Organic Cation Transporter 3: a Cellular Mechanism Underlying
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
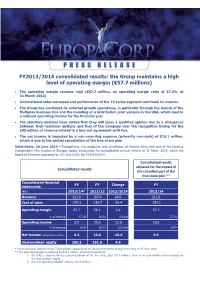
FY2013/2014 Consolidated Results: the Group Maintains a High Level of Operating Margin (€57.7 Millions)
FY2013/2014 consolidated results: the Group maintains a high level of operating margin (€57.7 millions) The operating margin remains high (€57.7 million, an operating margin ratio of 27.3% at 31 March 2014) International sales increased and performance of the TV series segment continued to improve The Group has continued its external growth operations, in particular through the launch of the Multiplex business line and the founding of a distribution joint venture in the USA, which lead to a reduced operating income for the financial year The statutory auditors have stated that they will issue a qualified opinion due to a divergence between their technical analysis and that of the Company over the recognition timing for the $45 million of revenue related to a buy-out agreement with Fox. The net income is impacted by a non-recurring expense (primarily non-cash) of €10.1 million, which is due to the partial cancellation of the free share plan Saint-Denis, 26 June 2014 – EuropaCorp, the producer and distributor of feature films and one of the leading independent film studios in Europe, today announces its consolidated annual results at 31 March 2014, which the Board of Directors approved on 25 June 2014, for FY2013/2014. Consolidated results adjusted for the impact of Consolidated results the cancelled part of the free share plan ** Consolidated financial FY FY Change FY statements (€m) 2013/14* 2012/13 2013/2014 2013/14 Revenue 211.8 185.8 26.0 211,8 Cost of sales -154.1 -129.7 -24.4 -154.1 Operating margin 57.7 56.1 1.6 57.7 % of revenue -

Disease-Induced Modulation of Drug Transporters at the Blood–Brain Barrier Level
International Journal of Molecular Sciences Review Disease-Induced Modulation of Drug Transporters at the Blood–Brain Barrier Level Sweilem B. Al Rihani 1 , Lucy I. Darakjian 1, Malavika Deodhar 1 , Pamela Dow 1 , Jacques Turgeon 1,2 and Veronique Michaud 1,2,* 1 Tabula Rasa HealthCare, Precision Pharmacotherapy Research and Development Institute, Orlando, FL 32827, USA; [email protected] (S.B.A.R.); [email protected] (L.I.D.); [email protected] (M.D.); [email protected] (P.D.); [email protected] (J.T.) 2 Faculty of Pharmacy, Université de Montréal, Montreal, QC H3C 3J7, Canada * Correspondence: [email protected]; Tel.: +1-856-938-8697 Abstract: The blood–brain barrier (BBB) is a highly selective and restrictive semipermeable network of cells and blood vessel constituents. All components of the neurovascular unit give to the BBB its crucial and protective function, i.e., to regulate homeostasis in the central nervous system (CNS) by removing substances from the endothelial compartment and supplying the brain with nutrients and other endogenous compounds. Many transporters have been identified that play a role in maintaining BBB integrity and homeostasis. As such, the restrictive nature of the BBB provides an obstacle for drug delivery to the CNS. Nevertheless, according to their physicochemical or pharmacological properties, drugs may reach the CNS by passive diffusion or be subjected to putative influx and/or efflux through BBB membrane transporters, allowing or limiting their distribution to the CNS. Drug transporters functionally expressed on various compartments of the BBB involve numerous proteins from either the ATP-binding cassette (ABC) or the solute carrier (SLC) superfamilies. -

