A Case of Abciximab Induced Acute Profound Thrombocytopenia Resulting in Compartment Syndrome of the Forearm from Massive Bleeding at the Brachial Artery Access Site
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Eptifibatide Is Noninferior to Abciximab: Implications for Clinical Practice
RESEARCH HIGHLIGHTS ANTIPLATELET THERAPY Eptifibatide is noninferior to abciximab: implications for clinical practice he glycoprotein IIb/IIIa (GPIIb/ randomized, open, parallel-group January 2004 and December 2007, IIIa) inhibitors eptifibatide and comparison of eptifibatide and abciximab and eptifibatide was used in 2,355 Tabciximab have comparable efficacy in 427 patients presenting within 12 h such procedures over this time frame. and safety in patients with ST-segment of STEMI onset and who underwent During the 1-year follow-up period, elevation myocardial infarction (STEMI) primary PCI. Enrolled patients were from no significant difference was reported undergoing primary percutaneous 22 centers in France and Germany. The for the incidence of death (8.0% and coronary intervention (PCI). These two study drugs were administered in 7.6%), myocardial infarction (9.0% and findings, from a randomized trial and a combination with background therapy 8.4%), or bleeding (2.7% and 3.2%) registry study, are reported in two papers comprising clopidogrel, aspirin, and between abciximab and eptifibatide, published in the Journal of the American heparin or enoxaparin. This study used respectively. Multivariable analysis College of Cardiology (JACC). the surrogate primary end point of showed that eptifibatide was noninferior Platelet aggregation and thrombus complete electrocardiographic ST-segment to abciximab for the prevention of death formation can be inhibited by blocking resolution (STR) 60 min after completion or myocardial infarction (odds ratio 0.94, the GPIIb/IIIa receptor on the platelet of PCI. 95% CI 0.82–1.09). membrane, thereby preventing the binding In the intention-to-treat analysis, These findings “fuel an already much of fibrinogen. -
Deliverable 5.A Interim Report on the Study Results APPENDIX 2
Deliverable 5.a Interim report on the study results APPENDIX 2: Algorithms used to identify study variables for service contract EMA/2011/38/CN ‐ PIOGLITAZONE November 28th 2012 D5.a Interim report on the study results (Appendix 2) for Service Contract EMA/2011/38/CN PIOGLITAZONE Author(s): Vera Ehrenstein (AUH‐AS) APPENDIX 2. ALGORITHMS USED TO IDENTIFY STUDY VARIABLES Algorithms for AU Database DISEASE/CONDITION ICD-8 CODE (1977-1993) ICD-10 CODE (1994-) Diabetes type 2 250.00; 250.06; 250.07; 250.09 E11.0; E11.1; E11.9 Cancer of bladder 188 C67 Haematuria N/A R31 Haematuria, unspecified B18, K70.0–K70.3, K70.9, K71, K73, Mild hepatic impairment 571, 573.01, 573.04 K74, K76.0 Moderate to severe hepatic 070.00, 070.02, 070.04, 070.06, B15.0, B16.0, B16.2, B19.0, K70.4, impairment 070.08, 573.00, 456.00–456.09 K72, K76.6, I85 Acute myocardial infarction 410 I21-I23 Acute coronary syndrome 410, 413 I20-I24 Ischemic heart disease 410-414 I20-I25 427.09, 427.10, 427.11, 427.19, Congestive heart failure I50, I11.0, I13.0,I13.2 428.99, 782.49; Acute renal failure N/A N17 Diabetic coma N/A E10.0, E11.0, E12.0,E13.0, E14.0 Diabetic acidosis N/A E10.1, E11.1, E12.1,E13.1, E14.1 F10.1-F10.9, G31.2, G62.1, G72.1, Alcoholism 291, 303, 577.10, 571.09, 571.10 I42.6, K29.2, K86.0, Z72.1 Obesity 277.99 E65-E66 D5.a Interim report on the study results (Appendix 2) for Service Contract EMA/2011/38/CN PIOGLITAZONE Author(s): Vera Ehrenstein (AUH‐AS) Algorithms for defining acute events in Denmark, ICD-10 code Event ICD-10 code I21.x, I23.x http://apps.who.int/classifications/icd10/browse/2010/en#/I21 -

