Supporting Document Document 1 of CCHD Screening to Reduce
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Somrat Vol. 11 No. 1 Page 21-32.Pmd
Asian Biomedicine Vol. 11 No. 1 February 2017; 21 - 32 DOI: 10.5372/1905-7415.1101.535 Original article Perioperative and Anesthetic Adverse events in Thailand (PAAd Thai) incident reporting study: anesthetic profiles and outcomes Somrat Charuluxananan1, Wimonrat Sriraj2, Yodying Punjasawadwong3, Siriporn Pitimana-aree4, Varinee Lekprasert5, Thewarug Werawatganon1, Wirat Wasinwong6, Prapa Ratanachai7, Dujduen Sriramatr8, Sunida Atichat9, Wanna Angkasuvan7, Chuthamat Somchat10, Duangporn Tanutanud11, Thidarat Ariyanuchitkul12, Jaroonpong Choorat13, Krairerk Sintavanuruk14, Jeratkana Janngam15 1Department of Anesthesiology, Faculty of Medicine, Chulalongkorn University, Bangkok 10330, Thailand 2Department of Anesthesiology, Faculty of Medicine, Khon Kaen University, Khon Kaen 40000, Thailand 3Department of Anesthesiology, Faculty of Medicine, Chiang Mai University, Chiang Mai 50200, Thailand 4Department of Anesthesiology, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand 5Department of Anesthesiology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok 10400, Thailand 6Department of Anesthesiology, Faculty of Medicine, Prince of Songkla University, Songkhla 90110, Thailand 7Department of Anesthesiology, Hatyai Hospital, Songkhla 90110, Thailand 8Department of Anesthesiology, Faculty of Medicine, Srinakharinwirot University, Nakhon Nayok 26120, Thailand 9Department of Anesthesiology, Chonburi Regional Hospital, Chonburi 20000, Thailand 10Department of Anesthesiology, Lamphun Hospital, Lamphun -

HIS in Thailand Never Ending Stories Thai Health Information System: of the Development of an Effective Situation and Challenges HIS in Thailand Dr
Never ending stories of the development of an effective HIS in Thailand Never ending stories Thai Health Information System: of the development of an effective Situation and challenges HIS in Thailand Dr. Pinij Faramnuayphal Supported by : Prince Mahidol Award Foundation under the Royal Patronage Ministry of Public Health World Health Organization The World Health Organization (WHO) identifies fully functional health Mahidol University information system as one of the six important building blocks of high Health Systems Research Institute performing health system. A well-functioning health information system (HIS) is one that ensures the production, analysis, dissemination and Published by: use of reliable and timely information on health determinants, health system performance and health status. All of these components Health Systems Research Institute (HSRI) contribute to a better health policy and planning, health resources allocation, health service delivery and finally, health outcome. With the cooperation of : The importance of health information system is crucial and is Ang Thong Provincial Health Office recognized that countries cannot build a good health system without Bangkok Hospital Group Medical Center it. Strengthening health information system, therefore, has become Bang Phae Hospital one of the most important issues worldwide in a recent decade. Bumrungrad Hospital Public Company Limited The demand on measuring the Millennium Development Goals is National Health Security office an example of the explicit requirements of -
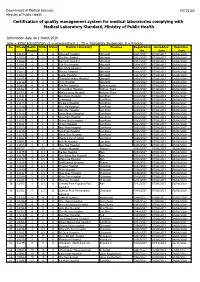
Certification of Quality Management System for Medical Laboratories Complying with Medical Laboratory Standard, Ministry of Public Health
