Azelaic Acid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Azelaic Acid
Azelaic Acid (FINACEA) Topical Foam 15% National Drug Monograph August 2016 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a focused drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information Description/Mechanism of Azelaic acid is a naturally occurring C9-dicarboxylic acid that is found in plants Action (such as whole grain cereals), animals and humans. Azelaic acid has antiinflammatory, antioxidative and antikeratinizing effects. In rosacea skin, azelaic acid decreases cathelicidin levels and kallikrein 5 (KLK5) activity and possibly inhibits toll-like receptor 2 (TLR2) expression.1 A 15% gel formulation has been marketed for rosacea, and 20% cream has been available for acne vulgaris. The newer foam formulation consists of an oil- in-water emulsion and was designed to have a higher lipid content than the gel for dry and sensitive skin. Indication(s) Under Review Topical treatment of inflammatory papules and pustules of mild to moderate in This Document rosacea. Dosage Form(s) Under Foam, 15% Review REMS REMS No REMS Postmarketing Requirements See Other Considerations for additional REMS information Pregnancy Rating Category B Executive Summary Efficacy There have been no head-to-head trials comparing the foam and gel formulations of azelaic acid in terms of safety, tolerability and efficacy in the treatment of papulopustular (PP) rosacea.. In two major randomized clinical trials, azelaic acid foam produced small benefits over vehicle foam in achieving Investigator’s Global Assessment (IGA) treatment success (NNTs of 9.2 and 11.5) and in reducing inflammatory lesion counts. -
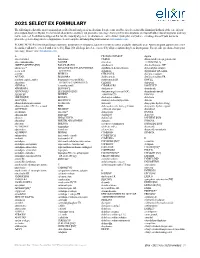
2021 SELECT EX FORMULARY the Following Is a List of the Most Commonly Prescribed Brand and Generic Medications
2021 SELECT EX FORMULARY The following is a list of the most commonly prescribed brand and generic medications. It represents an abbreviated version of the formulary list that is at the core of your prescription drug benefit plan. The list is not all-inclusive and does not guarantee coverage. Some preferred medications overlap with other clinical programs and may not be covered. In addition to drugs on this list, the majority of generic medications are covered under your plan and you are encouraged to ask your doctor to prescribe generic drugs whenever appropriate. Search complete formulary drug information at elixirsolutions.com. PLEASE NOTE: Preferred brand drugs may move to non-preferred status if a generic version becomes available during the year. Any medication approved to enter the market will not be covered until reviewed by Elixir. Not all drugs listed are covered by all prescription drug benefit programs. For specific questions about your coverage, please visit elixirsolutions.com. A B CILOXAN OINTMENT digoxin abacavir tablet balsalazide CIMDUO diltiazem ER (except generics for abacavir-lamivudine BAQSIMI cinacalcet CARDIZEM LA) ABILIFY MAINTENA [INJ] BASAGLAR [INJ] ciprofloxacin dimethyl fumarate DR* abiraterone* BD ULTRAFINE INSULIN SYRINGES ciprofloxacin-dexamethasone diphenoxylate-atropine acetic acid & NEEDLES citalopram dipyridamole ER-aspirin acitretin BELBUCA CITRANATAL divalproex sodium ACUVAIL BELSOMRA clarithromycin divalproex sodium ER acyclovir capsule, tablet benzonatate (except NDCs: clarithromycin ER DIVIGEL -

CVS Formulary Drug Listing
January 2021 Updated 11/01/2020 Performance Drug List - Standard Control The CVS Caremark® Performance Drug List - Standard Control is a guide within select therapeutic categories for clients, plan members and health care providers. Generics should be considered the first line of prescribing. If there is no generic available, there may be more than one brand-name medicine to treat a condition. These preferred brand-name medicines are listed to help identify products that are clinically appropriate and cost-effective. Generics listed in therapeutic categories are for representational purposes only. This is not an all-inclusive list. This list represents brand products in CAPS, branded generics in upper- and lowercase Italics, and generic products in lowercase italics. PLAN MEMBER HEALTH CARE PROVIDER Your benefit plan provides you with a