140-239.9 Organ Failure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Safety of Tirofiban for Patients with Acute Ischemic Stroke in Routine Clinical Practice
EXPERIMENTAL AND THERAPEUTIC MEDICINE 10: 169-174, 2015 Safety of tirofiban for patients with acute ischemic stroke in routine clinical practice YUAN-QUN ZHU1, YAN-JUN ZHANG2, HAI-LIN RUAN3, QING LIU2, QIN ZHAN2 and QIONG LI2 1Department of Neurology, Liuzhou Worker's Hospital, The Fourth Affiliated Hospital of Guangxi Medical University, Liuzhou, Guangxi 545005; 2Department of Geriatrics, People's Hospital of Zhengzhou, Zhengzhou, Henan 450003; 3Department of Emergency, Liuzhou Worker's Hospital, The Fourth Affiliated Hospital of Guangxi Medical University, Liuzhou, Guangxi 545005, P.R. China Received April 11, 2014; Accepted December 8, 2014 DOI: 10.3892/etm.2015.2495 Abstract. The aim of the present study was to investigate the Introduction safety of tirofiban alone and in combination with various treat- ments in acute ischemic stroke (AIS). A total of 120 patients Acute ischemic stroke (AIS) is a common cause of morbidity with AIS were included in the study, and these patients were and mortality worldwide. Thrombolysis with recombinant divided into three treatment groups: Group A (tirofiban alone, tissue plasminogen activator (rtPA) is the only proven beneficial n=68), group B (tirofiban plus thrombolytic therapy, n=26), therapy in AIS, and this is received by <2% of patients (1). The and group C (tirofiban as a ‘bridging therapy’, n=26). Risk inaccessibility of this treatment to the majority of patients is due factors, stroke severity, initial imaging, treatment regimens, to a number of factors: A lack of adequate transport facilities complications and long‑term outcomes were analyzed. In and infrastructure, including facilities for thrombolysis in most total, eight patients (6.7%) [six patients (23.1%) in group B centers; the high cost of tPA; and a lack of awareness among and two patients (7.7%) in group C] had hemorrhage during the public and doctors (2). -

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

Summary of the Product Characteristics
Tirofiban hydrochloride Hikma Pharma GmbH SUMMARY OF PRODUCT CHARACTERISTICS 1 NAME OF THE MEDICINAL PRODUCT <TIROFIBAN>® *50 micrograms/mL Solution for infusion <TIROFIBAN>® *250 micrograms/mL Concentrate for solution for infusion 2 QUALITATIVE AND QUANTITATIVE COMPOSITION <TIROFIBAN> Solution: 1 ml of solution for infusion contains 56 micrograms of tirofiban hydrochloride monohydrate which is equivalent to 50 micrograms Tirofiban. This medicinal product contains 31 mmol (or 715 mg) sodium per bag (250 ml). To be taken into consideration by patients on a controlled sodium diet. <TIROFIBAN> Concentrate: 1 ml of concentrate for solution for infusion contains 281 micrograms of tirofiban hydrochloride monohydrate which is equivalent to 250 micrograms Tirofiban. 50 ml of concentrate for solution for infusion contains 14,05 mg of tirofiban hydrochloride monohydrate which is equivalent to 12,5 mg Tirofiban. This medicinal product contains less than 1 mmol sodium (23 mg) per vial (50 ml), i.e. essentially ‘sodium- free’. For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM <TIROFIBAN> Solution: Solution for Infusion (250 ml bag) A clear, colourless solution. <TIROFIBAN> Concentrate: Concentrate for solution for infusion. A clear, colourless concentrated solution. * in the following document the abbreviated terms detailed below are used. • <TIROFIBAN> means <TIROFIBAN> Solution for Infusion or <TIROFIBAN> Concentrate for Solution for Infusion. • <TIROFIBAN> Solution will be used when referring to <TIROFIBAN> Solution for Infusion -