Department of Medical Sciences F0715102 Ministry of Public Health Certification of quality management system for medical laboratories complying with Medical Laboratory Standard, Ministry of Public Health Information date on 1 March 2019 new = initial accreditation, r1 = reassessment 1 , TS = Temporary Suspension, P = Process No. HCode Health RMSc Status Medical Laboratory Province Registration Accredited Expiration Region No. Date Date 1 10673 2 2 r1 Uttaradit Hospital Uttaradit 0001/2557 07/08/2017 06/08/2020 2 11159 2 2 r1 Tha Pla Hospital Uttaradit 0002/2557 07/08/2017 06/08/2020 3 11160 2 2 r1 Nam Pat Hospital Uttaradit 0003/2557 07/08/2017 06/08/2020 4 11161 2 2 r1 Fak Tha Hospital Uttaradit 0004/2557 07/08/2017 06/08/2020 5 11162 2 2 r1 Ban Khok Hospital Uttaradit 0005/2557 07/08/2017 06/08/2020 6 11163 2 2 r1 Phichai Hospital Uttaradit 0006/2557 07/08/2017 06/08/2020 7 11164 2 2 r1 Laplae Hospital Uttaradit 0007/2557 07/08/2017 06/08/2020 8 11165 2 2 r1 ThongSaenKhan Hospital Uttaradit 0008/2557 07/08/2017 06/08/2020 9 11158 2 2 r1 Tron Hospital Uttaradit 0009/2557 07/08/2017 06/08/2020 10 10863 4 4 r1 Pak Phli Hospital Nakhonnayok 0010/2557 07/08/2017 06/08/2020 11 10762 4 4 r1 Thanyaburi Hospital Pathum Thani 0011/2557 07/08/2017 06/08/2020 12 10761 4 4 r1 Klong Luang Hospital Pathum Thani 0012/2557 07/08/2017 06/08/2020 13 11141 1 1 P Ban Hong Hospital LamPhun 0014/2557 07/08/2014 06/08/2017 14 11142 1 1 P Li Hospital LamPhun 0015/2557 07/08/2014 06/08/2017 15 11144 1 1 P Pa Sang Hospital LamPhun 0016/2557 07/08/2014 06/08/2017 -

Bangkok Anesthesia Regional Training Center
RoleRole ofof BARTCBARTC (Bangkok(Bangkok AnesthesiaAnesthesia RegionalRegional TrainingTraining Center)Center) IInn cooperationcooperation inin educationeducation andand trainingtraining inin developingdeveloping countriescountries ProfProf TharaThara TritrakarnTritrakarn DirectorDirector ofof BARTCBARTC 14th WCA, Cape Town, South Africa, 3/1/2008 Oslo Center, Norway, 12/1/2008 ShortageShortage ofof anesthesiologistsanesthesiologists AA worldwideworldwide problemsproblems MoreMore seriousserious inin developingdeveloping poorpoor countriescountries MarkedMarked variationvariation amongamong countriescountries EconomyEconomy - Most important determining factors - Three levels of wealth & health - Rich countries (per capita GNP > $ 10,000) - Medium to low (GNP $ 1,000-10,000) - Poor countries (GNP < $ 1,000) RichRich && MediumMedium countriescountries GNPGNP PeoplePeople NumberNumber PeoplePeople perper capitacapita perper ofof perper (US(US $)$) doctordoctor anesthetistsanesthetists anesthetistanesthetist USA 33,799 387 23,300 11,500 Japan 34,715 522 4,229 20,000 Singapore 22,710 667 150 26,600 Hong Kong 23,597 772 150 40,000 Australia 19,313 2170 10,000 Malaysia 3,248 1,477 250 88,000 Thailand 1,949 2,461 500 124,000 Philippines 1,048 1,016 1176 64,600 MediumMedium && PoorPoor CountriesCountries GNPGNP PeoplePeople NumberNumber PeoplePeople perper capitacapita perper ofof perper (US(US $)$) doctordoctor anesthetistsanesthetists anesthetistanesthetist Indonesia 617 6,7866,786 350 591,000591,000 Pakistan 492 2,0002,000 400 340,000340,000 -

Cover Tjs 35-4-57
