A Case of Cushing Syndrome with Both Secondary Hypothyroidism and Hypercalcemia Due to Postoperative Adrenal Insufficiency
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Hyperthyroidism with an FSH- and TSH-Secreting Pituitary Adenoma
• Hyperthyroidism with an FSH- and TSH-secreting pituitary adenoma JOHN BERMINGHAM, DO LOUIS C. HAENEL, DO A 34-year-old man was found noma is rare. The combined secretion of follicle- to have elevated thyroxine (T 4 ), triiodothy- stimulating hormone (FSH) and TSH by a pi- ronine (T3 ), calculated free T4 , thyroid- tuitary adenoma is rarer. But with current stimulating hormone (TSH), follicle-stimu- widespread use of TSH assays, plus the future lating hormone (FSH), and alpha subunits clinical availability of more sensitive TSH as- of TSH and FSH. A computed tomography says as well as TSH bioactivity testing, more scan of the head showed a 16-mm mac- patients will have pituitary-induced hyperthy- roadenoma of the pituitary gland. There roidism correctly diagnosed, and the disorder was no evidence of loss or excess secre- will be better understood. tion of other pituitary hormones. The large As illustrated in the following case study, chromophobe adenoma was removed via making the correct diagnosis of primary ver- a transphenoidal approach. The patient sus secondary hyperthyroidism is imperative has been taken off all medication. Thyroid because the treatment and potential conse- function has returned to normal and there quences of each of these diseases are totally has been no loss of pituitary secretory ca- different. pacity of other pituitary hormones. The oc- currence of a combined TSH- and FSH- Report of case secreting pituitary adenoma is rare; to the In August 1985, a 34-year-old man was seen with authors knowledge, only one case has complaints that were initially vague and nonspe- been documented in the literature. -

Drugs for the Treatment of Hypercalcaemia C. R. PATERSON
Postgrad Med J: first published as 10.1136/pgmj.50.581.158 on 1 March 1974. Downloaded from Postgraduate Medical Journal (March 1974) 50, 158-162. Drugs for the treatment of hypercalcaemia C. R. PATERSON M.A., D.M., M.R.C.PATH. Department of Clinical Chemistry, University of Dundee, Dundee Summary able commercially (Phosphate Sandoz). The initial Hypercalcaemia is ordinarily treated by treatment of dose is 1-3 g (of phosphorus) per day according to the underlying disorder. In some cases, as in malignant the size of the patient. The serum calcium should be disease, in vitamin D poisoning and after a failed checked daily at first and the dose adjusted appro- parathyroidectomy, the hypercalcaemia itself needs to priately so that the maintenace dose is the minimum be treated. A large number of methods have been consistent with control of the serum calcium. Oral advocated for this, but phosphate is the drug of choice phosphate therapy is effective in the management of in most patients. This paper outlines its use, mode of hypercalcaemia of malignant disease and myeloma action and side effects and reviews the other methods (Goldsmith and Ingbar, 1966; Goldsmith et al., proposed for the management of hypercalcaemia. 1968; Thalassinos and Joplin, 1968), in hyperpara- thyroidism (Dent, 1962; Goldsmith and Ingbar, 1966; Eisenberg, 1968), and in vitamin D poisoningProtected by copyright. Introduction (Goldsmith and Ingbar, 1966). The management of hypercalcaemia is ordinarily Intravenous phosphate therapy is used in the that of the underlying disorder (Wills, 1971; management of acute hypercalcaemia, especially in Henrard, 1971; Watson, 1972). There are, however, the patient who is vomiting or in coma. -

PARANEOPLASTIC SYNDROMES: J Neurol Neurosurg Psychiatry: First Published As 10.1136/Jnnp.2004.040378 on 14 May 2004