Drotrecogin Alfa (Activated)
PRODUCT MONOGRAPH PrXIGRIS® drotrecogin alfa (activated) Sterile Powder for Intravenous Injection 5 mg or 20 mg drotrecogin alfa (activated) per vial Antithrombotic Profibrinolytic Anti-Inflammatory Enzyme © ELI LILLY CANADA INC. Date of Approval: 3650 Danforth Avenue August 20, 2009 Toronto, Ontario M1N 2E8 1-888-545-5972 www.lilly.ca Submission Control No: 128989 XIGRIS [drotrecogin alfa (activated)] Page 1 of 36 Product Monograph Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION......................................................... 3 SUMMARY PRODUCT INFORMATION ....................................................................... 3 INDICATIONS AND CLINICAL USE............................................................................. 3 CONTRAINDICATIONS .................................................................................................. 4 WARNINGS AND PRECAUTIONS................................................................................. 4 ADVERSE REACTIONS................................................................................................... 8 DRUG INTERACTIONS ................................................................................................. 12 DOSAGE AND ADMINISTRATION ............................................................................. 13 OVERDOSAGE ............................................................................................................... 16 ACTION AND CLINICAL PHARMACOLOGY ........................................................... 16 STORAGE -

Eptifibatide Is Noninferior to Abciximab: Implications for Clinical Practice
RESEARCH HIGHLIGHTS ANTIPLATELET THERAPY Eptifibatide is noninferior to abciximab: implications for clinical practice he glycoprotein IIb/IIIa (GPIIb/ randomized, open, parallel-group January 2004 and December 2007, IIIa) inhibitors eptifibatide and comparison of eptifibatide and abciximab and eptifibatide was used in 2,355 Tabciximab have comparable efficacy in 427 patients presenting within 12 h such procedures over this time frame. and safety in patients with ST-segment of STEMI onset and who underwent During the 1-year follow-up period, elevation myocardial infarction (STEMI) primary PCI. Enrolled patients were from no significant difference was reported undergoing primary percutaneous 22 centers in France and Germany. The for the incidence of death (8.0% and coronary intervention (PCI). These two study drugs were administered in 7.6%), myocardial infarction (9.0% and findings, from a randomized trial and a combination with background therapy 8.4%), or bleeding (2.7% and 3.2%) registry study, are reported in two papers comprising clopidogrel, aspirin, and between abciximab and eptifibatide, published in the Journal of the American heparin or enoxaparin. This study used respectively. Multivariable analysis College of Cardiology (JACC). the surrogate primary end point of showed that eptifibatide was noninferior Platelet aggregation and thrombus complete electrocardiographic ST-segment to abciximab for the prevention of death formation can be inhibited by blocking resolution (STR) 60 min after completion or myocardial infarction (odds ratio 0.94, the GPIIb/IIIa receptor on the platelet of PCI. 95% CI 0.82–1.09). membrane, thereby preventing the binding In the intention-to-treat analysis, These findings “fuel an already much of fibrinogen. -

The Role of Low-Molecular-Weight Heparin in the Management of Acute Coronary Syndromes Marc Cohen, MD, FACC Newark, New Jersey
CORE Metadata, citation and similar papers at core.ac.uk Provided by ElsevierJournal - ofPublisher the American Connector College of Cardiology Vol. 41, No. 4 Suppl S © 2003 by the American College of Cardiology Foundation ISSN 0735-1097/03/$30.00 Published by Elsevier Science Inc. doi:10.1016/S0735-1097(02)02901-7 The Role of Low-Molecular-Weight Heparin in the Management of Acute Coronary Syndromes Marc Cohen, MD, FACC Newark, New Jersey A substantial number of clinical studies have consistently demonstrated that low-molecular- weight heparin (LMWH) compounds are effective and safe alternative anticoagulants to unfractionated heparins (UFHs). They have been found to improve clinical outcomes in acute coronary syndromes and to provide a more predictable therapeutic response, longer and more stable anticoagulation, and a lower incidence of UFH-induced thrombocytopenia. Of the several LMWH agents that have been studied in large clinical trials, including enoxaparin, dalteparin, and nadroparin, not all have shown better efficacy than UFH. Enoxaparin is the only LMWH compound to have demonstrated sustained clinical and economic benefits in comparison with UFH in the management of unstable angina/ non–ST-segment elevation myocardial infarction (NSTEMI). Also, LMWH appears to be a reliable and effective antithrombotic treatment as adjunctive therapy in patients undergoing percutaneous coronary intervention. Clinical trials with enoxaparin indicate that LMWH is effective and safe in this indication, with or without the addition of a glycoprotein IIb/IIIa inhibitor. The efficacy demonstrated by enoxaparin in improving clinical outcomes in unstable angina/NSTEMI patients has led to investigations of its role in the management of ST-segment elevation myocardial infarction. -