ISSN 0125-6068 TheThai Journal of SURGERY Official Publication of the Royal College of Surgeons of Thailand www.surgeons.or.th/ejournal Volume 35 October-December 2014 Number 4 ORIGINAL ARTICLES 121 Comparison between Ventriculoatrial Shunt and Ventriculoperitoneal Shunt: Revision Rate and Complications Korrapakc Wangtanaphat, Porn Narischart 126 Open Surgical Management of Atherosclerotic Aortoiliac Occlusive Diseases (AIOD) Type 1 Anuwat Chantip 130 “Sawanpracharak” Connector: A Single Tube Intercostal Drainage Connector Wanchai Manakijsirisuthi 134 The Trainee’s Operative Experiences for General Surgery in Thailand Potchavit Aphinives CASE REPORT 139 Mitral and Tricuspid Valve Replacement in Uncommon Case of Situs Inversus with Dextrocardia Nuttapon Arayawudhikul, Boonsap Sakboon, Jareon Cheewinmethasiri, Angsu Chartirungsun, Benjamaporn Sripisuttrakul ABSTRACTS 143 Abstracts of the 39th Annual Scientific Congress of the Royal College of Surgeons of Thailand, 10-13 July 2014, Ambassador City Jomtien Hotel, Jomtien, Pattaya, Cholburi, Thailand (Part II) 169 Index Secretariat Office : Royal Golden Jubilee Building, 2 Soi Soonvijai, New Petchaburi Road, Huaykwang, Bangkok 10310, Thailand Tel. +66 2716 6141-3 Fax +66 2716 6144 E-mail: [email protected] www.surgeons.or.th The THAI Journal of SURGERY Official Publication of the Royal College of Surgeons of Thailand Vol. 35 October - December 2014 No. 4 Original Article Comparison between Ventriculoatrial Shunt and Ventriculoperitoneal Shunt: Revision Rate and Complications Korrapakc Wangtanaphat, MD Porn Narischart, MD Prasat Neurological Institute, Department of Medical Services, Ministry of Pubic Health, Bangkok, Thailand Abstract Background and Objective: Hydrocephalus is a common problem in neurosurgical field. In current clinical practice guidelines, ventriculoatrial shunt and ventriculoperitoneal shunt are recommended treatment options. No previous study reported differences between two procedures in term of complications and revision rates. -

January 08-11 Pp01
ANDAMAN Edition Volume 18 Issue 2 January 8 - 14, 2011 Daily news at www.phuketgazette.net 25 Baht Booze ban hits park tourists Teen stabbing sparks alcohol ban in national parks By Atchaa Khamlo derstand and have given us very Standard procedure is for staff good co-operation. The situation to ask people trying to bring alco- THE directors of several national is under control,” he said. hol into the park to leave it with parks in the Andaman region say Most of those warned about officers during their visit, he said. they have received good compli- drinking in the park were Thais, “We prefer to ask people for ance with the ban on alcohol in- but a few were foreigners. their co-operation rather than side parks that came into effect “As the park is quite expansive, threaten them with punishment. It on December 27. sometimes people might be drink- seems our public relations cam- Natural Resources and Envi- ing inside without our being aware paign is going well, as most people ronment Minister Suwit Khunkitti of it,” he added. just drink Coke or water,” he said. issued the ban immediately follow- Two signs declaring the park “Most foreigners understand ing the December 26 stabbing an alcohol prohibition zone are quite well. Not many of them drink murder of a student by a group of now being constructed and should whiskey, but some like to drink drunken schoolmates camping at go up at both entrances very soon, beer. But they don’t seem to have Khao Yai National Park in Surat along with a third sign to go up in any problem with alcohol being Thani. -

Economic Burden of Hospitalization with Acute Wheezing in Preschool Children: a Multi-Center Study