PARANEOPLASTIC SYNDROMES: J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2004.040378 on 14 May 2004. Downloaded from WHEN TO SUSPECT, HOW TO CONFIRM, AND HOW TO MANAGE ii43 J H Rees J Neurol Neurosurg Psychiatry 2004;75(Suppl II):ii43–ii50. doi: 10.1136/jnnp.2004.040378 eurological manifestations of cancer are common, disabling, and often multifactorial (table 1). The concept that malignant disease can cause damage to the nervous system Nabove and beyond that caused by direct or metastatic infiltration is familiar to all clinicians looking after cancer patients. These ‘‘remote effects’’ or paraneoplastic manifestations of cancer include metabolic and endocrine syndromes such as hypercalcaemia, and the syndrome of inappropriate ADH (antidiuretic hormone) secretion. Paraneoplastic neurological disorders (PNDs) are remote effects of systemic malignancies that affect the nervous system. The term PND is reserved for those disorders that are caused by an autoimmune response directed against antigens common to the tumour and nerve cells. PNDs are much less common than direct, metastatic, and treatment related complications of cancer, but are nevertheless important because they cause severe neurological morbidity and mortality and frequently present to the neurologist in a patient without a known malignancy. Because of the relative rarity of PND, neurological dysfunction should only be regarded as paraneoplastic if a particular neoplasm associates with a remote but specific effect on the nervous system more frequently than would be expected by chance. For example, subacute cerebellar ataxia in the setting of ovarian cancer is sufficiently characteristic to be called paraneoplastic cerebellar degeneration, as long as other causes have been ruled out. -

Clinical Research Protocol
CLINICAL RESEARCH PROTOCOL NCT02399475 The Thyroid Axis in Older Individuals with Persistent Subclinical Hypothyroidism: a Mechanistic, Randomized, Double-Blind, Cross-Over Study of Levothyroxine and Liothyronine Administration Regulatory Sponsor: Anne R. Cappola, MD, ScM Division of Endocrinology, Diabetes, and Metabolism 12-136 Translational Research Center 3400 Civic Center Blvd, Bldg 421 Philadelphia, PA 19104-5160 (215) 573 5359 Funding Sponsor: National Institute on Aging, NIH Medications Used: Thyrotropin Releasing Hormone (TRH) Levothyroxine (LT4) Liothyronine (LT3) Protocol Number: 821564 IND Number: 125167 Initial version:[11/26/2014] Amended [7/22/2015] Amended: [12/18/2014] Amended [9/9/2015] Amended: [1/2/2015] Amended [8/25/2016] Amended: [3/26/2015] Amended [12/23/2016] Amended: [5/13/2015] Amended [3/24/2017] Amended: [06/04/2015] Amended [9/26/2017] Amended: [6/10/2015] Amended [12/18/2017] (additional next page) Amended [12/18/18] CONFIDENTIAL This material is the property of the University of Pennsylvania. Do not disclose or use except as authorized in writing by the study sponsor LT4 and LT3 in Subclinical Hypothyroidism Page ii Version 12/18/2018 Table of Contents STUDY SUMMARY ......................................................................................................... 1 1 INTRODUCTION ...................................................................................................... 3 1.1 BACKGROUND .................................................................................................... -

Paraneoplastic Syndromes in Patients with Ovarian Neoplasia
202 Journal of the Royal Society of Medicine Volume 86 April 1993 Paraneoplastic syndromes in patients with ovarian neoplasia C N Hudson MChir FRCS FRCOG1 Marigold Curling MB BS2 Penelope Potsides' D G Lowe MD MRCPath MIBiol' 'The Association of Obstetricians and Gynaecologists, NE Thames Region and 2the Department ofHistopathology, St Bartholomew's Hospital Medical College, London EClA 7BE Keywords: paraneoplastic syndromes; ovarian cancer; prevalence Summary data at presentation of 908 patients with primary The prevalence of several paraneoplastic syndromes epithelial ovarian cancer, collected prospectively in associated with ovarian cancer was determined from the North East Thames Region. a clinicopathological study of 908 patients with primary ovarian malignancy in the North East Thames Data source Region. The diversity and rarity of these manifesta- In the 1970s a data bank for ovarian cancer in the tions are great and the explanation for them is North East Metropolitan Region was set up by difficult. Circumstantial evidence suggests that in the Association of Obstetricians and Gynaecologists some cases an autoimmune phenomenon is the most of the Region in association with the Regional plausible cause. Histopathologists Group. Data was entered either by pathologist or clinician, and as soon as a case Introduction was notified, the clinical data on an agreed proforma Paraneoplastic syndromes are systemic manifestations were obtained from the surgeon concerned - he/ ofcancer that cannot readily be explained by the local she provided details of the mode of presentation, or metastatic effects of a tumour or of hormones investigation, operative staging, and treatment. indigenous to the tissue in which the tumour arises. Histological material was reviewed centrally by The syndromes fall into four broad groups, in which the two of the authors. -
