Bilirubin Metabolism
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Myoglobin Expression Under Hypoxic Condtions In
THESIS IN THE FACE OF HYPOXIA: MYOGLOBIN EXPRESSION UNDER HYPOXIC CONDTIONS IN CULTURED WEDDELL SEAL SKELETAL MUSCLE CELLS Submitted by Michael Anthony De Miranda Jr. Department of Biology In partial fulfillment of the requirements For the degree of Master of Science Colorado State University Fort Collins, Colorado Spring 2012 Master’s Committee: Advisor: Shane Kanatous Gregory Florant Scott Earley Copyright by Michael A. De Miranda Jr. 2012 All Rights Reserved ABSTRACT IN THE FACE OF HYPOXIA: MYOGLOBIN EXPRESSION UNDER HYPOXIC CONDITIONS IN CULTURED WEDDELL SEAL SKELETAL MUSCLE CELLS The hallmark adaptation to breath-hold diving in Weddell seals (Leptonychotes weddellii) is enhanced concentrations of myoglobin in their skeletal muscles. Myoglobin is a cytoplasmic hemoprotein that stores oxygen for use in aerobic metabolism throughout the dive duration. In addition, throughout the duration of the dive, Weddell seals rely on oxygen stored in myoglobin to sustain aerobic metabolism in which lipid is the primary contributor of acetyl CoA for the citric acid cycle. Together, enhanced myoglobin concentrations and a lipid-based aerobic metabolism represent some of the unique adaptations to diving found in skeletal muscle of Weddell seals. This thesis presents data that suggests cultured Weddell seal skeletal muscle cells inherently possess adaptations to diving such as increased myoglobin concentrations, and rely on lipids to fuel aerobic metabolism. I developed the optimum culture media for this unique primary cell line based on myoblast confluence, myoblast growth rates, myotube counts, and myotube widths. Once the culture media was established, I then determined the de novo expression of myoglobin under normoxic and hypoxic oxygen conditions and the metabolic profile of the myotubes under each oxygen condition. -

Hyperbilirubinemia
Porphyrins Porphyrins (Porphins) are cyclic tetrapyrol compounds formed by the linkage )). of four pyrrole rings through methenyl bridges (( HC In the reduced porphyrins (Porphyrinogens) the linkage of four pyrrole rings (tetrapyrol) through methylene bridges (( CH2 )) The characteristic property of porphyrins is the formation of complexes with the metal ion bound to nitrogen atoms of the pyrrole rings. e.g. Heme (iron porphyrin). Proteins which contain heme ((hemoproteins)) are widely distributed e.g. Hemoglobin, Myoglobin, Cytochromes, Catalase & Tryptophan pyrrolase. Natural porphyrins have substituent side chains on the eight hydrogen atoms numbered on the pyrrole rings. These side chains are: CH 1-Methyl-group (M)… (( 3 )) 2-Acetate-group (A)… (( CH2COOH )) 3-Propionate-group (P)… (( CH2CH2COOH )) 4-Vinyl-group (V)… (( CH CH2 )) Porphyrins with asymmetric arrangement of the side chains are classified as type III porphyrins while those with symmetric arrangement of the side chains are classified as type I porphyrins. Only types I & III are present in nature & type III series is more important because it includes heme. 1 Heme Biosynthesis Heme biosynthesis occurs through the following steps: 1-The starting reaction is the condensation between succinyl-CoA ((derived from citric acid cycle in the mitochondria)) & glycine, this reaction is a rate limiting reaction in the hepatic heme synthesis, it occurs in the mitochondria & is catalyzed by ALA synthase (Aminolevulinate synthase) enzyme in the presence of pyridoxal phosphate as a cofactor. The product of this reaction is α-amino-β-ketoadipate which is rapidly decarboxylated to form δ-aminolevulinate (ALA). 2-In the cytoplasm condensation reaction between two molecules of ALA is catalyzed by ALA dehydratase enzyme to form two molecules of water & one 2 molecule of porphobilinogen (PBG) which is a precursor of pyrrole. -

Porphyrins & Bile Pigments