Economic Burden of Hospitalization with Acute Wheezing in Preschool Children: A Multi-Center Study Paskorn Sritipsukho MD*,**, Khlongtip Matchimmadamrong MD***, Sasawan Chinratanapisit MD****, Jitladda Deerojanawong MD***** * Center of Excellence in Applied Epidemiology, Thammasat University, Pathumthani, Thailand ** Division of Allergy, Department of Pediatrics, Faculty of Medicine, Thammasat University, Pathumthani, Thailand *** Department of Pediatrics, Saraburi Hospital, Saraburi, Thailand **** Department of Pediatrics, Bhumibol Adulyadej Hospital, Bangkok, Thailand ***** Division of Respiratory disease and intensive care, Department of Pediatrics, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand Background: Wheezing is an important health problem in Thailand especially among preschool age. Objective: The aim of this study was to estimate costs of wheezing for hospitalization in preschool children under patient, provider, and societal perspectives. Material and Method: Two hundred and thirty-four participants who were admitted with acute wheezing at 4 hospitals including Thammasat University Hospital, Saraburi Hospital, Bhumibol Adulyadej Hospital and King Chulalongkorn Memorial Hospital during July 2014 to June 2015 were included in the present study. Data from hospital financial database and caregivers’ expenses were collected. Cost-to-charge ratio method was employed for valuation of direct medical costs. Informal care costs were determined by human capital approach. Results: The means of patient, provider and societal costs per admission were 3,020 THB (SD = 6,632 THB), 18,126 THB (SD = 16,898 THB), and 20,269 THB (SD = 20,537 THB) respectively. The main cost component in provider and societal perspective were accommodation costs during admission. Informal care cost was a major cost component for direct non- medical costs. The economic burden of acute wheezing admission of preschool children in Thailand was estimated as 759 million THB per year. -

Resistance Patterns Selected by Nevirapine Vs
Resistance Patterns Selected by Nevirapine vs. Efavirenz in HIV-Infected Patients Failing First-Line Antiretroviral Treatment: A Bayesian Analysis Nicole Ngo-Giang-Huong1,2,3*, Gonzague Jourdain1,2,3, Billy Amzal1,2, Pensiriwan Sang-a-gad4, Rittha Lertkoonalak5, Naree Eiamsirikit6, Somboon Tansuphasawasdikul7, Yuwadee Buranawanitchakorn8, Naruepon Yutthakasemsunt9, Sripetcharat Mekviwattanawong10, Kenneth McIntosh3,11, Marc Lallemant1,2,3, for the Program for HIV Prevention and Treatment (PHPT) study group" 1 Institut de Recherche pour le De´veloppement (IRD) UMI 174 - PHPT, Marseilles, France, 2 Department of Medical Technology, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand, 3 Department of Immunology and Infectious Diseases, Harvard School of Public Health, Boston, Massachusetts, United States of America, 4 Ratchaburi Hospital, Ratchaburi, Thailand, 5 Maharat Nakonratchasima Hospital, Nakonratchasima, Thailand, 6 Samutprakarn Hospital, Samutprakarn, Thailand, 7 Buddhachinaraj Hospital, Pitsanuloke, Thailand, 8 Chiang Kham Hospital, Chiang Kham, Thailand, 9 Nong Khai Hospital, Nong Khai, Thailand, 10 Pranangklao Hospital, Bangkok, Thailand, 11 Division of Infectious Diseases, Children’s Hospital, Boston, Massachusetts, United States of America Abstract Background: WHO recommends starting therapy with a non-nucleoside reverse transcriptase inhibitor (NNRTI) and two nucleoside reverse transcriptase inhibitors (NRTIs), i.e. nevirapine or efavirenz, with lamivudine or emtricitabine, plus zidovudine or -

วารสาร พยาบาลสาร Nursing Journal ปีที่ 47 ฉบับที่ 1 มกราคม-มีนาคม พ.ศ