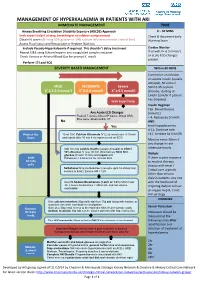
Management of Hyperkalaemia in Patients with Aki Immediate Management Time
MANAGEMENT OF HYPERKALAEMIA IN PATIENTS WITH AKI IMMEDIATE MANAGEMENT TIME ≥ Airway Breathing Circulation Disability Exposure (ABCDE) Approach 0 – 30 MINS Seek expert help if airway, breathing or circulation compromised Check & document Early Obtain IV access (If using 50% glucose or 10% calcium infusions consider central line) Warning Score Assess Fluid status and Resuscitate or Replace fluid loss Exclude Pseudo-Hyperkalaemia if required. This shouldn’t delay treatment Cardiac Monitor Repeat U&E using lithium heparin anti-coagulated sample container If unwell, K+ 6.5 mmol/L + or acute ECG changes Check Venous or Arterial Blood Gas for prompt K result P present Perform 12 Lead ECG SEVERITY BASED MANAGEMENT Within 60 MINS Commence an infusion of soluble insulin (usually actrapid), 50 units in MILD MODERATE Severe 50ml 0.9% sodium + + + K 5.5-5.9 mmol/l K 6-6.4 mmol/l K ≥ 6.5 mmol/l chloride, starting at 1ml/hr (2ml/hr if patient has diabetes) Seek Expert help Insulin Regimen Cap. Blood Glucose Any Acute ECG Changes (mmol/L) Peaked T waves, Absent P waves, Broad QRS, < 4: Reduce by 0.5ml/h Sine wave, Bradycardia, VT No AND Yes treat hypoglycaemia 4-11: Continue rate Protect the 10 ml 10% Calcium Gluconate IV (2.26 mmol) over 5-10 min >11: Increase by 0.5ml/h Heart and repeat after 10 min if no improvement on ECG Monitor every 30min if any change in rate Add 10 units soluble Insulin (usually Actrapid) to 250ml otherwise hourly 10% Glucose IV over 30 min (Alternatively 50ml 50% glucose IV over 15 min) and repeat until Dialysis Shift Potassium < 5.5mmol/L for at least 4hrs. -

Kaplan & Sadock's Study Guide and Self Examination Review In
Kaplan & Sadock’s Study Guide and Self Examination Review in Psychiatry 8th Edition ← ↑ → © 2007 Lippincott Williams & Wilkins Philadelphia 530 Walnut Street, Philadelphia, PA 19106 USA, LWW.com 978-0-7817-8043-8 © 2007 by LIPPINCOTT WILLIAMS & WILKINS, a WOLTERS KLUWER BUSINESS 530 Walnut Street, Philadelphia, PA 19106 USA, LWW.com “Kaplan Sadock Psychiatry” with the pyramid logo is a trademark of Lippincott Williams & Wilkins. All rights reserved. This book is protected by copyright. No part of this book may be reproduced in any form or by any means, including photocopying, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appearing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. Printed in the USA Library of Congress Cataloging-in-Publication Data Sadock, Benjamin J., 1933– Kaplan & Sadock’s study guide and self-examination review in psychiatry / Benjamin James Sadock, Virginia Alcott Sadock. —8th ed. p. cm. Includes bibliographical references and index. ISBN 978-0-7817-8043-8 (alk. paper) 1. Psychiatry—Examinations—Study guides. 2. Psychiatry—Examinations, questions, etc. I. Sadock, Virginia A. II. Title. III. Title: Kaplan and Sadock’s study guide and self-examination review in psychiatry. IV. Title: Study guide and self-examination review in psychiatry. RC454.K36 2007 616.890076—dc22 2007010764 Care has been taken to confirm the accuracy of the information presented and to describe generally accepted practices. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this book and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. -
Paraneoplastic Hypercalcaemia Associated with TCC of Bladder
