Lowering of IOP by Improved Drainage Through the Ciliary Muscle
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Experimental Glaucoma Model with Controllable Intraocular Pressure History Kayla R
www.nature.com/scientificreports OPEN Experimental glaucoma model with controllable intraocular pressure history Kayla R. Ficarrotta1, Youssef H. Mohamed1 & Christopher L. Passaglia1,2* Glaucoma-like neuropathies can be experimentally induced by disturbing aqueous outfow from the eye, resulting in intraocular pressure (IOP) changes that are variable in magnitude and time course and permanent in duration. This study introduces a novel method of glaucoma induction that ofers researchers round-the-clock measurement and reversible control of IOP for the frst time. One eye of Brown-Norway rats was implanted with a cannula tethered to a pressure sensor and aqueous reservoir. IOP was raised 10 mmHg for weeks-to-months in treated animals and unaltered in control animals. Counts of Brn3a-expressing retinal ganglion cells (RGCs) in implanted eyes were indistinguishable from non-implanted eyes in control animals and 15 ± 2%, 23 ± 4%, and 38 ± 4% lower in animals exposed to 2, 4, and 9 weeks of IOP elevation. RGC loss was greater in peripheral retina at 2 weeks and widespread at longer durations. Optic nerves also showed progressive degeneration with exposure duration, yet conventional outfow facility of implanted eyes was normal (24.1 ± 2.9 nl/min/mmHg) even after 9-weeks elevation. Hence, this infusion-based glaucoma model exhibits graded neural damage with unimpaired outfow pathways. The model further revealed a potentially-signifcant fnding that outfow properties of rat eyes do not remodel in response to chronic ocular hypertension. Glaucoma is a heterogeneous group of ocular disorders characterized by progressive and preferential loss of ret- inal ganglion cells (RGCs), resulting in visual feld defcits and ultimately blindness. -

Post-Miosis Changes in the Anterior Chamber Structures in Primary and Lens-Induced Secondary Chronic Angle- Closure Glaucoma
Int J Ophthalmol, Vol. 12, No. 4, Apr.18, 2019 www.ijo.cn Tel: 8629-82245172 8629-82210956 Email: [email protected] ·Brief Report· Post-miosis changes in the anterior chamber structures in primary and lens-induced secondary chronic angle- closure glaucoma Mu Li1, Xiao-Qin Yan1, Gai-Yun Li1,2, Hong Zhang1 1Department of Ophthalmology, Tongji Hospital, Tongji INTRODUCTION Medical College, Huazhong University of Science and laucoma was a leading cause of irreversible blindness Technology, Wuhan 430030, Hubei Province, China G worldwide[1-2], and could be categorized into two types: 2Retinal Department, Shanxi Eye Hospital, Taiyuan 030002, angle-closure glaucoma (ACG) and open angle glaucoma. In Shanxi Province, China Asian, ACG is more prevalent than open angle glaucoma[3-5]. In Co-first authors: Mu Li and Xiao-Qin Yan terms of ACG, it could be divided into primary and secondary Correspondence to: Gai-Yun Li. No.100, Fudong Street, types. For the pathogenesis of primary ACG, besides the Taiyuan 030002, Shanxi Province, China. [email protected]; non-pupillary block mechanisms[6-11], the major mechanism Hong Zhang. No.1095, Jiefang Road, Wuhan 430030, Hubei was pupillary block[12-13]. As an initial option for primary Province, China. [email protected] ACG treatment, miotics could induce the contraction of the Received: 2018-04-13 Accepted: 2018-12-05 sphincter pupillae, which could then pull the peripheral iris away from the trabecular meshwork and therefore reopen Abstract the angle, and finally decrease intraocular pressure (IOP) and ● To evaluate post-miosis changes in the anterior chamber control the progression of glaucoma. -

