Summary of the Product Characteristics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Safety of Tirofiban for Patients with Acute Ischemic Stroke in Routine Clinical Practice
EXPERIMENTAL AND THERAPEUTIC MEDICINE 10: 169-174, 2015 Safety of tirofiban for patients with acute ischemic stroke in routine clinical practice YUAN-QUN ZHU1, YAN-JUN ZHANG2, HAI-LIN RUAN3, QING LIU2, QIN ZHAN2 and QIONG LI2 1Department of Neurology, Liuzhou Worker's Hospital, The Fourth Affiliated Hospital of Guangxi Medical University, Liuzhou, Guangxi 545005; 2Department of Geriatrics, People's Hospital of Zhengzhou, Zhengzhou, Henan 450003; 3Department of Emergency, Liuzhou Worker's Hospital, The Fourth Affiliated Hospital of Guangxi Medical University, Liuzhou, Guangxi 545005, P.R. China Received April 11, 2014; Accepted December 8, 2014 DOI: 10.3892/etm.2015.2495 Abstract. The aim of the present study was to investigate the Introduction safety of tirofiban alone and in combination with various treat- ments in acute ischemic stroke (AIS). A total of 120 patients Acute ischemic stroke (AIS) is a common cause of morbidity with AIS were included in the study, and these patients were and mortality worldwide. Thrombolysis with recombinant divided into three treatment groups: Group A (tirofiban alone, tissue plasminogen activator (rtPA) is the only proven beneficial n=68), group B (tirofiban plus thrombolytic therapy, n=26), therapy in AIS, and this is received by <2% of patients (1). The and group C (tirofiban as a ‘bridging therapy’, n=26). Risk inaccessibility of this treatment to the majority of patients is due factors, stroke severity, initial imaging, treatment regimens, to a number of factors: A lack of adequate transport facilities complications and long‑term outcomes were analyzed. In and infrastructure, including facilities for thrombolysis in most total, eight patients (6.7%) [six patients (23.1%) in group B centers; the high cost of tPA; and a lack of awareness among and two patients (7.7%) in group C] had hemorrhage during the public and doctors (2). -

The Role of Low-Molecular-Weight Heparin in the Management of Acute Coronary Syndromes Marc Cohen, MD, FACC Newark, New Jersey
CORE Metadata, citation and similar papers at core.ac.uk Provided by ElsevierJournal - ofPublisher the American Connector College of Cardiology Vol. 41, No. 4 Suppl S © 2003 by the American College of Cardiology Foundation ISSN 0735-1097/03/$30.00 Published by Elsevier Science Inc. doi:10.1016/S0735-1097(02)02901-7 The Role of Low-Molecular-Weight Heparin in the Management of Acute Coronary Syndromes Marc Cohen, MD, FACC Newark, New Jersey A substantial number of clinical studies have consistently demonstrated that low-molecular- weight heparin (LMWH) compounds are effective and safe alternative anticoagulants to unfractionated heparins (UFHs). They have been found to improve clinical outcomes in acute coronary syndromes and to provide a more predictable therapeutic response, longer and more stable anticoagulation, and a lower incidence of UFH-induced thrombocytopenia. Of the several LMWH agents that have been studied in large clinical trials, including enoxaparin, dalteparin, and nadroparin, not all have shown better efficacy than UFH. Enoxaparin is the only LMWH compound to have demonstrated sustained clinical and economic benefits in comparison with UFH in the management of unstable angina/ non–ST-segment elevation myocardial infarction (NSTEMI). Also, LMWH appears to be a reliable and effective antithrombotic treatment as adjunctive therapy in patients undergoing percutaneous coronary intervention. Clinical trials with enoxaparin indicate that LMWH is effective and safe in this indication, with or without the addition of a glycoprotein IIb/IIIa inhibitor. The efficacy demonstrated by enoxaparin in improving clinical outcomes in unstable angina/NSTEMI patients has led to investigations of its role in the management of ST-segment elevation myocardial infarction. -