Case Study TheScientificWorldJOURNAL (2004) 4, 1069–1070 ISSN 1537-744X; DOI 10.1100/tsw.2004.187 Paraneoplastic Hypercalcaemia Associated with TCC of Bladder A.B. Patel1,*, L. Wilson2, C. Blick2, and P. Meffan2 1Institute of Urology and Nephrology, UCL Medical School, Charles Bell House, 67 Riding House Street, London; 2Department of Urology, East Surrey Hospital, Redhill, Surrey and Sussex NHS Trust, U.K. E-mail: [email protected] Received July 14, 2004; Revised September 28, 2004; Accepted October 5, 2004; Published December 10, 2004 KEYWORDS: TCC, hypercalcaemia,paraneoplastic syndrome DOMAIN: urology Hypercalcaemia associated with transitional carcinoma of the bladder is rare in the absence of metastatic disease. We report a case of paraneoplastic hypercalcaemia associated with a high-grade, organ-confined bladder carcinoma, which resolved upon surgical resection of the tumour. CASE REPORT A 58-year-old woman presented with a 3-week history of weight loss, general malaise, and constipation as well as two episodes of macroscopic haematuria. Laboratory testing on admission to hospital showed marked hypercalcaemia (3.66, normal 2.15–2.60) associated with a PTH level of 1.3 (normal 0.5–5.5) and acute renal failure (BUN 37.5, creatinine 280). Ultrasound examination showed moderate right hydroureteronephrosis associated with a large, lobulated echogenic mass in the bladder. Immediate treatment involved intravenous colloid infusion, intravenous furosemide, and intravenous pamidronate in order to treat the hypercalcaemia. Subsequent transurethral bladder resection revealed grade 3 pT2 transitional cell carcinoma (TCC). Staging computerised tomography and bone scan showed no evidence of local or distant metastatic disease. The patient then underwent radical cystectomy and ileal conduit formation. -

Artefactual Serum Hyperkalaemia and Hypercalcaemia in Essential Thrombocythaemia J Clin Pathol: First Published As 10.1136/Jcp.53.2.105 on 1 February 2000
J Clin Pathol 2000;53:105–109 105 Artefactual serum hyperkalaemia and hypercalcaemia in essential thrombocythaemia J Clin Pathol: first published as 10.1136/jcp.53.2.105 on 1 February 2000. Downloaded from M R Howard, S Ashwell, L R Bond, I Holbrook Abstract the release of potassium ions from platelets Aim—To investigate possible abnormali- which are entrapped within the clot in a serum ties of serum potassium and calcium sample. This phenomenon generally occurs levels in patients with essential thrombo- with platelet counts in excess of 600 × 109/litre, cythaemia and significant thrombocyto- with a roughly predictable increment in serum sis. potassium for every further increase in platelet Methods—24 cases of essential thrombo- count. The potassium level is normalised if the cythaemia with significant thrombocyto- estimation is made using plasma rather than sis (platelet count > 700 × 109/litre) had serum.45 serum potassium and calcium estimations Abnormalities of other ions have not been performed at the time of maximum well described in essential thrombocythaemia. thrombocytosis before treatment, and at Despite the presence of calcium in platelet- the time of low platelet count after dense granules and its secretion from platelets treatment with cytoreductive drugs. Se- during activation, there has been no systematic lected patients were further investigated study of serum calcium levels in patients with with plasma sampling and estimation of essential thrombocythaemia and significantly ionised calcium and parathyroid hor- increased platelet counts. There has been a mone. single case report of serum hypercalcaemia Results—At the time of maximum throm- associated with essential thrombocythaemia. In bocytosis six patients had serum hyperka- this case the hypercalcaemia rapidly resolved laemia (> 5.5 mmol/litre) and five had following reduction of the platelet count.6 We serum hypercalcaemia (> 2.6 mmol/litre). -

Thymoma: an Update DR CESAR MORAN
TUEDAY SURGICAL PATHOLOGY Thymoma: an update DR CESAR MORAN TUEDAY SURGICAL PATHOLOGY Glial and Glial-Neuronal Tumors DR ARIE PERRY GLIAL AND GLIO- NEURONAL TUMORS Arie Perry, M.D. DISCLOSURES (Arie Perry, MD) • I have no financial relationships to disclose. - and - • I will not discuss off label use or investigational use in my presentation School of Medicine NEUROPATHOLOGY AND REAL ESTATE • Location • Location • Location • Patient Age • Neuroimaging School of Medicine GLIOMAS • Astrocytomas (A) • Oligodendrogliomas (O) • [Mixed oligoastrocytomas (MOA)] • Ependymomas • Diffuse glioma = A, O, or MOA School of Medicine GLIOMA GRADING: WHO 2016 • Grade I = Benign • Grade II = Low-grade • Grade III = “Anaplastic” • Grade IV = High-grade malignant, e.g. “GBM” School of Medicine Distribution of Primary Malignant Brain and Other CNS Tumors by CBTRUS Histology Groupings and Histology and Behavior (N = 121,277) CBTRUS Statistical Report: NPCR and SEER, 2011–2015. Gliomas account for 26% of all primary CNS tumors, but 81% of all malignant CNS tumors Neuro Oncol. 2018;20(suppl_4):iv1-iv86. doi:10.1093/neuonc/noy131 © The Author(s) 2018. Published by Oxford University Press on behalf of the Society for Neuro-Oncology. ASTROCYTOMAS • Diffuse (75%) • Circumscribed / Favorable (25%) – Fibrillary – Pilocytic – Gemistocytic – PXA – Giant Cell – SEGA – Small Cell – DIA – Granular Cell – Epithelioid School of Medicine ASTROCYTOMA, IDH-mutant, WHO GRADE II • Age 30-40 • Insidious / Slow growing • Non-enhancing • Often progress to grades III or IV • Survival -