Affections of Uvea Affections of Uvea
AFFECTIONS OF UVEA AFFECTIONS OF UVEA Anatomy and physiology: • Uvea is the vascular coat of the eye lying beneath the sclera. • It consists of the uvea and uveal tract. • It consists of 3 parts: Iris, the anterior portion; Ciliary body, the middle part; Choroid, the third and the posterior most part. • All the parts of uvea are intimately associated. Iris • It is spongy having the connective tissue stroma, muscular fibers and abundance of vessels and nerves. • It is lined anteriorly by endothelium and posteriorly by a pigmented epithelium. • Its color is because of amount of melanin pigment. Mostly it is brown or golden yellow. • Iris has two muscles; the sphincter which encircles the pupil and has parasympathetic innervation; the dilator which extends from near the sphincter and has sympathetic innervation. • Iris regulates the amount of light admitted to the interior through pupil. • The iris separates the anterior chamber from the posterior chamber of the eye. Ciliary Body: • It extends backward from the base of the iris to the anterior part of the choroid. • It has ciliary muscle and the ciliary processes (70 to 80 in number) which are covered by ciliary epithelium. Choroid: • It is located between the sclera and the retina. • It extends from the ciliaris retinae to the opening of the optic nerve. • It is composed mainly of blood vessels and the pigmented tissue., The pupil • It is circular and regular opening formed by the iris and is larger in dogs in comparison to man. • It contracts or dilates depending upon the light source, due the sphincter and dilator muscles of the iris, respectively. -

Japanese Journal of Ophthalmology Vol.43 No.4
Autonomic Nerves Containing Substance P in the Aqueous Outflow Channels and Scleral Spur of the Guinea Pig Mariko Sasamoto, Hai-Bo Chen and Shigeo Tsukahara Department of Ophthalmology, Yamanashi Medical University, Tamaho, Yamanashi, Japan Purpose: To study the innervation of the aqueous outflow channels and scleral spur by auto- nomic nerves containing substance P. Methods: The experiments were conducted on guinea pigs. Immunohistochemical tech- niques and capsaicin-ablation of the sensory nerves were used to investigate nerves contain- ing substance P at the light and electron microscopic level. Results: Nerves containing substance P were observed in the aqueous outflow channels and scleral spur regions. The fine structures of these nerves had a similar pattern in those regions, and the labeled elements had abundant small vesicles, a few large vesicles, and numerous neurotubuli. Following capsaicin treatment, these nerves remained intact and no degener- ated substance P-like immunoreactive nerves were found. Conclusions: Nerves containing substance P are most likely of autonomic origin in view of their ultrastructural features. These nerves innervate the aqueous outflow channels and scleral spur, and are probably important for neurogenic influences on the intraocular pres- sure by the autonomic nervous system. Jpn J Ophthalmol 1999;43:272–278 © 1999 Japa- nese Ophthalmological Society Key Words: Aqueous outflow channels, capsaicin, guinea pig, immunohistochemistry, substance P. Introduction The scleral spur region should also be considered 4,5 Aqueous outflow channels and the scleral spur because it plays a part in outflow regulation. The human scleral spur contains elastic tissue, similar to play important roles in the regulation of intraocular sclera, so that changes in the IOP might affect these pressure (IOP), and are known to have varied pepti- 5 dergic innervation, which have received special at- tissues. -

Passport to Success
The following terms and other boldface terms in the chapter are defined in the Glossary accommodation choroid After careful study of this chapter, you should be able to: cochlea conjunctiva 1. Describe the function of the sensory system convergence 2. Differentiate between the special and general senses and give examples of each cornea 3. Describe the structure of the eye gustation 4. List and describe the structures that protect the eye lacrimal apparatus 5. Define refraction and list the refractive parts of the eye lens (crystalline lens) 6. Differentiate between the rods and the cones of the eye olfaction 7. Compare the functions of the extrinsic and intrinsic muscles of organ of Corti the eye ossicle 8. Describe the nerve supply to the eye proprioceptor 9. Describe the three divisions of the ear refraction 10. Describe the receptor for hearing and explain how it functions retina 11. Compare static and dynamic equilibrium and describe the sclera location and function of these receptors semicircular canal 12. Explain the function of proprioceptors sensory adaptation 13. List several methods for treatment of pain sensory receptor 14. Describe sensory adaptation and explain its value tympanic membrane 15. Show how word parts are used to build words related to the vestibule sensory system (see Word Anatomy at the end of the chapter) vitreous body PASSport to Success Visit thePoint or see the Student Resource CD in the back of this book for definitions and pronun- ciations of key terms as well as a pretest for this chapter. ® Paul’s Second Case: Seeing More of the Sun’s Effects aul glanced once again at the postcard condition, and it does have a hereditary fac- sitting on his entranceway table as he ar- tor.” The doctor dilated Paul’s eyes with drops Prived home in the evening. -