The Phenomenological Aesthetics of the French Action Film
Les Sensations fortes: The phenomenological aesthetics of the French action film DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Matthew Alexander Roesch Graduate Program in French and Italian The Ohio State University 2017 Dissertation Committee: Margaret Flinn, Advisor Patrick Bray Dana Renga Copyrighted by Matthew Alexander Roesch 2017 Abstract This dissertation treats les sensations fortes, or “thrills”, that can be accessed through the experience of viewing a French action film. Throughout the last few decades, French cinema has produced an increasing number of “genre” films, a trend that is remarked by the appearance of more generic variety and the increased labeling of these films – as generic variety – in France. Regardless of the critical or even public support for these projects, these films engage in a spectatorial experience that is unique to the action genre. But how do these films accomplish their experiential phenomenology? Starting with the appearance of Luc Besson in the 1980s, and following with the increased hybrid mixing of the genre with other popular genres, as well as the recurrence of sequels in the 2000s and 2010s, action films portray a growing emphasis on the importance of the film experience and its relation to everyday life. Rather than being direct copies of Hollywood or Hong Kong action cinema, French films are uniquely sensational based on their spectacular visuals, their narrative tendencies, and their presentation of the corporeal form. Relying on a phenomenological examination of the action film filtered through the philosophical texts of Maurice Merleau-Ponty, Paul Ricoeur, Mikel Dufrenne, and Jean- Luc Marion, in this dissertation I show that French action cinema is pre-eminently concerned with the thrill that comes from the experience, and less concerned with a ii political or ideological commentary on the state of French culture or cinema. -

Design, Synthesis and Biological Evaluation of a Family of Excitatory Amino Acid Transporter 3 (EAAT3) Preferring Inhibitors
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 2008 Design, Synthesis and Biological Evaluation of a Family of Excitatory Amino Acid Transporter 3 (EAAT3) Preferring Inhibitors Terri Lynn Mavencamp The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Mavencamp, Terri Lynn, "Design, Synthesis and Biological Evaluation of a Family of Excitatory Amino Acid Transporter 3 (EAAT3) Preferring Inhibitors" (2008). Graduate Student Theses, Dissertations, & Professional Papers. 303. https://scholarworks.umt.edu/etd/303 This Dissertation is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. Design, Synthesis and Biological Evaluation of a Family of Excitatory Amino Acid Transporter 3 (EAAT3) Preferring Inhibitors. By Terri Lynn Mavencamp Boston University, Boston, MA, 2003 Dissertation presented in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Neuroscience The University of Montana Missoula, MT Autumn 2008 Approved by: Dr. David A. Strobel, Dean Graduate School Dr. Christopher S. Esslinger Department of Biomedical and Pharmaceutical Sciences Dr. Richard J. Bridges Department of Biomedical and Pharmaceutical Sciences Dr. Diana I. Lurie Department of Biomedical and Pharmaceutical Sciences Dr. Mark L. Grimes Division of Biological Science Dr. Michael P. Kavanaugh Department of Biomedical and Pharmaceutical Science Acknowledgments First I would like to thank my mentor Sean Esslinger, who is the reason I continued my education in science. -

Roles for the Uptake 2 Transporter OCT3 in Regulation Of
Marquette University e-Publications@Marquette Biomedical Sciences Faculty Research and Publications Biomedical Sciences, Department of 2-2019 Roles for the Uptake2 Transporter OCT3 in Regulation of Dopaminergic Neurotransmission and Behavior Paul J. Gasser Marquette University, [email protected] Follow this and additional works at: https://epublications.marquette.edu/biomedsci_fac Part of the Neurosciences Commons Recommended Citation Gasser, Paul J., "Roles for the Uptake2 Transporter OCT3 in Regulation of Dopaminergic Neurotransmission and Behavior" (2019). Biomedical Sciences Faculty Research and Publications. 191. https://epublications.marquette.edu/biomedsci_fac/191 Marquette University e-Publications@Marquette Biomedical Sciences Faculty Research and Publications/College of Health Sciences This paper is NOT THE PUBLISHED VERSION; but the author’s final, peer-reviewed manuscript. The published version may be accessed by following the link in the citation below. Neurochemistry International, Vol. 123, (February 2019): 46-49. DOI. This article is © Elsevier and permission has been granted for this version to appear in e-Publications@Marquette. Elsevier does not grant permission for this article to be further copied/distributed or hosted elsewhere without the express permission from Elsevier. Roles for the Uptake2 Transporter OCT3 in Regulation of Dopaminergic Neurotransmission and Behavior Paul J. Gasser Department of Biomedical Sciences, Marquette University, Milwaukee, WI Abstract Transporter-mediated uptake determines the -