prescription benefit program Your patient is covered under a prescription benefit plan administered administered by CVS Caremark. Ask your doctor to consider by CVS Caremark. As a way to help manage health care costs, prescribing, when medically appropriate, a preferred medicine from authorize generic substitution whenever possible. If you believe a this list. Take this list along when you or a covered family member brand-name product is necessary, consider prescribing a brand name sees a doctor. on this list. Please note: Please note: • Your specific prescription benefit plan design may not cover • Generics should be considered the first line of prescribing. certain products or categories, regardless of their appearance in • The member's prescription benefit plan design may alter coverage this document. Products recently approved by the U.S. Food and of certain products or vary copay1 amounts based on the condition Drug Administration (FDA) may not be covered upon release being treated. -

Supply Issues Update for Primary and Secondary Care: September 2019
COMMERCIAL-SENSITIVE Supply Issues Update for Primary and Secondary Care: September 2019 This report has been produced by the Department of Health and Social Care (DHSC) Medicine Supply Team. We aim to update this report monthly to provide an update on current primary and secondary care medicine supply issues that we are working on. This information is confidential to the NHS; please do not upload to websites in the public domain. Please do share with relevant colleagues and networks. Where it has been stated ‘a clinical memo from UKMI will be published on the SPS website’, this will be found at the following URL: https://www.sps.nhs.uk/category/shortages-discontinuations-and-expiries/ Acetylcholine Chloride (Miochol-E) 20mg Contents powder and solvent for irrigation ..................8 New Issues ............................................................. 3 Aciclovir 500mg/1g injection .........................8 Injectables ......................................................... 3 Amikacin 500mg/2ml injection ......................8 Diamorphine 5mg injection ........................... 3 Emerade 500 microgram and 300 microgram Adrenaline 1 in 1000, 1ml ampoules ............. 4 adrenaline auto-injector (AAI) devices ..........8 Lanoxin (digoxin) 250mcg/ml injection ......... 4 EpiPen and EpiPen Junior ..............................9 Sayana Press (medroxyprogesterone acetate Erwinase injection ..........................................9 104mg) injection ............................................ 5 Haloperidol 5mg/ml injection ........................9 -

Florida Medicaid Brand Drug Preferred List*
FLORIDA MEDICAID BRAND DRUG PREFERRED LIST* Brand Name Generic Name Advair Diskus for inhalation fluticasone/salmeterol diskus Aggrenox capsules aspirin/dipyridamole Albenza tablets albendazole Androgel gel pack/pump** testosterone Avelox tablets** moxifloxacin Azactam vials aztreonam Benicar/Benicar-HCT tablets** olmesartan/olmesartan-HCTZ Bicnu vials carmustine Biltricide tablets praziquantel Butrans patch** buprenorphine transdermal Catapres TTS patch clonidine patch ER Cellcept suspension mycophenolate mofetil Cipro suspension (250mg/5ml & 500mg/5ml) ciprofloxacin Copaxone syringes 20mg glatiramer accetate/Glatopa Derma-Smoothe-FS oil fluocinolone 0.01% oil Differin cream and lotion adapalene erythromycin ethylsuccinate E.E.S. 200mg/5ml suspension - New addition suspension Elidel 1% cream pimecrolimus Emend capsules aprepitant Exelon patch rivastigmine transdermal Finacea GEL 15% azelaic acid Focalin XR capsules dexmethylphenidate hcl Gleevec tablets imatinib Mesylate Glyset tablets miglitol Humalog vial insulin lispro vial Kitabis Pak tobramycin pak Lamictal Dose Pak lamotrigine dose pak Lescol capsules / Lescol XL tablets** fluvastatin ER Letairis tablets** ambrisentan Lialda 1.2g tablets** mesalamine 1.2 g Lotemax 0.5% drops - New addition loteprednol 0.5% drops Makena single dose vial & auto inj** hydroxyprogesterone caproate vial Mephyton tablets phytonadione tablets Micardis and Micardis HCT tablets** telmisartan and telmisartan HCT Natroba suspension spinosad Norvir tablets ritonavir tablets Prevacid ODT lansoprazole ODT Proair -

Aetna Formulary Exclusions Drug List