Ophthalmology Abbreviations Alphabetical
COMMON OPHTHALMOLOGY ABBREVIATIONS Listed as one of America’s Illinois Eye and Ear Infi rmary Best Hospitals for Ophthalmology UIC Department of Ophthalmology & Visual Sciences by U.S.News & World Report Commonly Used Ophthalmology Abbreviations Alphabetical A POCKET GUIDE FOR RESIDENTS Compiled by: Bryan Kim, MD COMMON OPHTHALMOLOGY ABBREVIATIONS A/C or AC anterior chamber Anterior chamber Dilators (red top); A1% atropine 1% education The Department of Ophthalmology accepts six residents Drops/Meds to its program each year, making it one of nation’s largest programs. We are anterior cortical changes/ ACC Lens: Diagnoses/findings also one of the most competitive with well over 600 applicants annually, of cataract whom 84 are granted interviews. Our selection standards are among the Glaucoma: Diagnoses/ highest. Our incoming residents graduated from prestigious medical schools ACG angle closure glaucoma including Brown, Northwestern, MIT, Cornell, University of Michigan, and findings University of Southern California. GPA’s are typically 4.0 and board scores anterior chamber intraocular ACIOL Lens are rarely lower than the 95th percentile. Most applicants have research lens experience. In recent years our residents have gone on to prestigious fellowships at UC Davis, University of Chicago, Northwestern, University amount of plus reading of Iowa, Oregon Health Sciences University, Bascom Palmer, Duke, UCSF, Add power (for bifocal/progres- Refraction Emory, Wilmer Eye Institute, and UCLA. Our tradition of excellence in sives) ophthalmologic education is reflected in the leadership positions held by anterior ischemic optic Nerve/Neuro: Diagno- AION our alumni, who serve as chairs of ophthalmology departments, the dean neuropathy ses/findings of a leading medical school, and the director of the National Eye Institute. -