Bio. 2. ASPU. Lectu.6. Prof. Dr. F. ALQuobaili Porphyrins & Bile Pigments • Biomedical Importance These topics are closely related, because heme is synthesized from porphyrins and iron, and the products of degradation of heme are the bile pigments and iron. Knowledge of the biochemistry of the porphyrins and of heme is basic to understanding the varied functions of hemoproteins in the body. The porphyrias are a group of diseases caused by abnormalities in the pathway of biosynthesis of the various porphyrins. A much more prevalent clinical condition is jaundice, due to elevation of bilirubin in the plasma, due to overproduction of bilirubin or to failure of its excretion and is seen in numerous diseases ranging from hemolytic anemias to viral hepatitis and to cancer of the pancreas. • Metalloporphyrins & Hemoproteins Are Important in Nature Porphyrins are cyclic compounds formed by the linkage of four pyrrole rings through methyne (==HC—) bridges. A characteristic property of the porphyrins is the formation of complexes with metal ions bound to the nitrogen atom of the pyrrole rings. Examples are the iron porphyrins such as heme of hemoglobin and the magnesium‐containing porphyrin chlorophyll, the photosynthetic pigment of plants. • Natural Porphyrins Have Substituent Side Chains on the Porphin Nucleus The porphyrins found in nature are compounds in which various side chains are substituted for the eight hydrogen atoms numbered in the porphyrin nucleus. As a simple means of showing these substitutions, Fischer proposed a shorthand formula in which the methyne bridges are omitted and a porphyrin with this type of asymmetric substitution is classified as a type III porphyrin. -
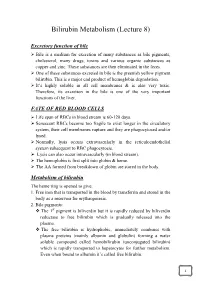
Bilirubin Metabolism (Lecture 8)
Bilirubin Metabolism (Lecture 8) Excretory function of bile Bile is a medium for excretion of many substances as bile pigments, cholesterol, many drugs, toxins and various organic substances as copper and zinc. These substances are then eliminated in the feces. One of these substances excreted in bile is the greenish yellow pigment bilirubin. This is a major end product of hemoglobin degradation. It’s highly soluble in all cell membranes & is also very toxic. Therefore, its excretion in the bile is one of the very important functions of the liver. FATE OF RED BLOOD CELLS Life span of RBCs in blood stream is 60-120 days. Senescent RBCs become too fragile to exist longer in the circulatory system, their cell membranes rupture and they are phagocytosed and/or lysed. Normally, lysis occurs extravascularly in the reticuloendothelial system subsequent to RBC phagocytosis. Lysis can also occur intravascularly (in blood stream). The hemoglobin is first split into globin & heme. The AA formed from breakdown of globin are stored in the body. Metabolism of bilirubin The heme ring is opened to give: 1. Free iron that is transported in the blood by transferrin and stored in the body as a reservoir for erythropoiesis. 2. Bile pigments: The 1st pigment is biliverdin but it is rapidly reduced by biliverdin reductase to free bilirubin which is gradually released into the plasma. The free bilirubin is hydrophobic, immediately combines with plasma proteins (mainly albumin and globulin) forming a water soluble compound called hemobilirubin (unconjugated bilirubin) which is rapidly transported to hepatocytes for further metabolism. Even when bound to albumin it’s called free bilirubin. -

Biochemistry I Enzymes
BIOCHEMISTRY I 3rd. Stage Lec. ENZYMES Biomedical Importance: Enzymes, which catalyze the biochemical reactions, are essential for life. They participate in the breakdown of nutrients to supply energy and chemical building blocks; the assembly of those building blocks into proteins, DNA, membranes, cells, and tissues; and the harnessing of energy to power cell motility, neural function, and muscle contraction. The vast majority of enzymes are proteins. Notable exceptions include ribosomal RNAs and a handful of RNA molecules imbued with endonuclease or nucleotide ligase activity known collectively as ribozymes. The ability to detect and to quantify the activity of specific enzymes in blood, other tissue fluids, or cell extracts provides information that complements the physician’s ability to diagnose and predict the prognosis of many diseases. Further medical applications include changes in the quantity or in the catalytic activity of key enzymes that can result from genetic defects, nutritional deficits, tissue damage, toxins, or infection by viral or bacterial pathogens (eg, Vibrio cholerae). Medical scientists address imbalances in enzyme activity by using pharmacologic agents to inhibit specific enzymes and are investigating gene therapy as a means to remedy deficits in enzyme level or function. In addition to serving as the catalysts for all metabolic processes, their impressive catalytic activity, substrate specificity, and stereospecificity enable enzymes to fulfill key roles in additional processes related to human health and well-being. Proteases and amylases augment the capacity of detergents to remove dirt and stains, and enzymes play important roles in producing or enhancing the nutrient value of food products for both humans and animals. -

