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. -

SPDEF (NM 001252294) Human Tagged ORF Clone Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for RG232468 SPDEF (NM_001252294) Human Tagged ORF Clone Product data: Product Type: Expression Plasmids Product Name: SPDEF (NM_001252294) Human Tagged ORF Clone Tag: TurboGFP Symbol: SPDEF Synonyms: bA375E1.3; PDEF Vector: pCMV6-AC-GFP (PS100010) E. coli Selection: Ampicillin (100 ug/mL) Cell Selection: Neomycin ORF Nucleotide >RG232468 representing NM_001252294 Sequence: Red=Cloning site Blue=ORF Green=Tags(s) TTTTGTAATACGACTCACTATAGGGCGGCCGGGAATTCGTCGACTGGATCCGGTACCGAGGAGATCTGCC GCCGCGATCGCC ATGGGCAGCGCCAGCCCGGGTCTGAGCAGCGTATCCCCCAGCCACCTCCTGCTGCCCCCCGACACGGTGT CGCGGACAGGCTTGGAGAAGGCGGCAGCGGGGGCAGTGGGTCTCGAGAGACGGGACTGGAGTCCCAGTCC ACCCGCCACGCCCGAGCAGGGCCTGTCCGCCTTCTACCTCTCCTACTTTGACATGCTGTACCCTGAGGAC AGCAGCTGGGCAGCCAAGGCCCCTGGGGCCAGCAGTCGGGAGGAGCCACCTGAGGAGCCTGAGCAGTGCC CGGTCATTGACAGCCAAGCCCCAGCGGGCAGCCTGGACTTGGTGCCCGGCGGGCTGACCTTGGAGGAGCA CTCGCTGGAGCAGGTGCAGTCCATGGTGGTGGGCGAAGTGCTCAAGGACATCGAGACGGCCTGCAAGCTG CTCAACATCACCGCAGATCCCATGGACTGGAGCCCCAGCAATGTGCAGAAGTGGCTCCTGTGGACAGAGC ACCAATACCGGCTGCCCCCCATGGGCAAGGCCTTCCAGGAGCTGGCGGGCAAGGAGCTGTGCGCCATGTC GGAGGAGCAGTTCCGCCAGCGCTCGCCCCTGGGTGGGGATGTGCTGCACGCCCACCTGGACATCTGGAAG TCAGCCTCGACCAGTGAGGAGAGCTGGACCGACAGCGAGGTGGACTCATCATGCTCCGGGCAGCCCATCC ACCTGTGGCAGTTCCTCAAGGAGTTGCTACTCAAGCCCCACAGCTATGGCCGCTTCATTAGGTGGCTCAA CAAGGAGAAGGGCATCTTCAAAATTGAGGACTCAGCCCAGGTGGCCCGGCTGTGGGGCATCCGCAAGAAC CGTCCCGCCATGAACTACGACAAGCTGAGCCGCTCCATCCGCCAGTATTACAAGAAGGGCATCATCCGGA -

Combinatorial Targeting of the Androgen Receptor for Prostate
Combinatorial Targeting of the Androgen Receptor for Prostate Cancer Therapy A thesis submitted to the University of Adelaide in the fulfilment of the requirements for the degree of Doctor of Philosophy By Sarah Louise Carter B.BiomolChem.(Hons) Dame Roma Mitchell Cancer Research Laboratories School of Medicine The University of Adelaide and The Hanson Institute March 2015 Contents Chapter 1: General Introduction ........................................................................................1 1.1 Background ..................................................................................................................2 1.2 Androgens and the Prostate ..........................................................................................3 1.3 Androgen Signalling through the Androgen Receptor .................................................4 1.3.1 The androgen receptor (AR) ..................................................................................4 1.3.2 Androgen signalling in the prostate .......................................................................6 1.4 Current Treatment Strategies for Prostate Cancer ........................................................8 1.4.1 Diagnosis ...............................................................................................................8 1.4.2 Localised disease .................................................................................................10 1.4.3 Relapse and metastatic disease ............................................................................13