AHS Provincial High-Alert Medication List
Provincial High-alert Medication List Classes/Categories of Medications Specific Medications adrenergic agonists: IV (e.g., epiNEPHrine, ePHEDrine, isoproterenol, magnesium sulfate injection PHENYLephrine, norepinephrine, doBUTamine, doPAMine, salbutamol) methotrexate: oral for non-oncologic adrenergic antagonists: IV (e.g., propranolol, metoPROLOL, labetalol, use esmolol) nitroprusside sodium for injection anesthetic agents: general, inhaled and IV (e.g., propofol, ketamine, sevoflurane, isoflurane, desflurane, etomidate) opium tincture antiarrhythmics: IV (e.g., lidocaine, amiodarone, procainamide, oxytocin: IV adenosine, bretylium, ibutilide) potassium chloride for injection: antithrombotic agents: concentrate anticoagulants (e.g., warfarin, acenocoumarol, tinzaparin, potassium phosphates injection enoxaparin, dalteparin, danaparoid, unfractionated heparin, sodium citrate) promethazine: IV factor Xa inhibitors (e.g., fondaparinux, rivaroxaban) vasopressin: IV or intraosseous direct thrombin inhibitors (e.g., apixaban, argatroban, bivalirudin, dabigatran) thrombolytics (e.g., alteplase, tenecteplase) glycoprotein IIb/IIIa inhibitors (e.g.,eptifibitide, tirofiban, abciximab) cardioplegic solutions chemotherapeutic agents: parenteral and oral dextrose: 20% or greater (hypertonic) dialysis solutions: peritoneal and hemodialysis The following medications are also epidural or intrathecal medications associated with higher risk and must inotropic medications: IV (e.g., digoxin, milrinone) comply with the segregated storage and labelling -

(12) United States Patent (10) Patent No.: US 8,835,407 B2 Mosher Et Al
US008835407B2 (12) United States Patent (10) Patent No.: US 8,835,407 B2 Mosher et al. (45) Date of Patent: *Sep. 16, 2014 (54) PHARMACEUTICAL COMPOSITIONS 5,324,718 A 6/1994 Loftsson COMPRISING PRASUGREL AND 5,376,645 A 12, 1994 Stella et al. CYCLODEXTRIN DERVATIVES AND 3:3: A .22 seal. METHODS OF MAKING AND USING THE 5576,328 A 1 1/1996 Herbert et al. SAME 5,632,275 A 5/1997 Browne et al. 5,874,418 A 2f1999 Stella et al. (75) Inventors: Gerold L. Mosher, Kansas City, MO 357. A 1 A.28 t al (US), Stephen G. Michatha, Waltham, 6,071,514. A 6/2000 GrinnellCai Ca. et al. MA (US); Daniel J. Cushing, 6,133,248. A 10/2000 Stella Phoenixville, PA (US) 6,153,746 A 1 1/2000 Shah et al. 6,204.256 B1 3/2001 Shalaby et al. (73) Assignee: CyDex Pharmaceuticals, Inc., La Jolla, 6.248,729 B1 6/2001 Coniglio et al. CA (US) 6,294,192 B1 9/2001 Patel et al. 6,383,471 B1 5, 2002 Chen et al. (*) Notice: Subject to any disclaimer, the term of this 6,451,3396,429,210 B2B1 9/20028, 2002 B styletet alal. patent is extended or adjusted under 35 6,504,030 B1 1/2003 Bousquet et al. U.S.C. 154(b) by 0 days. 6,509.348 B1 1/2003 Ogletree 6,569.463 B2 5/2003 Patel et al. This patent is Subject to a terminal dis- 6,573.381 B1 6/2003 Bousquet et al. -

The Efficacy and Safety of Combination Glycoprotein Iibiiia Inhibitors And