Tissue-Engineered Models for Glaucoma Research
micromachines Review Tissue-Engineered Models for Glaucoma Research Renhao Lu 1 , Paul A. Soden 2 and Esak Lee 1,* 1 Nancy E. and Peter C. Meinig School of Biomedical Engineering, Cornell University, Ithaca, NY 14853, USA; [email protected] 2 College of Human Ecology, Cornell University, Ithaca, NY 14853, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-607-255-8491 Received: 5 June 2020; Accepted: 22 June 2020; Published: 24 June 2020 Abstract: Glaucoma is a group of optic neuropathies characterized by the progressive degeneration of retinal ganglion cells (RGCs). Patients with glaucoma generally experience elevations in intraocular pressure (IOP), followed by RGC death, peripheral vision loss and eventually blindness. However, despite the substantial economic and health-related impact of glaucoma-related morbidity worldwide, the surgical and pharmacological management of glaucoma is still limited to maintaining IOP within a normal range. This is in large part because the underlying molecular and biophysical mechanisms by which glaucomatous changes occur are still unclear. In the present review article, we describe current tissue-engineered models of the intraocular space that aim to advance the state of glaucoma research. Specifically, we critically evaluate and compare both 2D and 3D-culture models of the trabecular meshwork and nerve fiber layer, both of which are key players in glaucoma pathophysiology. Finally, we point out the need for novel organ-on-a-chip models of glaucoma that functionally integrate currently available 3D models of the retina and the trabecular outflow pathway. Keywords: glaucoma; tissue engineering; trabecular meshwork; Schlemm’s canal; retinal ganglion cell; intraocular pressure; optic nerve head; electrospinning; soft lithography; 3D scaffold; 3D bioprinting 1. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -
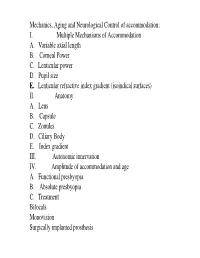
I. Multiple Mechanisms of Accommodation A. Variable Axial Length B
Mechanics, Aging and Neurological Control of accommodation: I. Multiple Mechanisms of Accommodation A. Variable axial length B. Corneal Power C. Lenticular power D. Pupil size E. Lenticular refractive index gradient (isoindical surfaces) II. Anatomy A. Lens B. Capsule C. Zonules D. Ciliary Body E. Index gradient III. Autonomic innervation IV. Amplitude of accommodation and age A. Functional presbyopia B. Absolute presbyopia C. Treatment Bifocals Monovision Surgically implanted prosthesis Course title - (VS217) Oculomotor functions and neurology Instructor - Clifton Schor GSI: James O’Shea, Michael Oliver & Aleks Polosukhina Schedule of lectures, exams and laboratories : Lecture hours 10-11:30 Tu Th; 5 min break at 11:00 Labs Friday the first 3 weeks Examination Schedule : Quizes: January 29; February 28 Midterm: February 14: Final March 13 Power point lecture slides are available on a CD Resources: text books, reader , website, handouts Class Website: Reader. Website http://schorlab.berkeley.edu Click courses 117 class page name VS117 password Hering,1 First Week: read chapters 16-18 See lecture outline in syllabus Labs begin this Friday, January 25 Course Goals Near Response - Current developments in optometry Myopia control – environmental, surgical, pharmaceutical and genetic Presbyopia treatment – amelioration and prosthetic treatment Developmental disorders (amblyopia and strabismus) Reading disorders Ergonomics- computers and sports vision Virtual reality and personal computer eye-ware Neurology screening- Primary care gate keeper neurology, systemic, endocrines, metabolic, muscular skeletal systems. Mechanics, Aging and Neurological Control of accommodation : I. Five Mechanisms of Accommodation A. Variable axial length B. Corneal Power and astigmatism C. Lenticular power D. Pupil size & Aberrations E. Lenticular refractive index gradient (isoindical surfaces) II. -

Eye External Anatomy of Eye Accessory Structures
4/22/16 Eye Bio 40B Dr. Kandula External Anatomy of Eye Accessory Structures l Eyebrows l Levator Palpebrae Superioris - opens eye l Eyelashes l Ciliary glands – modified sweat glands l Small sebaceous glands l Sty is inflamed ciliary glands or small sebaceous glands 1 4/22/16 Terms: Lacrimal gland and duct Surface of eye Lacrimal puncta Lacrimal sac Nasolacrimal duct Nasal cavity Tears / Lacrimal fluid l a watery physiologic saline, with a plasma-like consistency, l contains the bactericidal enzyme lysozyme; l it moistens the conjunctiva and cornea, l provides nutrients and dissolved O2 to the cornea. Extrinsic Muscles of the Eye: Lateral/medial rectus Important to know Superior/inferior rectus actions and nerve Superior/inferior oblique supply in table 2 4/22/16 Extrinsic Eye Muscles • Eye movements controlled by six extrinsic eye muscles Four recti muscles § Superior rectus – moves eyeball superiorly supplied by Cranial Nerve III § Inferior rectus - moves eyeball inferiorly supplied by Cranial Nerve III § Lateral rectus - moves eyeball laterally supplied by Cranial Nerve VI § Medial rectus - moves eyeball medially supplied by Cranial Nerve III Extrinsic Eye Muscles Two oblique muscles rotate eyeball on its axis § Superior oblique rotates eyeball inferiorly and laterally and is supplied by Cranial Nerve IV § Inferior oblique rotates superiorly and laterally and is supplied by Cranial Nerve III Convergence of the Eyes l Binocular vision in humans has both eyes looking at the same object l As you look at an object close to your face, -