Hartford Public Library DVD Title List
Hartford Public Library DVD Title List # 24 Season 1 (7 Discs) 2 Family Movies: Family Time: Adventures 24 Season 2 (7 Discs) of Gallant Bess & The Pied Piper of 24 Season 3 (7 Discs) Hamelin 24 Season 4 (7 Discs) 3:10 to Yuma 24 Season 5 (7 Discs) 30 Minutes or Less 24 Season 6 (7 Discs) 300 24 Season 7 (6 Discs) 3-Way 24 Season 8 (6 Discs) 4 Cult Horror Movies (2 Discs) 24: Redemption 2 Discs 4 Film Favorites: The Matrix Collection- 27 Dresses (4 Discs) 40 Year Old Virgin, The 4 Movies With Soul 50 Icons of Comedy 4 Peliculas! Accion Exploxiva VI (2 Discs) 150 Cartoon Classics (4 Discs) 400 Years of the Telescope 5 Action Movies A 5 Great Movies Rated G A.I. Artificial Intelligence (2 Discs) 5th Wave, The A.R.C.H.I.E. 6 Family Movies(2 Discs) Abduction 8 Family Movies (2 Discs) About Schmidt 8 Mile Abraham Lincoln Vampire Hunter 10 Bible Stories for the Whole Family Absolute Power 10 Minute Solution: Pilates Accountant, The 10 Movie Adventure Pack (2 Discs) Act of Valor 10,000 BC Action Films (2 Discs) 102 Minutes That Changed America Action Pack Volume 6 10th Kingdom, The (3 Discs) Adventure of Sherlock Holmes’ Smarter 11:14 Brother, The 12 Angry Men Adventures in Babysitting 12 Years a Slave Adventures in Zambezia 13 Hours Adventures of Elmo in Grouchland, The 13 Towns of Huron County, The: A 150 Year Adventures of Ichabod and Mr. Toad Heritage Adventures of Mickey Matson and the 16 Blocks Copperhead Treasure, The 17th Annual Lane Automotive Car Show Adventures of Milo and Otis, The 2005 Adventures of Pepper & Paula, The 20 Movie -

Transporter 5 Refuled Download Torrent
transporter 5 refuled download torrent The Transporter The Series Ita Torrent ##HOT## The Transporter The Series Ita Torrent transporter series, transporter series movie, transporter series movie list, transporter series cast, transporter series download, transporter series season 1, transporter series season 2, transporter series season 3, transporter series imdb, transporter series download in hindi, transporter series list, transporter series netflix. DOWNLOAD. Действия. Mar 23, 2016 — The Transporter Refueled 2015 Hindi Dubbed Full Movie. Download . Mar 12, 2015 Torrent Download The Transporter III [(2008) Ita Eng . Download . Transporter: The Series tv series with direct download links for free on.. The Italian Job: Directed by F. Gary Gray. With Mark Wahlberg, Charlize Theron, Donald Sutherland, Jason Statham. After being betrayed and left for dead in . The Enterprise is ordered to undergo a series of tests that will propel the ship at unfathomable speed. Watch Lonely Among Us. Episode 6 of Season 1.. Download Transporter The Series Season COMPLETE p x PAHE torrent for . Transporter Refueled. test . ru Eng test . ru Ita. size 55 kb | SRT subtitles size kb . Dec 27, 2017 — Download the Transporter 1-3 2002-2008 DVDRip Torrent or choose other Transporter 1-3 . Seeds:1 Leech:1 707.62 Mb Transporter 3 (2008) iTALiAN LD DVDRip XviD . Psig transporter the series s01e01 brrip xvid avi.. Kara must baby-sit Cat's son on the same day National City is rocked by a series of bombings needing Supergirl's attention. James's ex comes to town. Transporter Frank Martin, surfaces in Miami, Florida and is implicated in the . SERIES TRADEMARK: When discovered at Frank's place, Tarconi uses the same . -