Interventional Cardiology The efficacy and safety of combination glycoprotein IIbIIIa inhibitors and reduced-dose thrombolytic therapy–facilitated percutaneous coronary intervention for ST-elevation myocardial infarction: A meta-analysis of randomized clinical trials Mohamad C.N. Sinno, MD, Sanjaya Khanal, MD, FACC, Mouaz H. Al-Mallah, MD, Muhammad Arida, MD, and W. Douglas Weaver, MD Detroit, MI Objective We reviewed the literature and performed a meta-analysis comparing the safety and efficacy of adjunctive use of reduced-dose thrombolytics and glycoprotein (Gp) IIbIIIa inhibitors to the sole use of Gp IIbIIIa inhibitors before percutaneous coronary intervention (PCI) in patients presenting with acute ST-segment elevation myocardial infarction (STEMI). Background Early reperfusion in STEMI is associated with improved outcomes. The use of reduced-dose thrombolytic and Gp IIbIIIa inhibitors combination before PCI in the setting of acute STEMI remains controversial. Methods We performed a literature search and identified randomized trials comparing the use of combination therapy–facilitated PCI versus PCI done with Gp IIbIIIa inhibitor alone. Included studies were reviewed to determine Thrombolysis in Myocardial Infarction (TIMI)-3 flow at baseline, major bleeding, 30-day mortality, TIMI-3 flow after PCI,and 30-day reinfarction. We performed a random-effect model meta-analysis. We quantified heterogeneity between studies with I2. A value N50% represents substantial heterogeneity. Results We identified 4 clinical trials randomizing 725 patients; 424 patients were pretreated with combination therapy before PCI, and 301 patients had Gp IIbIIIa inhibitor alone during PCI. Combination therapy–facilitated PCI was associated with a 2-fold increase in TIMI-3 flow upon arrival to the catheterization laboratory compared with the sole use of upstream Gp IIbIIIa inhibitors (192/390 patients [49%] versus 60/284 [21%]; relative risk [RR], 2.2; P b .00001). -
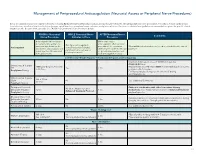
Neuraxial Access Or Peripheral Nerve Procedures)
Management of Periprocedural Anticoagulation (Neuraxial Access or Peripheral Nerve Procedures) Below are guidelines to prevent spinal hematoma following Epidural/Intrathecal/Spinal procedures and perineural hematoma following peripheral nerve procedures. Procedures include epidural injec- tions/infusions, intrathecal injections/infusions/pumps, spinal injections, peripheral nerve catheters, and plexus infusions. Decisions to deviate from guideline recommendations given the specific clinical situation are the decision of the provider. See ‘Additional Comments’ section for more details. PRIOR to Neuraxial/ WHILE Neuraxial/Nerve AFTER Neuraxial/Nerve Comments Nerve Procedure Catheter in Place Procedure How long should I hold prior When can I restart to neuraxial procedure? (i.e. anticoagulants after neuraxial Can I give anticoagulants minimum time between the procedures? (i.e. minimum What additional information do I need to consider for the care of Anticoagulant concurrently with neuraxial, last dose of anticoagulant and time between catheter removal patients? peripheral nerve catheter, or spinal injection OR neuraxial/ or spinal/nerve injection and plexus placement? nerve placement) next anticoagulation dose) Low-Molecular Weight Heparin, Unfractionated Heparin, and Fondaparinux Maximum total heparin dose of 10,000 units per day (5000 SQ Q12 hrs) Unfractionated Heparin 5000 units Q 12 hrs – no time Heparin 5000 units SQ 8 hrs is NOT recommended with concurrent SQ Yes 2 hrs restrictions neuraxial catheter in place Prophylaxis Dosing For IV prophylactic dosing, use ‘treatment’ IV dosing recommendations. Unfractionated Heparin SQ: 8-10 hrs SQ/IV No 2 hrs See ‘Additional Comments’ IV: 4 hrs Treatment Dosing Enoxaparin (Lovenox), Caution in combination with other hemostasis-altering No (Note: May be used for Dalteparin (Fragmin) 12 hrs 4 hrs medications. -

A Aaas. See Abdominal Aortic Aneurysms Aads. See Adjuvant