GP Iib/Iiia Adult Cardiology Treatment Dosing and Monitoring Guidelines
GP IIb/IIIa Inhibitor Adult Cardiology Treatment Dosing and Monitoring Guidelines During times of eptifibatide shortage, the following guidance is available for tirofiban usei Eptifibatide (Integrilin®) Tirofiban (Aggrastat®) Dosing Loading dose: 180 mcg/kg IV bolus (max: 22.6 mg) Loading dose: 25 mcg/kg IV over 5 minutes ii ACS Maintenance infusion: 2 mcg/kg/minute (max: 15 mg/hr) up to 72 hours Maintenance infusion: 0.15 mcg/kg/minute continued for up to 18 (until discharge or CABG surgery) hours st 1 Loading dose: 180 mcg/kg IV bolus (max: 22.6 mg) Loading dose: 25 mcg/kg IV over 5 minutes ii PCI Maintenance infusion: 2 mcg/kg/minute (max: 7.5 mg/hr) continued for Maintenance infusion: 0.15 mcg/kg/minute continued for up to 18 up to 18 to 24 hours hours 2nd loading dose: 180 mcg/kg IV bolus (max: 22.6 mg) should be administered 10 minutes after the first bolus Dose Adjustment For CrCl ≤ 50 mL/minute: For CrCl ≤ 60 mL/minute: 1st loading dose: 180 mcg/kg IV bolus (max: 22.6 mg) Loading dose: 25 mcg/kg IV over 5 minutes Maintenance infusion: 2 mcg/kg/minute (max 7.5 mg/hr) Maintenance infusion: 0.075 mcg/kg/minute continued for up to 18 2nd loading dose (if PCI): 180 mcg/kg IV bolus (max: 22.6 mg) should be hours administered 10 minutes after the first bolus For end-stage renal disease: CONTRAINDICATED Contraindications − Severe hypersensitivity reaction to eptifibatide − Severe hypersensitivity reaction to tirofiban − History of bleeding diathesis or evidence of active abnormal bleeding − A history of thrombocytopenia following prior -

Summary of the Product Characteristics
Tirofiban hydrochloride Welding GmbH & Co.KG 1.3 Product Information SUMMARY OF THE PRODUCT CHARACTERISTICS 1 NAME OF THE MEDICINAL PRODUCT <TIROFIBAN>® *50 micrograms/mL Solution for infusion <TIROFIBAN>® *250 micrograms/mL Concentrate for solution for infusion 2 QUALITATIVE AND QUANTITATIVE COMPOSITION <TIROFIBAN> Solution: 1 ml of solution for infusion contains 56 micrograms of Tirofiban hydrochloride monohydrate which is equivalent to 50 micrograms Tirofiban. This medicinal product contains 31 mmol (or 715 mg) sodium per bag (250 ml). To be taken into consideration by patients on a controlled sodium diet. <TIROFIBAN> Concentrate: 1 ml of concentrate for solution for infusion contains 281 micrograms of Tirofiban hydrochloride monohydrate which is equivalent to 250 micrograms Tirofiban. 50 ml of concentrate for solution for infusion contains 70.2514,05 mg of Tirofiban hydrochloride monohydrate which is equivalent to 62.512,5 mg Tirofiban. This medicinal product contains less than 1 mmol sodium (23 mg) per vial (50 ml), i.e. essentially ‘sodium- free’. For excipients, see section 6.1. 3 PHARMACEUTICAL FORM <TIROFIBAN> Solution: Solution for Infusion (250 ml bag) A clear, colourless solution. <TIROFIBAN> Concentrate: Concentrate for solution for infusion. A clear, colourless concentrated solution. * in the following document the abbreviated terms detailed below are used. • <TIROFIBAN> means <TIROFIBAN> Solution for Infusion or <TIROFIBAN> Concentrate for Solution for Infusion. • <TIROFIBAN> Solution will be used when referring to <TIROFIBAN> -

Product Monograph
PRODUCT MONOGRAPH Pr AGGRASTAT® tirofiban hydrochloride injection 12.5 mg / 250 mL tirofiban (5 mg / 100 mL in bags of 250 mL) Sterile Solution for Intravenous Infusion only Platelet aggregation inhibitor Cipher Pharmaceuticals Inc. Date of Revision: 2345 Argentia Road, Suite 100A July 24, 2018 Mississauga, Ontario L5N 8K4 Submission Control No.: 218105 AGGRASTAT® - Product Monograph Page 1 of 31 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION ........................................................ 3 SUMMARY PRODUCT INFORMATION........................................................................ 3 INDICATIONS AND CLINICAL USE ............................................................................. 3 CONTRAINDICATIONS ................................................................................................... 3 WARNINGS AND PRECAUTIONS ................................................................................. 4 ADVERSE REACTIONS ................................................................................................... 7 DRUG INTERACTIONS ................................................................................................. 11 DOSAGE AND ADMINISTRATION ............................................................................. 12 OVERDOSAGE ................................................................................................................ 17 ACTION AND CLINICAL PHARMACOLOGY ............................................................ 17 STORAGE AND STABILITY ........................................................................................ -