Deliverable 5.A Interim Report on the Study Results APPENDIX 2
Deliverable 5.a Interim report on the study results APPENDIX 2: Algorithms used to identify study variables for service contract EMA/2011/38/CN ‐ PIOGLITAZONE November 28th 2012 D5.a Interim report on the study results (Appendix 2) for Service Contract EMA/2011/38/CN PIOGLITAZONE Author(s): Vera Ehrenstein (AUH‐AS) APPENDIX 2. ALGORITHMS USED TO IDENTIFY STUDY VARIABLES Algorithms for AU Database DISEASE/CONDITION ICD-8 CODE (1977-1993) ICD-10 CODE (1994-) Diabetes type 2 250.00; 250.06; 250.07; 250.09 E11.0; E11.1; E11.9 Cancer of bladder 188 C67 Haematuria N/A R31 Haematuria, unspecified B18, K70.0–K70.3, K70.9, K71, K73, Mild hepatic impairment 571, 573.01, 573.04 K74, K76.0 Moderate to severe hepatic 070.00, 070.02, 070.04, 070.06, B15.0, B16.0, B16.2, B19.0, K70.4, impairment 070.08, 573.00, 456.00–456.09 K72, K76.6, I85 Acute myocardial infarction 410 I21-I23 Acute coronary syndrome 410, 413 I20-I24 Ischemic heart disease 410-414 I20-I25 427.09, 427.10, 427.11, 427.19, Congestive heart failure I50, I11.0, I13.0,I13.2 428.99, 782.49; Acute renal failure N/A N17 Diabetic coma N/A E10.0, E11.0, E12.0,E13.0, E14.0 Diabetic acidosis N/A E10.1, E11.1, E12.1,E13.1, E14.1 F10.1-F10.9, G31.2, G62.1, G72.1, Alcoholism 291, 303, 577.10, 571.09, 571.10 I42.6, K29.2, K86.0, Z72.1 Obesity 277.99 E65-E66 D5.a Interim report on the study results (Appendix 2) for Service Contract EMA/2011/38/CN PIOGLITAZONE Author(s): Vera Ehrenstein (AUH‐AS) Algorithms for defining acute events in Denmark, ICD-10 code Event ICD-10 code I21.x, I23.x http://apps.who.int/classifications/icd10/browse/2010/en#/I21 -
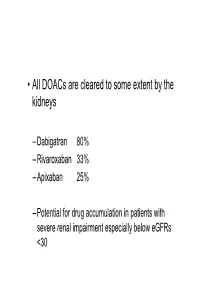
• All Doacs Are Cleared to Some Extent by the Kidneys
• All DOACs are cleared to some extent by the kidneys – Dabigatran 80% – Rivaroxaban 33% – Apixaban 25% – Potential for drug accumulation in patients with severe renal impairment especially below eGFRs <30 Warfarin is unaffected by renal impairment (only • Rivaroxaban & Apixaban are both oral direct inhibitor of factor Xa. • Rivaroxaban doses recommended for clinical use are 15mg od and 20 mg od (15 mg bd for first 3 weeks of treatment of DVT). • Apixaban 5mg bd or 2.5mg bd • Rivaroxaban peak plasma levels are reached 2 to 3 h after ingestion • Apixaban peak plasma levels are reached ~3hrs after ingestion • Rivaroxaban is taken with food – Apixaban without food • Rivaroxaban is 33% renaly excreted and has a half-life of 9 h in patients with normal renal function. – There is an analogy with Therapeutic LMWH – We very rarely ask for an anti-Xa assay • And what is the clinical significance of a Xa assay ? (Cut off values are largely arbitrary) – Fixed doses – Importance of When the last dose was taken ? – Importance of What is the renal function ? – If bleeding • What is the nature of the bleeding ? • In extremis we can give protamine sulphate (? Efficacy) • How to manage bleeding on a DOAC? –How severe is the bleeding ? –When was the last dose of medication ? –What is the renal function ? – Recheck –If minor bleeding; epistaxis, gingival, bruising, menorrhagia • Withhold the NOAC (when was the last dose taken?) • Recheck renal function • Check FBC • Local measures • Unlikely to require further intervention – Re-challenge – ? Switch NOAC -