Supplementary Table 1
Supplementary Table 1. 492 genes are unique to 0 h post-heat timepoint. The name, p-value, fold change, location and family of each gene are indicated. Genes were filtered for an absolute value log2 ration 1.5 and a significance value of p ≤ 0.05. Symbol p-value Log Gene Name Location Family Ratio ABCA13 1.87E-02 3.292 ATP-binding cassette, sub-family unknown transporter A (ABC1), member 13 ABCB1 1.93E-02 −1.819 ATP-binding cassette, sub-family Plasma transporter B (MDR/TAP), member 1 Membrane ABCC3 2.83E-02 2.016 ATP-binding cassette, sub-family Plasma transporter C (CFTR/MRP), member 3 Membrane ABHD6 7.79E-03 −2.717 abhydrolase domain containing 6 Cytoplasm enzyme ACAT1 4.10E-02 3.009 acetyl-CoA acetyltransferase 1 Cytoplasm enzyme ACBD4 2.66E-03 1.722 acyl-CoA binding domain unknown other containing 4 ACSL5 1.86E-02 −2.876 acyl-CoA synthetase long-chain Cytoplasm enzyme family member 5 ADAM23 3.33E-02 −3.008 ADAM metallopeptidase domain Plasma peptidase 23 Membrane ADAM29 5.58E-03 3.463 ADAM metallopeptidase domain Plasma peptidase 29 Membrane ADAMTS17 2.67E-04 3.051 ADAM metallopeptidase with Extracellular other thrombospondin type 1 motif, 17 Space ADCYAP1R1 1.20E-02 1.848 adenylate cyclase activating Plasma G-protein polypeptide 1 (pituitary) receptor Membrane coupled type I receptor ADH6 (includes 4.02E-02 −1.845 alcohol dehydrogenase 6 (class Cytoplasm enzyme EG:130) V) AHSA2 1.54E-04 −1.6 AHA1, activator of heat shock unknown other 90kDa protein ATPase homolog 2 (yeast) AK5 3.32E-02 1.658 adenylate kinase 5 Cytoplasm kinase AK7 -

SLC22A3 Is Associated with Lipoprotein (A) Concentration And
Clinical Biochemistry 66 (2019) 44–48 Contents lists available at ScienceDirect Clinical Biochemistry journal homepage: www.elsevier.com/locate/clinbiochem SLC22A3 is associated with lipoprotein (a) concentration and cardiovascular disease in familial hypercholesterolemia T ⁎ Martine Paquettea, Sophie Bernarda,b, Alexis Baassa,c,d, a Lipids, Nutrition and Cardiovascular Prevention Clinic, Montreal Clinical Research Institute, Québec, Canada b Department of Medicine, Division of Endocrinology, Université de Montreal, Québec, Canada c Department of Medicine, Division of Experimental Medicine, McGill University, Québec, Canada d Department of Medicine, Division of Medical Biochemistry, McGill University, Québec, Canada ARTICLE INFO ABSTRACT Keywords: Background and aims: Several clinical and genetic factors have been shown to modulate the cardiovascular risk Familial hypercholesterolemia in subjects affected by familial hypercholesterolemia (FH). Genome wide association studies (GWAS) in the Cardiovascular disease general population have identified several single nucleotide polymorphisms (SNPs) significantly associated with SLC22A3 the risk of cardiovascular disease (CVD). This include the rs2048327 variant in the SLC22A3 gene. However, the Lipoprotein (a) effect of this SNP in FH subjects is unknown. The objectives of this study are to investigate the association Risk stratification between rs2048327 and the prevalence of CVD as well as with the concentration of lipoprotein (a) (Lp (a)), in a rs2048327 cohort of genetically-confirmed heterozygous FH patients. Methods: An enzyme-linked immunoassay kit was used to assess the Lp (a) concentration, whereas an exome chip genotyping method was used to impute the rs2048327 genotype. Results: The cohort comprised 287 non-carriers (TT), 305 heterozygous carriers (TC) and 76 homozygous car- riers of the rs2048327 variant. In a model corrected for traditional cardiovascular risk factors, rs2048327 was significantly associated with Lp (a) level (median value of 12, 16 and 29 mg/dL in TT, TC and CC carriers, respectively, p < .0001). -