พยาบาลสาร : Nursing Journal คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ วารสาร พยาบาลสาร Nursing Journal ปีที่ 47 ฉบับที่ 1 มกราคม-มีนาคม พ.ศ. 2563 • Volume 47 No.1 January-March 2020 ISSN 0125-5118 ที่ปรึกษา (Consultant) ศาสตราจารย์ ดร.วิภาดา คุณาวิกติกุล คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ Wipada Kunaviktikul, PhD, RN, FAAN Faculty of Nursing, Chiang Mai University ผู้ช่วยศาสตราจารย์ ดร.จุฑารัตน์ มีสุขโข คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ Jutarat Mesukko, PhD, RN Faculty of Nursing, Chiang Mai University ที่ปรึกษากองบรรณาธิการ (Editorial Advisors) ศาสตราจารย์เกียรติคุณ ดร.วิจิตร ศรีสุพรรณ อดีตนายกสภาการพยาบาล Wichit Srisuphan, DrPH, RN Professor ศาสตราจารย์ ดร.ประนอม โอทกานนท์ ศาสตราจารย์ Pranom Othagnont, RN, M.E.D.,Ed.D. Professor ศาสตราจารย์ ดร.สมจิต หนุเจริญกุล ศาสตราจารย์ Somchit Hanucharurnkul, PhD, RN Professo บรรณาธิการ (Editor) ศาสตราจารย์ ดร. อารีวรรณ กลั่นกลิ่น คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ Areewan Klunklin, PhD, RN Faculty of Nursing, Chiang Mai University รองบรรณาธิการ (Associate Editor) รองศาสตราจารย์ ดร.นันทพร แสนศิริพันธ์ คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ Nantaporn Sansiriphun, PhD, RN, APN Faculty of Nursing, Chiang Mai University กองบรรณาธิการ (Editorial Board) ศาสตราจารย์ ดร.รุจา ภู่ไพบูลย์ คณะพยาบาลศาสตร์ มหาวิทยาลัยมหิดลศาสตราจารย์ Rutja Phuphaibul, DNS, RN Faculty of Nursing, Mahidol University ศาสตราจารย์ ดร.วีณา จีระแพทย์ คณะพยาบาลศาสตร์ จุฬาลงกรณ์มหาวิทยาลัย Veena Jirapaet, PhD, RN Faculty of Nursing, Chulalongkorn University ศาสตราจารย์ ดร.วารุณี ฟองแก้ว คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ Warunee Fongkaew, -

Blood Group Genomics
BLOOD GROUP GENOMICS Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry analysis of 36 blood group alleles among 396 Thai samples reveals region-specific variants Philaiphon Jongruamklang,1 Christoph Gassner,2 Stefan Meyer,2 Aksarakorn Kummasook,3 Marion Darlison,1 Chayanun Boonlum,4 Surin Chanta,5 Beat M. Frey,2 Martin L. Olsson,1,6* and Jill R. Storry 1,6* lood group antigen polymorphism shows great BACKGROUND: Blood group phenotype variation has variation in different world populations. The been attributed to potential resistance to pathogen reason for this is not completely understood; invasion. Variation was mapped in blood donors from however, it has been attributed to both Lampang (northern region) and Saraburi (central region), B Thailand, where malaria is endemic. The previously unknown blood group allele profiles were characterized ABBREVIATIONS: MALDI-TOF MS 5 matrix-assisted laser and the data were correlated with phenotypes. The high desorption/ionization time-of-flight mass spectrometry; PCR- incidence of the Vel-negative phenotype previously ASP 5 polymerase chain reaction with allele-specific reported in Thais was investigated. primers; SNP(s) 5 single nucleotide polymorphism(s). STUDY DESIGN AND METHODS: DNA from 396 From 1Hematology and Transfusion Medicine, Department of blood donors was analyzed by matrix-assisted laser Laboratory Medicine, Lund University, Lund, Sweden; desorption/ionization–time-of-flight mass spectrometry. 2Molecular Diagnostics & Research (MOC), Blood Transfusion Outliers were investigated by serology and DNA Service Zurich,€ Zurich-Schlieren,€ Switzerland; 3Department of sequencing. Allele discrimination assays for SMIM1 Medical Technology, School of Allied Health Sciences, rs1175550A/G and ACKR1 rs118062001C/T were University of Phayao, Phayao, Thailand; 4Transfusion Medicine, performed and correlated with antigen expression. -

Aw-Poster-Pongsak Pirom-0629