Low Molecular Weight Heparins and Heparinoids
NEW DRUGS, OLD DRUGS NEW DRUGS, OLD DRUGS Low molecular weight heparins and heparinoids John W Eikelboom and Graeme J Hankey UNFRACTIONATED HEPARIN has been used in clinical ABSTRACT practice for more than 50 years and is established as an effective parenteral anticoagulant for the prevention and ■ Several low molecular weight (LMW) heparin treatment of various thrombotic disorders. However, low preparations, including dalteparin, enoxaparin and molecularThe Medical weight Journal (LMW) of heparinsAustralia haveISSN: recently 0025-729X emerged 7 October as nadroparin, as well as the heparinoid danaparoid sodium, more2002 convenient, 177 6 379-383 safe and effective alternatives to unfrac- are approved for use in Australia. 1 tionated©The heparin Medical (BoxJournal 1). of AustraliaIn Australia, 2002 wwwLMW.mja.com.au heparins are ■ LMW heparins are replacing unfractionated heparin for replacingNew Drugs,unfractionated Old Drugs heparin for preventing and treating the prevention and treatment of venous thromboembolism venous thromboembolism and for the initial treatment of and the treatment of non-ST-segment-elevation acute unstable acute coronary syndromes. The LMW heparinoid coronary syndromes. danaparoid sodium is widely used to treat immune heparin- ■ induced thrombocytopenia. The advantages of LMW heparins over unfractionated heparin include a longer half-life (allowing once-daily or twice-daily subcutaneous dosing), high bioavailability and Limitations of unfractionated heparin predictable anticoagulant response (avoiding the need -
Efficacy Claims and Subset Analyses in Phase III: Some Thoughts and Examples
Efficacy Claims and Subset Analyses in Phase III: Some thoughts and examples Kevin J Carroll My personal views, not AZ’s Why do we do them? • Fundamentally, because we can, and we feel compelled to do so. • Yet, we have no agreed framework for the conduct and interpretation of such analyses, nor for their potential implications on product labelling and drug approval. • Of interest to consider the use and utility of subgroup analyses in confirmatory Phase III trials where such analyses are intended: 1. To provide an assessment of internal ‘consistency’ in an trial with an overall positive outcome. 2. By design to formally assess a hypothesis of efficacy in a predefined subset. 3. To salvage a negative trial. 2 The persuasiveness of subset analyses in confirmatory trials PIII trial Not designed to formally Designed to formally assess efficacy in subset assess efficacy in subset Overall result Overall result Co-primary Subset as part positive negative popln, divided of hierarchical alpha formal confirmatory Multiple Post-hoc • Subset exploratory subsets not testing analyses •Subset +ve procedure subsets identified in weakest of identified in advance • label claim even evidence if overall –ve advance • Extremely •Subset +ve difficult to use • label claim • Subset as basis for •Susbet -ve • Looking for defined in approval. • Overall ‘consistency’ response to positive • Grps that data • May be some • Label claim ‘benefit the most • possibly after very limited possible for / least’ regulatory circumstances overall? • Not a matter of rejection where proving efficacy, • How to conditional but obvious respond to approval can potential to such data? be considered impact on with post- labelling approval commitment 3 1. -