Myoglobin from Equine Skeletal Muscle
Myoglobin from equine skeletal muscle Catalog Number M0630 Storage Temperature –20 C CAS RN 100684-32-0 Precautions and Disclaimer This product is for R&D use only, not for drug, Product Description household, or other uses. Please consult the Safety Molecular mass:1 17.6 kDa Data Sheet for information regarding hazards and safe Extinction coefficient:2 EmM = 12.92 (555 nm) handling practices. pI:3 7.3 (major component) and 6.8 (minor component) Preparation Instructions Myoglobin from horse skeletal muscle is a single chain This protein is soluble in water (10 mg/ml), yielding a heme protein containing 153 amino acid residues. It clear, red brown solution. posesses no disulfide bridges or free -SH groups. Myoglobin contains 8 variously sized right-handed References helical regions, joined by non-ordered or random coil 1. Darbre, P.D. et al., Comparison of the myoglobin of regions. These 8 helices (A, B, C, D, E, F, G, and H) the zebra (Equus burchelli) with that of the horse are folded back on top of one another, and the heme is (Equus cabalus). Biochim. Biophys. Acta, 393(1), situated between helices E and F. The heme is almost 201-204 (1975). totally buried. Only the edge carrying the two 2. Bowen, W.J., The absorption spectra and extinction hydrophylic propionic acid groups is exposed. The coefficients of myoglobin. J. Biol. Chem., 179, 235- heme is held in position by a coordinating complex 245 (1949). between the central Fe(II) atom and 2 histidine residues 3. Radola, B.J., Isoelectric focusing in layers of (on helices E and F, respectively). -
NEONATAL Hb, O2-TRANSPORT & JAUNDICE: OVERVIEW
BILIRUBIN METABOLISM & JAUNDICE UNIVERSITY OF PNG SCHOOL OF MEDICINE AND HEALTH SCIENCES DISCIPLINE OF BIOCHEMISTRY & MOLECULAR BIOLOGY PBL MBBS II SEMINAR VJ Temple 1 Brief description of Hemoglobin (Hb) structure • Hemoglobin (Hb): Made up of 4-Subunits (Tetramer) held together by multiple non-covalent interactions; • Each subunit consist of: • Heme (Ferro-Protoporphyrin), • Globin protein; • Heme: Protoporphyrin IX and Ferrous ion (Fe2); • Globin protein folds around Heme group forming a protective Hydrophobic pocket; • Heme is the site of Oxygen binding; 2 • There are different types of Hemoglobin, with different subunits: • Foetal Hemoglobin (Hb F): 2 2 Two types of Adult Hemoglobin (Hb A): • Hb A1 represented as: 2 2 • It is the major (98%) form of Hb in adults; • Hb A2 represented as: 2 2 • It is the minor (2%) form of Hb in adults; 3 What are the major sources of Heme in humans? • RBC is major source of Heme in humans, • Life span of RBC is about 120 days, • Other sources of Heme include: • Myoglobin (Mb): Stores Oxygen in muscle cells, • Cytochromes: present in some enzymes, • Catalase: an enzyme, 4 What normally happens to RBC after 120 days? • RBC is destroyed mainly in Reticuloendothelial system (Extra-vascular system: Spleen and Liver); • Daily turnover of Hb is about 6 g/day; • Hb is broken down, • Globin protein is hydrolyzed to amino acids, • Protoporphyrin Ring in Heme is Hydrophobic, thus must be made soluble before it is excreted, • Ferrous ion is removed and stored in Iron pool, for reuse, • Protoporphyrin ring is metabolized -
Bilirubin PDF 12Days