Intravenous Tirofiban Therapy for Patients with Capsular Warning Syndrome
Open access Original article Stroke Vasc Neurol: first published as 10.1136/svn-2018-000163 on 9 January 2019. Downloaded from Intravenous tirofiban therapy for patients with capsular warning syndrome Wei Li, Ya Wu, Xiao-Shu Li, Cheng-Chun Liu, Shu-Han Huang, Chun-Rong Liang, Huan Wang, Li-Li Zhang, Zhi-Qiang Xu, Yan-Jiang Wang, Meng Zhang To cite: Li W, Wu Y, Li X-S, et al. ABSTRACT Although CWS occurs in only about 1.5% Intravenous tirofiban therapy for Background Capsular warning syndrome (CWS) is defined of patients with transient symptoms, the risk patients with capsular warning as recurrent episodes of transient ischaemic attacks ≥3 syndrome. of developing into a permanent deficit is high Stroke and Vascular times during a short time frame. There is no effective 4 Neurology 2019;4: e000163. and often with poor prognosis. Moreover, therapy to stop these attacks. We, herein, report our doi:10.1136/svn-2018-000163 the frequently recurrent attacks cause signif- experience of using intravenous tirofiban to treat CWS. icant disability and great anxiety to patients ► Additional material is Methods All patients with CWS in our hospital from who experience these episodes. Different published online only. To view January 2013 to September 2017 were reviewed. please visit the journal online Patients in tirofiban group (T-group) were treated by therapies have been proposed, including anti- (http:// dx. doi. org/ 10. 1136/ svn- intravenous tirofiban at 0.4 μg/kg/min for 30 min followed coagulation, antiplatelet therapies and even 2018- 000163). by 0.1–0.15 µg/kg/min infusion. -

GUIDELINE for ANTITHROMBOTIC REVERSAL Table 1
GUIDELINE for ANTITHROMBOTIC REVERSAL This document is intended as a guideline only and should not replace sound clinical judgment Table 1: Reversal for ANTICOAGULANT therapy ANTITHROMBOTIC REVERSAL AGENT COMMENTS DIRECT THROMBIN Short half-life and discontinuation of DTI are primary means of attenuating bleed – Off-label use of INHIBITORS (DTIs) rFVIIa/PCC: support with crystalloid and blood products to facilitate rapid renal clearance of drug – REQUIRES ATTENDING IV: 4 Factor PCC APPROVAL – Argatroban Dose*: 50 units/kg (dose cap at 100 kg to mitigate thrombotic risk) – Document attending – Bivalirudin Administration: Place in empty IV bag and give slow IV push over 10 minutes name in the order (Angiomax®) • Use within 4 hours of reconstitution comments Half-life 10-90 Onset: <30 minutes minutes Caution: thrombotic risk Additional options: PO: – If dabigatran ingested – Dabigatran within 1 hour, consider (Pradaxa®) rFVIIa activated charcoal. Dose*: 100 mcg/kg (dose cap at 100 kg to mitigate thrombotic risk) Half-life 12-17 – Mechanical methods, • May repeat in 2 hours if continued bleeding hours in normal such as dialysis, may be Administration: IV bolus over 3-5 minutes renal function considered as a last • Use within 3 hours of reconstitution resort The aPTT is currently Onset: <30 minutes Caution: thrombotic risk the only readily Recommend not giving available lab test to rFVIIa and PCC together QUALITATIVELY due to high risk of measure dabigatran. thrombosis unless clinical Do not use PT/INR situation warrants FACTOR XA 4 Factor -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