GP Iib/Iiia Adult Cardiology Treatment Dosing and Monitoring Guidelines
GP IIb/IIIa Inhibitor Adult Cardiology Treatment Dosing and Monitoring Guidelines During times of eptifibatide shortage, the following guidance is available for tirofiban usei Eptifibatide (Integrilin®) Tirofiban (Aggrastat®) Dosing Loading dose: 180 mcg/kg IV bolus (max: 22.6 mg) Loading dose: 25 mcg/kg IV over 5 minutes ii ACS Maintenance infusion: 2 mcg/kg/minute (max: 15 mg/hr) up to 72 hours Maintenance infusion: 0.15 mcg/kg/minute continued for up to 18 (until discharge or CABG surgery) hours st 1 Loading dose: 180 mcg/kg IV bolus (max: 22.6 mg) Loading dose: 25 mcg/kg IV over 5 minutes ii PCI Maintenance infusion: 2 mcg/kg/minute (max: 7.5 mg/hr) continued for Maintenance infusion: 0.15 mcg/kg/minute continued for up to 18 up to 18 to 24 hours hours 2nd loading dose: 180 mcg/kg IV bolus (max: 22.6 mg) should be administered 10 minutes after the first bolus Dose Adjustment For CrCl ≤ 50 mL/minute: For CrCl ≤ 60 mL/minute: 1st loading dose: 180 mcg/kg IV bolus (max: 22.6 mg) Loading dose: 25 mcg/kg IV over 5 minutes Maintenance infusion: 2 mcg/kg/minute (max 7.5 mg/hr) Maintenance infusion: 0.075 mcg/kg/minute continued for up to 18 2nd loading dose (if PCI): 180 mcg/kg IV bolus (max: 22.6 mg) should be hours administered 10 minutes after the first bolus For end-stage renal disease: CONTRAINDICATED Contraindications − Severe hypersensitivity reaction to eptifibatide − Severe hypersensitivity reaction to tirofiban − History of bleeding diathesis or evidence of active abnormal bleeding − A history of thrombocytopenia following prior -

Summary of the Product Characteristics
Tirofiban hydrochloride Welding GmbH & Co.KG 1.3 Product Information SUMMARY OF THE PRODUCT CHARACTERISTICS 1 NAME OF THE MEDICINAL PRODUCT <TIROFIBAN>® *50 micrograms/mL Solution for infusion <TIROFIBAN>® *250 micrograms/mL Concentrate for solution for infusion 2 QUALITATIVE AND QUANTITATIVE COMPOSITION <TIROFIBAN> Solution: 1 ml of solution for infusion contains 56 micrograms of Tirofiban hydrochloride monohydrate which is equivalent to 50 micrograms Tirofiban. This medicinal product contains 31 mmol (or 715 mg) sodium per bag (250 ml). To be taken into consideration by patients on a controlled sodium diet. <TIROFIBAN> Concentrate: 1 ml of concentrate for solution for infusion contains 281 micrograms of Tirofiban hydrochloride monohydrate which is equivalent to 250 micrograms Tirofiban. 50 ml of concentrate for solution for infusion contains 70.2514,05 mg of Tirofiban hydrochloride monohydrate which is equivalent to 62.512,5 mg Tirofiban. This medicinal product contains less than 1 mmol sodium (23 mg) per vial (50 ml), i.e. essentially ‘sodium- free’. For excipients, see section 6.1. 3 PHARMACEUTICAL FORM <TIROFIBAN> Solution: Solution for Infusion (250 ml bag) A clear, colourless solution. <TIROFIBAN> Concentrate: Concentrate for solution for infusion. A clear, colourless concentrated solution. * in the following document the abbreviated terms detailed below are used. • <TIROFIBAN> means <TIROFIBAN> Solution for Infusion or <TIROFIBAN> Concentrate for Solution for Infusion. • <TIROFIBAN> Solution will be used when referring to <TIROFIBAN>