Poster #0629 HEPATITIS B VIRUS DNA LEVEL CHANGES IN HBeAg+ PREGNANT WOMEN RECEIVING TDF FOR PREVENTION OF MOTHER-TO-CHILD TRANSMISSION IRD-CMU PHPT CROIConference on Retroviruses Nicole Ngo-Giang-Huong1, Nicolas Salvadori2, Woottichai Khamduang2, Tim R. Cressey2, Linda J. Harrison3, Luc Decker1, Camlin Tierney3, Jullapong Achalapong4, and Opportunistic Infections Trudy V. Murphy5, Noele Nelson5, George K. Siberry6, Raymond T. Chung7, Stanislas Pol8, Gonzague Jourdain1, for the iTAP study group 1IRD, Chiang Mai, Thailand, 2Chiang Mai University, Chiang Mai, Thailand, 3Harvard University, Boston, MA, USA, 4Chiangrai Prachanukroh Hospital, Chiang Rai, Thailand, 5CDC, Atlanta, GA, USA, 6USAID, Arlington, VA, USA, 7Massachusetts General Hospital, Boston, MA, USA, 8Cochin Hospital, Paris, France Background HBV DNA load measurements • 12% (19 of 161) did not achieve 5.3 log10 IU/ml at delivery; References • Population: all women assigned to the TDF arm + a randomly the median (range) HBV DNA for these women was 8.3 • High hepatitis B virus (HBV) DNA levels and positive hepatitis (7.1 to 9.1) log IU/mL at baseline, 7.4 (4.7 to 8.6) at • Sarin SK, Kumar M, Lau GK, et al. Asian-Pacific clinical practice guidelines on selected subset of 50 women assigned to the placebo arm 10 B e antigen (HBeAg-an indicator of rapid viral replication and 32-weeks, 7.0 (3.9 to 8.5) at 36 weeks and 7.8 (5.3 to 8.9) the management of hepatitis B: a 2015 update. Hepatol Int 2016;10:1-98. • European Association for the Study of the Liver. Electronic address eee, high level of HBV DNA) are the main markers of risk for • Timing: at baseline (28 weeks gestation), at Weeks 32 and at delivery. -

Clinical Epidemiology of 7126 Melioidosis Patients in Thailand and the Implications for a National Notifiable Diseases Surveilla
applyparastyle “fig//caption/p[1]” parastyle “FigCapt” View metadata, citation and similar papers at core.ac.uk brought to you by CORE Open Forum Infectious Diseases provided by Apollo MAJOR ARTICLE Clinical Epidemiology of 7126 Melioidosis Patients in Thailand and the Implications for a National Notifiable Diseases Surveillance System Viriya Hantrakun,1, Somkid Kongyu,2 Preeyarach Klaytong,1 Sittikorn Rongsumlee,1 Nicholas P. J. Day,1,3 Sharon J. Peacock,4 Soawapak Hinjoy,2,5 and Direk Limmathurotsakul1,3,6, 1Mahidol-Oxford Tropical Medicine Research Unit (MORU), Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand, 2 Epidemiology Division, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand, 3 Centre for Tropical Medicine and Global Health, Nuffield Department of Clinical Medicine, Old Road Campus, University of Oxford, Oxford, United Kingdom, 4 Department of Medicine, University of Cambridge, Cambridge, United Kingdom, 5 Office of International Cooperation, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand, and 6 Department of Tropical Hygiene, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand Background. National notifiable diseases surveillance system (NNDSS) data in developing countries are usually incomplete, yet the total number of fatal cases reported is commonly used in national priority-setting. Melioidosis, an infectious disease caused by Burkholderia pseudomallei, is largely underrecognized by policy-makers due to the underreporting of fatal cases via the NNDSS. Methods. Collaborating with the Epidemiology Division (ED), Ministry of Public Health (MoPH), we conducted a retrospec- tive study to determine the incidence and mortality of melioidosis cases already identified by clinical microbiology laboratories nationwide. A case of melioidosis was defined as a patient with any clinical specimen culture positive for B.