Contractile Cells in the Human Scleral Spur
Exp. Eye Res. (1992) 54, 531-543 Contractile Cells in the Human Scleral Spur ERNST TAMM”“, CASSANDRA FLUGEL”, FRITZ H.STEFANIb~~~ JOHANNES W. ROHEN” aDepartment of Anatomy, University of Erlangen- Niirnberg and bEye Hospital of the University of Munich, Germany (Received Lund 75 March 7997 and accepted in revised form 73 June 7997) The scieral spur in 37 human (age 17-87 years) and six cynomolgusmonkey eyes (2-4 years) was investigated. Serial meridional and tangential sections were studied with ultrastructural and immunocytochemicalmethods. The bundlesof the ciliary muscledo not enter the scleralspur, but their tendons, which consistof elasticfibres join the elasticfibres in the scleralspur. Within the scleralspur a populationof circularly oriented and spindle-shapedcells is found. In contrast to the ciliary musclecells, the scleralspur cellsform no bundles,but are looselyaggregated. They have long cytoplasmicprocesses and are connectedto each other by adherens-typeand gap junctions. They stain intensely for a-smooth muscleactin. myosin and vimentin. In contrast to the ciliary musclecells, they do not stain for desmin. Ultrastructurally, the scleral spur cells contain abundant thin (actin) filaments, but do not otherwise show the typical ultrastructural features of ciliary musclecells. The scleral spur cells do not expressa completebasal lamina. They form individual tendinousconnections with the elasticfibres in the scleral spur, which are continuous with the elasticfibres of the trabecular meshwork.The scleralspur cellsare in close contact with nerve terminals containing small agranular (30-60 nm) and large granular (65-l 10 nm) vesiclesbut alsowith terminalscontaining small granular (30-60 nm) vesicleswhich are regardedas typical for adrenergic terminals. We conclude that the scleral spur cells are contractile myofibroblasts.Their contraction might influence the rate of the aqueousoutflow. -

Navigating the Angle: Gonioscopy
4/13/17 Navigating the Angle: Gonioscopy Justin Schweitzer, OD, FAAO Cataract, Cornea, Refractive and Glaucoma Surgery Specialist Vance Thompson Vision Sioux Falls, South DaKota To Participate in Live Polling: • Download “Poll Everywhere” App from your mobile app store • Log on & choose “I’m Participating” • Join PollEv.com/ Or to participate via mobile device without the app, text Cornea to 22333 to join Allergan GlauKos Bausch and Lomb Bio-Tissue Alcon BioTissue Reichert 1 4/13/17 2 4/13/17 How do we view the angle? Direct Lens – use a contact lens with specific anterior curvature that will overcome critical angle Indirect – use a mirror to overcome the critical angle Direct Gonioscopy Koeppe Lens Indirect Gonioscopy Goldmann Three Mirror Zeiss four-mirror lens 3 4/13/17 Gonioscopy The gold standard for assessing the drainage apparatus of the eye CPT code 92020 Gonioscopy Important in distinguishing between different types of glaucoma Open vs Closed angle glaucoma Types of Goniolenses 4 4/13/17 6 mirror lens?!?! 5 4/13/17 SlitS -Lamp Setup 6 4/13/17 Set-up Tips Position mirror at 12:00 Keep gonio lens oriented straight, not tilted Put light on mirror before you go to the oculars Consider resting hand on the patient’s head and using elbow rest if needed Start with Low Mag and Observe Iris Conformation Optical Corneal Wedge 7 4/13/17 How Do We Do It? Angle Anatomy Angle Anatomy Posterior Iris Insertion Ciliary Body (Band) Scleral Spur Trabecular MeshworK Anterior Schwalbe’s Line 8 4/13/17 Ciliary Body (Band) Visibility - Wide Pigmentation Scleral Spur Tr ab ec u l ar Mesh w o r K 9 4/13/17 Schwalbe’s Line Review – Identifying Angle Structures – Two Basic Techniques Posterior Anterior Anterior (Optical Wedge) to Posterior Angle Presentations 10 4/13/17 What Are You Seeing? 11 4/13/17 What Are You Seeing? What Are You Seeing? 12 4/13/17 Recording Your Findings St.