Index A Acetylsalicylic acid (ASA) treatment, cost-effectiveness of, AAAs. See Abdominal aortic coronary artery spasm, 957 2773, 2775 aneurysms MI, 938 Acute myocardial infarction (AMI), 21. AADs. See Adjuvant antiarrhythmic non-STEMI, 957 See also Non-ST elevation drugs stable angina, 922 acute myocardial infarction; Abciximab, 946, 950, 954 unstable angina, 954, 957 ST elevation acute myocardial AMI, 1024 ACHEIVETM stent, 1037 infarction adjunctive treatment with, 1023 Acquired immunodeficiency syndrome aging and, 2446 CAD, unstable, 1010 (AIDS) anterior wall KD, 986 antiviral therapies for, metabolic V4R value and, 65 non-STEMI, 957, 958 complications of, 2378 occlusions and, 62–64 STEMI, 968 treatment for, 2380 bundle branch block in, 1993–1994, transfusion/blood conservation, 2509 cardiac involvement, prevalence of at 1995 unstable angina, 957 autopsy, 2371–2372 treatment of, 1994 Abdominal aortic aneurysms (AAAs), cardiomyopathy in, 2376–2377 clinical recognition 1644–1648 alternative explanations for, auscultation, 681–683 background and history, 1771 2378–2379 ECG diagnosis, 683 clinical recognition, 1645, 1646–1647 cytokines as possible cause of, inspection and palpation, 679–681 endovascular procedures for 2378 myocardial scintigraphy, 686–687 treatment of drug-induced, 2379 myocardial stunning and patient selection, 1773–1774 myocardial cell injury and, 2378 hibernation, 683 stent grafts, design characteristics cardiovascular involvement in, serum enzyme and cardiac of, 1771–1773 2371–2381 intracellular substance natural history, 1644 PHT and, 2380–2381 changes in, 683–686 surgical repair, 1645–1648 DCM and, 1241–1242 complications of, echocardiography Abdominal disorders, PTE and, 2188 echocardiography and prevalence of and, 815–819 Ablation. See also specific ablations cardiovascular abnormalities coronary heart disease and, 677–691 AF, 1973–1974 in, 2372–2374 differential diagnosis, 687 SND, 1937 health care workers and, 2381 echocardiographic assessment of, ABT-578, DES, 1034 heart neoplasms and, 2272 813–814 ACAD. -

Glycoprotein (GP) Iib/Iiia Receptor Inhibitors for Use in Acute Coronary Syndromes (ACS) & Percutaneous Coronary Intervention (PCI)
Medical Advisory Panel Drug Class Review: Glycoprotein (GP) IIb/IIIa Receptor Inhibitors For Use in Acute Coronary Syndromes (ACS) & Percutaneous Coronary Intervention (PCI) Written by Sara Brouse, Pharm.D., BCPS and Kevin Roberts, BS Pharm., Pharm.D. Purpose: To review the safety, efficacy and administration of the available GP IIb/IIIa receptor inhibitors. I. Indications: 1-4, 37 Currently, there are three glycoprotein (GP) IIb/IIIa receptor inhibitors (Table 1) available in the US. The 2000 ACC/AHA unstable angina and non-ST-segment elevation myocardial infarction (MI) guidelines recommend administration of GP IIb/IIIa receptor inhibitors in patients with non-ST-segment elevation acute coronary syndromes (ACS) at high risk of death or a nonfatal myocardial infarction. Such high-risk features include positive biochemical markers of infarction (ex. troponin I), ST-segment depression on ECG, signs of left ventricular dysfunction, pulmonary edema, age greater than 75 years old, ongoing chest pain for greater than 20 minutes, or ischemia refractory to other medical therapy. Additionally, GP llb/llla inhibitors are utilized for patients who will undergo a percutaneous coronary intervention (PCI), such as balloon angioplasty, atherectomy, or stent implantation during cardiac catheterization. As demonstrated by table 2, only eptifibatide (Integrilin®) has FDA labeled support for both of these clinical indications. Table 1. GP IIb/IIIa Receptor Inhibitors Product Product Availability Product Treatment Cost Manufacturer # Cost (VA)1 Per Day (VA) Abciximab Single use 5ml vial (2 mg/ml) $249 $988* Centocor/ (ReoPro®®®) Eli Lilly Eptifibatide a. 100 ml premixed (750 mcg/ml) a. $97 $292^ COR/Key (Integrilin®®®) b. 10 ml/vial (2000 mcg/ml) b. -