Bilirubin Physiology – WYNTKFTB • Bilirubin metabolism – Unconjugated – Conjugation – Excretion • Enterohepatic circulation • Implication of bilirubin metabolism – Urine – Stool • Understand the metabolic pathway as related to the disease state of JAUNDICE Don’t make me come up there and steal your google machines! BR - Alb Thank you. BG the Bilirubin an overview by howard sachs Slo-Motion Instant Replay… Heme oxygenase Biliverdin Reductase Heme oxygenase Biliverdin Reductase Bilirubin Albumin (unconjugated) …not water soluble… Unconjugated Bilirubin (‘Indirect’) Key points: • ‘Attached to albumin’: too big to pass through glomerular filtration barrier. • Intravascular: Hemoglobin ® urine • Unconjugated: not water soluble. How can we get too much unconjugated bilirubin in the serum? 1. Hemolysis • Elevated indirect bilirubin is used as a diagnostic marker (with LDH, ¯ haptoglobin) 2. Conjugation defect: inherited (Gilbert’s, Crigler-Najjar) Multidrug resistance associated protein Bilirubin binds to cytosolic binding protein, glutathione s-transferase (GST) for transport to ER Conjugation of bilirubin is catalyzed by bilirubin-uridinediphosphate (UDP)- glucuronosyltransferase (UGT1A1). Product is bilirubin diglucuronide. UDPGA is the donor sugar Multidrug resistance Endoplasmic reticulum associated protein Bilirubin diglucuronide Conjugated (direct) Bilirubin binds to cytosolic binding protein, glutathione s-transferase (GST) for transport to ER Conjugation of bilirubin is catalyzed by bilirubin-uridinediphosphate (UDP)- glucuronosyltransferase -

A Short Review of Iron Metabolism and Pathophysiology of Iron Disorders
medicines Review A Short Review of Iron Metabolism and Pathophysiology of Iron Disorders Andronicos Yiannikourides 1 and Gladys O. Latunde-Dada 2,* 1 Faculty of Life Sciences and Medicine, Henriette Raphael House Guy’s Campus King’s College London, London SE1 1UL, UK 2 Department of Nutritional Sciences, School of Life Course Sciences, King’s College London, Franklin-Wilkins-Building, 150 Stamford Street, London SE1 9NH, UK * Correspondence: [email protected] Received: 30 June 2019; Accepted: 2 August 2019; Published: 5 August 2019 Abstract: Iron is a vital trace element for humans, as it plays a crucial role in oxygen transport, oxidative metabolism, cellular proliferation, and many catalytic reactions. To be beneficial, the amount of iron in the human body needs to be maintained within the ideal range. Iron metabolism is one of the most complex processes involving many organs and tissues, the interaction of which is critical for iron homeostasis. No active mechanism for iron excretion exists. Therefore, the amount of iron absorbed by the intestine is tightly controlled to balance the daily losses. The bone marrow is the prime iron consumer in the body, being the site for erythropoiesis, while the reticuloendothelial system is responsible for iron recycling through erythrocyte phagocytosis. The liver has important synthetic, storing, and regulatory functions in iron homeostasis. Among the numerous proteins involved in iron metabolism, hepcidin is a liver-derived peptide hormone, which is the master regulator of iron metabolism. This hormone acts in many target tissues and regulates systemic iron levels through a negative feedback mechanism. Hepcidin synthesis is controlled by several factors such as iron levels, anaemia, infection, inflammation, and erythropoietic activity. -

Myoglobin and Creatine Kinase in Acute Myocardial Infarction
Br Heart J 1984; 51: 189-94 Myoglobin and creatine kinase in acute myocardial infarction J M McCOMB, E A McMASTER, G MAcKENZIE, A A J ADGEY From the Regional Medical Cardiology Centre, Royal Victoria Hospital, Belfast, Northem Ireland SUMMARY Serum myoglobin concentration and creatine kinase activity were measured serially in 70 consecutive patients presenting within four hours of the onset of symptoms of suspected acute myocardial infarction. Of 36 patients with definite or possible myocardial infarction (WHO criteria), the serum myoglobin concentration was raised (>85 ,g/l) one hour after the onset of symptoms in 25% and at four hours in 890/o. Creatine kinase activity was raised (>140 U/1) one hour after the onset in 25% and at four hours in only 56%. Within 12 hours of the onset of symptoms the myoglobin concentration reached a peak in 83% and the creatine kinase a peak in only 14%. Within 36 hours the myoglobin concentration fell to normal values in 67% while creatine kinase activity fell to normal values in only 3%. Four hours after the onset of symptoms the serum myoglobin concen- tration distinguished easily those patients with myocardial infarction from those without, whereas when creatine kinase values were used the sensitivity was poor but the specificity high. From the combined results ofthe two studies and using a single measurement of serum myoglobin concentration at six hours from the onset of symptoms to predict the diagnosis in 114 patients with suspected infarction, the sensitivity was 93% and specificity 890/o. Kiss and Reinhart' first reported abnormal serum PART 1 concentrations ofmyoglobin 10 to 12 hours after acute Seventy consecutive patients with symptoms sugges- myocardial infarction. -