Covered and non-covered drugs Drugs not covered – and their covered alternatives 2020 Advanced Control Plan – Aetna Formulary Exclusions Drug List 05.03.525.1B (7/20) Below is a list of medications that will not be covered without a Key prior authorization for medical necessity. If you continue using one of these drugs without prior approval, you may be required UPPERCASE Brand-name medicine to pay the full cost. Ask your doctor to choose one of the generic lowercase italics Generic medicine or brand formulary options listed below. Preferred Options For Excluded Medications1 Excluded drug name(s) Preferred option(s) ABILIFY aripiprazole, clozapine, olanzapine, quetiapine, quetiapine ext-rel, risperidone, ziprasidone, VRAYLAR ABSORICA isotretinoin ACANYA adapalene, benzoyl peroxide, clindamycin gel (except NDC^ 68682046275), clindamycin solution, clindamycin-benzoyl peroxide, erythromycin solution, erythromycin-benzoyl peroxide, tretinoin, EPIDUO, ONEXTON, TAZORAC ACIPHEX, esomeprazole, lansoprazole, omeprazole, pantoprazole, DEXILANT ACIPHEX SPRINKLE ACTICLATE doxycycline hyclate capsule, doxycycline hyclate tablet (except doxycycline hyclate tablet 50 mg [NDC^ 72143021160 only], 75 mg, 150 mg), minocycline, tetracycline ACTOS pioglitazone ACUVAIL bromfenac, diclofenac, ketorolac, PROLENSA acyclovir cream acyclovir (except acyclovir cream), valacyclovir ADCIRCA sildenafil, tadalafil ADZENYS XR-ODT amphetamine-dextroamphetamine mixed salts ext-rel†, dexmethylphenidate ext-rel, dextroamphetamine ext-rel, methylphenidate ext-rel†, MYDAYIS, -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Preferred Drug List
October 2021 Preferred Drug List The Preferred Drug List, administered by CVS Caremark® on behalf of Siemens, is a guide within select therapeutic categories for clients, plan members and health care providers. Generics should be considered the first line of prescribing. If there is no generic available, there may be more than one brand-name medicine to treat a condition. These preferred brand-name medicines are listed to help identify products that are clinically appropriate and cost-effective. Generics listed in therapeutic categories are for representational purposes only. This is not an all-inclusive list. This list represents brand products in CAPS, branded generics in upper- and lowercase Italics, and generic products in lowercase italics. PLAN MEMBER HEALTH CARE PROVIDER Your benefit plan provides you with a prescription benefit program Your patient is covered under a prescription benefit plan administered administered by CVS Caremark. Ask your doctor to consider by CVS Caremark. As a way to help manage health care costs, prescribing, when medically appropriate, a preferred medicine from authorize generic substitution whenever possible. If you believe a this list. Take this list along when you or a covered family member brand-name product is necessary, consider prescribing a brand name sees a doctor. on this list. Please note: Please note: • Your specific prescription benefit plan design may not cover • Generics should be considered the first line of prescribing. certain products or categories, regardless of their appearance in • This drug list represents a summary of prescription coverage. It is this document. Products recently approved by the U.S. Food and not all-inclusive and does not guarantee coverage. -

Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act
Updated June 07, 2021 Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act Three categories of bulk drug substances: • Category 1: Bulk Drug Substances Under Evaluation • Category 2: Bulk Drug Substances that Raise Significant Safety Risks • Category 3: Bulk Drug Substances Nominated Without Adequate Support Updates to Categories of Substances Nominated for the 503B Bulk Drug Substances List1 • Add the following entry to category 2 due to serious safety concerns of mutagenicity, cytotoxicity, and possible carcinogenicity when quinacrine hydrochloride is used for intrauterine administration for non- surgical female sterilization: 2,3 o Quinacrine Hydrochloride for intrauterine administration • Revision to category 1 for clarity: o Modify the entry for “Quinacrine Hydrochloride” to “Quinacrine Hydrochloride (except for intrauterine administration).” • Revision to category 1 to correct a substance name error: o Correct the error in the substance name “DHEA (dehydroepiandosterone)” to “DHEA (dehydroepiandrosterone).” 