Society for Endocrinology National Clinical Cases 2021
Endocrine Abstracts June 2021 Volume 74 ISSN 1479-6848 (online) Society for Endocrinology National Clinical Cases 2021 22 June 2021, Online published by Online version available at bioscientifica www.endocrine-abstracts.org Volume 74 Endocrine Abstracts June 2021 Society for Endocrinology National Clinical Cases 2021 Tuesday 22 June 2021 Online Meeting Chairs Dr Anna Crown (Brighton) Dr Miles Levy (Leicester) Dr Annice Mukherjee (Manchester) Dr Michael O’Reilly (Dublin) Abstract Marking Panel Dr Kristien Boelart (Birmingham) Dr Karin Bradley (Bristol) Dr Simon Howell (Preston) Dr Andrew Lansdown (Cardiff) Dr Miles Levy (Leicester) Dr Daniel Morganstein (London) Dr Michael O’Reilly (Dublin) Professor Robert Semple (Edinburgh) Dr Peter Taylor (Cardiff) Dr Helen Turner (Oxford) Professor Bijay Vaidya (Exeter) Dr Nicola Zammitt (Edinburgh) Society for Endocrinology National Clinical Cases 2021 CONTENTS Society for Endocrinology National Clinical Cases 2021 Oral Communications ................................................. OC1–OC10 Highlighted Cases ................................................. NCC1–NCC71 AUTHOR INDEX Endocrine Abstracts (2021) Vol 74 Society for Endocrinology National Clinical Cases 2021 Oral Communications Endocrine Abstracts (2021) Vol 74 Society for Endocrinology National Clinical Cases 2021 OC1 lupus-anticoagulant. 5 days post-admission, in view of sudden onset lower A rare heterozygous IGFI variant causing postnatal growth failure and backache & worsening infection markers, repeat CT CAP was done which offering novel insights into IGF-I physiology revealed new bilateral adrenal haemorrhages. MRI adrenals revealed B/l adrenal 1 1 2 1 haemorrhages with fat stranding ,no underlying adrenal mass noted. Her 9am Emily Cottrell , Sumana Chatterjee , Vivian Hwa & Helen L. Storr ! 1 cortisol was 25, therefore she was started on IV hydrocortisone for acute Centre for Endocrinology, William Harvey Research Institute, Barts and adrenal insufficiency. -
Multiple Myeloma Associated With
ISSN: 2469-5696 Islam and Kotoucek. Int J Blood Res Disord 2018, 5:029 DOI: 10.23937/2469-5696/1410029 International Journal of Volume 5 | Issue 1 Open Access Blood Research and Disorders RESEARCH ARTICLE Multiple Myeloma Associated with Dermatomyositis: A Short Report and Mini-Review Md Serajul Islam1,2* and Pavel Kotoucek2 Check for 1Department of Haematology, Guys’ & St Thomas’ Hospital, London, UK updates 2Department of Haematology, Broomfield Hospital, Chelmsford, UK *Corresponding author: Md Serajul Islam, Department of Haematology, Guys’ & St Thomas’ Hospital, London, UK; De- partment of Haematology, Broomfield Hospital, Chelmsford, UK, Tel: +44-7769580452, Fax: +44-1245-51-6669, E-mail: [email protected] amyloid deposits in various tissues [3]. The American Abstract Cancer Society has estimated that 30,770 new MM Multiple myeloma (MM) is characterized by the neoplastic proliferation of plasma cell clones that produce monoclo- cases will occur in the United States in 2018, with an nal immunoglobulin. Dermatomyositis (DM), and to a lesser estimated 12,770 deaths [4]. Idiopathic inflammatory extent polymyositis (PM), carry a higher risk of cancer than myopathies (IIM), a heterogeneous group of disorders that of the general population as demonstrated by several characterised by weakness and inflammation of skele- studies with the prevalence being 32% and 15% for DM and PM respectively. The mechanism underlying the association tal muscle, are often associated with malignancies [5]. between idiopathic inflammatory myopathies (IIM) and ma- Polymyositis (PM) and dermatomyositis (DM) are clas- lignancies remains unclear. Both conditions predominantly sified as IIM, with these conditions predominantly af- affect adults. About 15% of DM is refractory to conventional fecting adults [6].