Delayed Onset Muscle Soreness in People with Diabetes; Biomarkers and Nutritional Supplementation Hani H
Loma Linda University TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works Loma Linda University Electronic Theses, Dissertations & Projects 12-1-2011 Delayed Onset Muscle Soreness in People with Diabetes; Biomarkers and Nutritional Supplementation Hani H. Al-Nakhli Loma Linda University Follow this and additional works at: http://scholarsrepository.llu.edu/etd Part of the Rehabilitation and Therapy Commons Recommended Citation Al-Nakhli, Hani H., "Delayed Onset Muscle Soreness in People with Diabetes; Biomarkers and Nutritional Supplementation" (2011). Loma Linda University Electronic Theses, Dissertations & Projects. 19. http://scholarsrepository.llu.edu/etd/19 This Dissertation is brought to you for free and open access by TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works. It has been accepted for inclusion in Loma Linda University Electronic Theses, Dissertations & Projects by an authorized administrator of TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works. For more information, please contact [email protected]. Loma Linda University School of Allied Health Professions in conjunction with the Faculty of Graduate Studies _____________________ Delayed Onset Muscle Soreness in People with Diabetes; Biomarkers and Nutritional Supplementation by Hani H. Al-Nakhli _____________________ A Dissertation submitted in partial satisfaction of the requirements for the degree Doctor of Philosophy in Rehabilitations Science _____________________ December, 2011 © 2011 Hani H. Al-Nakhli All Right Reserved Each person whose signature appears below certifies that this dissertation in his/her opinion is adequate, in scope and quality, as a dissertation for the degree Doctor of Philosophy. , Chairperson Jerrold S. Petrofsky, Professor of Physical Therapy, Director of Research Lee S. Berk, Associate Professor of Physical Therapy Richard Hubbard, Professor of Pathology Michael S. -

Attenuation of Glucose-Induced Myoglobin Glycation and the Formation of Advanced Glycation End Products (Ages) by (R)-Α-Lipoic Acid in Vitro
biomolecules Article Attenuation of Glucose-Induced Myoglobin Glycation and the Formation of Advanced Glycation End Products (AGEs) by (R)-α-Lipoic Acid In Vitro Hardik Ghelani 1,2, Valentina Razmovski-Naumovski 1,2,3, Rajeswara Rao Pragada 4 and Srinivas Nammi 1,2,* ID 1 School of Science and Health, Western Sydney University, Sydney, NSW 2751, Australia; [email protected] (H.G.); [email protected] (V.R.-N.) 2 National Institute of Complementary Medicine (NICM), Western Sydney University, Sydney, NSW 2751, Australia 3 South Western Sydney Clinical School, School of Medicine, University of New South Wales, Sydney, NSW 2052, Australia 4 Department of Pharmacology, College of Pharmaceutical Sciences, Andhra University, Visakhapatnam 530003, Andhra Pradesh, India; [email protected] * Correspondence: [email protected]; Tel.: +61-2-4620-3038; Fax: +61-2-4620-3025 Received: 1 December 2017; Accepted: 1 February 2018; Published: 8 February 2018 Abstract: High-carbohydrate containing diets have become a precursor to glucose-mediated protein glycation which has been linked to an increase in diabetic and cardiovascular complications. The aim of the present study was to evaluate the protective effect of (R)-α-lipoic acid (ALA) against glucose-induced myoglobin glycation and the formation of advanced glycation end products (AGEs) in vitro. Methods: The effect of ALA on myoglobin glycation was determined via the formation of AGEs fluorescence intensity, iron released from the heme moiety of myoglobin and the level of fructosamine. The extent of glycation-induced myoglobin oxidation was measured via the levels of protein carbonyl and thiol. Results: The results showed that the co-incubation of ALA (1, 2 and 4 mM) with myoglobin (1 mg/mL) and glucose (1 M) significantly decreased the levels of fructosamine, which is directly associated with the decrease in the formation of AGEs.