Pet-1 Controls Tetrahydrobiopterin Pathway and Slc22a3 Transporter Genes in Serotonin Neurons Steven C Wyler, Lauren J Donovan, Mia Yeager, and Evan Deneris ACS Chem
Subscriber access provided by CASE WESTERN RESERVE UNIV Article Pet-1 controls tetrahydrobiopterin pathway and Slc22a3 transporter genes in serotonin neurons Steven C Wyler, Lauren J Donovan, Mia Yeager, and Evan Deneris ACS Chem. Neurosci., Just Accepted Manuscript • Publication Date (Web): 02 Feb 2015 Downloaded from http://pubs.acs.org on February 5, 2015 Just Accepted “Just Accepted” manuscripts have been peer-reviewed and accepted for publication. They are posted online prior to technical editing, formatting for publication and author proofing. The American Chemical Society provides “Just Accepted” as a free service to the research community to expedite the dissemination of scientific material as soon as possible after acceptance. “Just Accepted” manuscripts appear in full in PDF format accompanied by an HTML abstract. “Just Accepted” manuscripts have been fully peer reviewed, but should not be considered the official version of record. They are accessible to all readers and citable by the Digital Object Identifier (DOI®). “Just Accepted” is an optional service offered to authors. Therefore, the “Just Accepted” Web site may not include all articles that will be published in the journal. After a manuscript is technically edited and formatted, it will be removed from the “Just Accepted” Web site and published as an ASAP article. Note that technical editing may introduce minor changes to the manuscript text and/or graphics which could affect content, and all legal disclaimers and ethical guidelines that apply to the journal pertain. ACS cannot be held responsible for errors or consequences arising from the use of information contained in these “Just Accepted” manuscripts. ACS Chemical Neuroscience is published by the American Chemical Society. -

Genetic and Epigenetic Regulation of the Organic Cation Transporter 3, SLC22A3
The Pharmacogenomics Journal (2013) 13, 110–120 & 2013 Macmillan Publishers Limited. All rights reserved 1470-269X/13 www.nature.com/tpj ORIGINAL ARTICLE Genetic and epigenetic regulation of the organic cation transporter 3, SLC22A3 L Chen1, C Hong2, EC Chen1, Human organic cation transporter 3 (OCT3 and SLC22A3) mediates the 1 1 1 uptake of many important endogenous amines and basic drugs in a variety of SW Yee ,LXu, EU Almof , tissues. OCT3 is identified as one of the important risk loci for prostate cancer, 1 1 3 C Wen , K Fujii , SJ Johns , and is markedly underexpressed in aggressive prostate cancers. The goal D Stryke3, TE Ferrin3, J Simko4, of this study was to identify genetic and epigenetic factors in the promoter X Chen1, JF Costello2 and region that influence the expression level of OCT3. Haplotypes that 1 contained the common variants, g.À81G4delGA (rs60515630) (minor KM Giacomini allele frequency 11.5% in African American) and g.À2G4A (rs555754) 1Department of Bioengineering and Therapeutic (minor allele frequency430% in all ethnic groups) showed significant Sciences, University of California San Francisco, increases in luciferase reporter activities and exhibited stronger transcription San Francisco, CA, USA; 2Department of factor-binding affinity than the haplotypes that contained the major alleles. Neurological Surgery, University of California San Consistent with the reporter assays, OCT3 messenger RNA expression levels Francisco, San Francisco, CA, USA; 3Department of Pharmaceutical Chemistry, University of were significantly higher in Asian (Po0.001) and Caucasian (Po0.05) liver California San Francisco, San Francisco, CA, USA samples from individuals who were homozygous for g.À2A/A in comparison and 4Department of Pathology and Urology, with those homozygous for the g.À2G/G allele.