1 For the purposes of the substance names in the categories, hydrated forms of the substance are included in the scope of the substance name. 2 Quinacrine HCl was previously reviewed in 2016 as part of FDA’s consideration of this bulk drug substance for inclusion on the 503A Bulks List. As part of this review, the Division of Bone, Reproductive and Urologic Products (DBRUP), now the Division of Urology, Obstetrics and Gynecology (DUOG), evaluated the nomination of quinacrine for intrauterine administration for non-surgical female sterilization and recommended that quinacrine should not be included on the 503A Bulks List for this use. This recommendation was based on the lack of information on efficacy comparable to other available methods of female sterilization and serious safety concerns of mutagenicity, cytotoxicity and possible carcinogenicity in use of quinacrine for this indication and route of administration. -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act
Updated July 30, 2020 Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act Three categories of bulk drug substances: • Category 1: Bulk Drug Substances Under Evaluation • Category 2: Bulk Drug Substances that Raise Significant Safety Risks • Category 3: Bulk Drug Substances Nominated Without Adequate Support Notice of Updates to Categories of Substances Nominated for the 503B Bulk Drug Substances List • Additions to category 1: Betahistine Hydrochloride L-Proline Citrulline Papaverine Hydrochloride* Copper Gluconate Phosphatidylcholine Diiodohydroxyquinoline Podophyllum Resin Glucosamine Sulfate Potassium Chloride Sodium Molybdate Glucosamine Sulfate Sodium Chloride Sodium Nitroprusside Hydrochloric Acid* Sodium Selenite/Sodium Selenite Pentahydrate* Ibutamoren Mesylate Trichloroacetic Acid* L-Citrulline* Ubidecarenone (Coenzyme Q10)* L-Lysine * Bulk drug substance is currently in Category 3 and is being moved to Category 1. • Minor revision to entry in Category 1 to correct a misspelling: o Correct the misspelling of “cimatidine” to “cimetidine” 1 Updated July 30, 2020 503B Category 1: Bulk Drug Substances Under Evaluation • 5-Methyltetrahydrofolate Calcium • Chromic Chloride • 17-alpha-Hydroxyprogesterone • Chromium chloride/ Chromium Chloride • Acetylcysteine Hexahydrate • Acyclovir • Ciclopirox Oleate • Adapalene • Cimetidine • Adenosine • Ciprofloxacin HCl • Allantoin • Citric Acid Anhydrous • Alpha Lipoic Acid • Citrulline/L-Citrulline • Alprostadil • Clindamycin Phosphate -

List of Formulary Drug Removals
July 2021 Formulary Drug Removals Below is a list of medicines by drug class that have been removed from your plan’s formulary. If you continue using one of the drugs listed below and identified as a Formulary Drug Removal, you may be required to pay the full cost. If you are currently using one of the formulary drug removals, ask your doctor to choose one of the generic or brand formulary options listed below. Category Formulary Drug Formulary Options Drug Class Removals Acromegaly SANDOSTATIN LAR SOMATULINE DEPOT SIGNIFOR LAR SOMAVERT Allergies dexchlorpheniramine levocetirizine Antihistamines Diphen Elixir RyClora CARBINOXAMINE TABLET 6 MG Allergies BECONASE AQ flunisolide spray, fluticasone spray, mometasone spray, DYMISTA Nasal Steroids / Combinations OMNARIS QNASL ZETONNA Anticonvulsants topiramate ext-rel capsule carbamazepine, carbamazepine ext-rel, clobazam, divalproex sodium, (generics for QUDEXY XR only) divalproex sodium ext-rel, gabapentin, lamotrigine, lamotrigine ext-rel, levetiracetam, levetiracetam ext-rel, oxcarbazepine, phenobarbital, phenytoin, phenytoin sodium extended, primidone, rufinamide, tiagabine, topiramate, valproic acid, zonisamide, FYCOMPA, OXTELLAR XR, TROKENDI XR, VIMPAT, XCOPRI BANZEL SUSPENSION clobazam, lamotrigine, rufinamide, topiramate, TROKENDI XR ONFI SABRIL vigabatrin ZONEGRAN carbamazepine, carbamazepine ext-rel, divalproex sodium, divalproex sodium ext-rel, gabapentin, lamotrigine, lamotrigine ext-rel, levetiracetam, levetiracetam ext-rel, oxcarbazepine, phenobarbital, phenytoin, phenytoin sodium