Protocol for Non-Interventional Studies Based on Existing Data TITLE PAGE Document Number: C30445781-01
ABCD Protocol for non-interventional studies based on existing data TITLE PAGE Document Number: c30445781-01 BI Study Number: 1237-0090 BI Investigational Stiolto® Respimat® Product(s): The Role of Inhaler Device in the Treatment Persistence with Dual Title: Bronchodilators in Patients with COPD Protocol version 1.0 identifier: Date of last version of N/A protocol: PASS: No EU PAS register Study not registered number: Olodaterol and Tiotropium Bromide (ATC R03AL06) Active substance: Umeclidinium and Vilanterol (ATC R03AL03) Medicinal product: Stiolto® Respimat®; Anoro® Ellipta® Product reference: N/A Procedure number: N/A Joint PASS: No The primary objective of the study is to use US data to determine relative persistence between Olodaterol/Tiotropium Bromide delivered with the Respimat soft mist inhaler and Umeclidinium/Vilanterol delivered with the Ellipta dry powder inhaler using a 1:2 propensity score matched analysis. The secondary objectives of the study are as follows: Research question and - Characterize new users of Olodaterol/Tiotropium Bromide objectives: and Umeclidinium/Vilanterol in terms of demographics, medication use, comorbidities, and other variables, before and after propensity score matching. - Determine the incidence rate and proportion of patients discontinuing or switching among new users of Olodaterol/Tiotropium Bromide and Umeclidinium/ Vilanterol. - Determine the relative rate and proportion of patients discontinuing between Olodaterol/ Tiotropium Bromide and 001-MCG-102_RD-02 (1.0) / Saved on: 22 Oct 2015 Boehringer Ingelheim Page 2 of 69 Protocol for non-interventional studies based on existing data BI Study Number 1237-0090 c30445781-01 Proprietary confidential information © 2019 Boehringer Ingelheim International GmbH or one or more of its affiliated companies Umeclidinium/Vilanterol. -
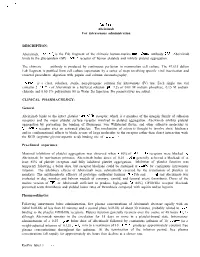
Abciximab for Intravenous Administration
ReoPro@ Abciximab For intravenous administration DESCRIPTION: Abciximab, ReoPro @ , is the Fab fragment of the chimeric human-murine monoclonal antibody 7E3. Abciximab binds to the glycoprotein (GP) IIb/IIIa receptor of human platelets and inhibits platelet aggregation. The chimeric 7E3 antibody is produced by continuous perfusion in mammalian cell culture. The 47,615 dalton Fab fragment is purified from cell culture supematant by a series of steps involving specific viral inactivation and removal procedures, digestion with papain and column chromatography. ReoPro@ is a clear, colorless, sterile, non-pyrogenic solution for intravenous (IV) use. Each single use vial contains 2 mg/mL of Abciximab in a buffered solution (pH 7.2) of 0.01 M sodium phosphate, 0.15 M sodium chloride and 0.00 1% polysorbate 80 in Water for Injection. No preservatives are added. CLINICAL PHARMACOLOGY: General Abciximab binds to the intact platelet GPIIb/IIIa receptor, which is a member of the integrin family of adhesion receptors and the major platelet surface receptor involved in platelet aggregation. Abciximab inhibits platelet aggregation by preventing the binding of fibrinogen, von Willebrand factor, and other adhesive molecules to GPIIb/IIIa receptor sites on activated platelets. The mechanism of action is thought to involve steric hindrance and/or conformational effects to block access of large molecules to the receptor rather than direct interaction with the RGD (arginine-glycine-aspartic acid) binding site of GPIIb/IIIa. Pre-clinical experience Maximal inhibition of platelet aggregation was observed when r: 80% of GPIIb/IIIa receptors were blocked .by Abciximab. In non-human primates, Abciximab bolus doses of 0.25 mg/kg generally achieved a blockade of at least 80% of platelet receptors and fully inhibited platelet aggregation. -

Antithrombotic Reversal – Adult – Inpatient Clinical Practice Guideline
Antithrombotic Reversal – Adult – Inpatient Clinical Practice Guideline Note: Active Table of Contents – Click to follow link EXECUTIVE SUMMARY ........................................................................................................... 3 SCOPE ................................................................................................................................... 4 METHODOLOGY .................................................................................................................... 4 DEFINITIONS.......................................................................................................................... 5 INTRODUCTION ..................................................................................................................... 5 RECOMMENDATIONS ............................................................................................................ 6 UW HEALTH IMPLEMENTATION ........................................................................................... 14 APPENDIX A. EVIDENCE GRADING SCHEME(S) ...................................................................... 15 APPENDIX B. SUMMARY OF INTERIM REVISIONS (AS APPROPRIATE) .. ERROR! BOOKMARK NOT DEFINED. REFERENCES ........................................................................................................................ 21 1 Contact for Content: Name: Anne Rose, PharmD – Pharmacy Department Phone Number: (608) 263-9738 Email Address: [email protected] CPG Contact for Changes: Name: Philip Trapskin, PharmD, -

Abciximab (Reopro®)
Clinical Guideline October 2016 Abciximab (ReoPro®) For Acute Coronary Syndrome (ACS) with Percutaneous Coronary Intervention (PCI) INDICATIONS (See sidebar for contraindications) CONTRAINDICATIONS Abciximab (ReoPro) – used in combination with aspirin and unfractionated heparin (UFH) or Active internal bleeding low molecular weight heparin (LMWH) – is indicated as an adjunct to percutaneous coronary intervention (PCI) for the prevention of cardiac ischemic complications with acute coronary Recent (within 6 weeks) syndrome (ACS). gastrointestinal (GI) or genitourinary (GU) bleeding of clinical significance DOSAGE AND ADMINISTRATION FOR ACS WITH PCI History of CVA within two years, or CVA with a significant residual (Please see page 2 for elective and rescue administration) neurological deficit 1. Start with weight adjusted bolus (see Table 1 below). To administer the bolus, withdraw Bleeding diathesis appropriate amount from undiluted vial and give IV push. Administration of oral 2. Follow bolus with continuous infusion. To mix the maintenance infusion, place anticoagulants within seven days unless prothrombin time is < 1.2 appropriate amount of abciximab (ml) in 250 ml of diluent (D5W or NS.) Mix well. See times control infusion rate based on patient weight in Table 1. Thrombocytopenia 3. Obtain a platelet count 3 hours after starting infusion. (<100,000 cells/μL) Table 1. Abciximab dosing for ACS with PCI Recent (within 6 weeks) major surgery or trauma BOLUS INFUSION Intracranial neoplasm, arteriovenous Patient Amount of Amount