Aggrastat (Tirofiban Hydrochloride Injection Premixed)
® AGGRASTAT (TIROFIBAN HYDROCHLORIDE INJECTION PREMIXED) ® AGGRASTAT (tirofiban HCl) DESCRIPTION AGGRASTAT* (tirofiban hydrochloride), a non-peptide antagonist of the platelet glycoprotein (GP) IIb/IIIa receptor, inhibits platelet aggregation. Tirofiban hydrochloride monohydrate, a non-peptide molecule, is chemically described as N(butylsulfonyl)-O-[4-(4-piperidinyl)butyl]-L-tyrosine monohydrochloride monohydrate. Its molecular formula is C22H36N2O5S•HCI•H2O and its structural formula is: • HCI • H2 O CH 2 COOH C H NHSO 2CH 2CH 2CH 2CH 3 HN CH 2CH 2 CH2 CH 2O Tirofiban hydrochloride monohydrate is a white to off-white, non-hygroscopic, free- flowing powder, with a molecular weight of 495.08. It is very slightly soluble in water. AGGRASTAT Injection Premixed is supplied as a sterile solution in water for injection, for intravenous use only, in plastic containers of 100 mL or 250 mL. Each 100 mL of the premixed, iso-osmotic intravenous injection contains 5.618 mg tirofiban hydrochloride monohydrate equivalent to 5 mg tirofiban (50 mcg/mL) and the following inactive ingredients: 0.9 g sodium chloride, 54 mg sodium citrate dihydrate, and 3.2 mg citric acid anhydrous. Each 250 mL of the premixed, iso-osmotic intravenous injection contains 14.045 mg tirofiban hydrochloride monohydrate equivalent to 12.5 mg tirofiban (50 mcg/mL) and the following inactive ingredients: 2.25 g sodium chloride, 135 mg sodium citrate dihydrate, and 8 mg citric acid anhydrous. The pH of the solution ranges from 5.5 to 6.5 and may have been adjusted with hydrochloric acid and/or sodium hydroxide. The flexible container is manufactured from a specially designed multilayer plastic (PL 2408). -
Neuraxial Access Or Peripheral Nerve Procedures)
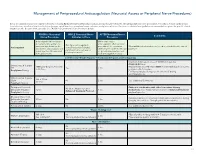
Management of Periprocedural Anticoagulation (Neuraxial Access or Peripheral Nerve Procedures) Below are guidelines to prevent spinal hematoma following Epidural/Intrathecal/Spinal procedures and perineural hematoma following peripheral nerve procedures. Procedures include epidural injec- tions/infusions, intrathecal injections/infusions/pumps, spinal injections, peripheral nerve catheters, and plexus infusions. Decisions to deviate from guideline recommendations given the specific clinical situation are the decision of the provider. See ‘Additional Comments’ section for more details. PRIOR to Neuraxial/ WHILE Neuraxial/Nerve AFTER Neuraxial/Nerve Comments Nerve Procedure Catheter in Place Procedure How long should I hold prior When can I restart to neuraxial procedure? (i.e. anticoagulants after neuraxial Can I give anticoagulants minimum time between the procedures? (i.e. minimum What additional information do I need to consider for the care of Anticoagulant concurrently with neuraxial, last dose of anticoagulant and time between catheter removal patients? peripheral nerve catheter, or spinal injection OR neuraxial/ or spinal/nerve injection and plexus placement? nerve placement) next anticoagulation dose) Low-Molecular Weight Heparin, Unfractionated Heparin, and Fondaparinux Maximum total heparin dose of 10,000 units per day (5000 SQ Q12 hrs) Unfractionated Heparin 5000 units Q 12 hrs – no time Heparin 5000 units SQ 8 hrs is NOT recommended with concurrent SQ Yes 2 hrs restrictions neuraxial catheter in place Prophylaxis Dosing For IV prophylactic dosing, use ‘treatment’ IV dosing recommendations. Unfractionated Heparin SQ: 8-10 hrs SQ/IV No 2 hrs See ‘Additional Comments’ IV: 4 hrs Treatment Dosing Enoxaparin (Lovenox), Caution in combination with other hemostasis-altering No (Note: May be used for Dalteparin (Fragmin) 12 hrs 4 hrs medications. -

Rescue Treatment with Intra-Arterial Tirofiban Infusion and Emergent Carotid Stenting
Yonsei Med J 49(5):857 - 859, 2008 DOI 10.3349/ymj.2008.49.5.857 Rescue Treatment with Intra-arterial Tirofiban Infusion and Emergent Carotid Stenting Tae Jin Song,1 Kee Oog Lee,1 Dong Joon Kim,2 and Kyung-Yul Lee1 Departments of 1Neurology and 2Diagnostic Radiology, Yonsei University College of Medicine, Seoul, Korea. Rapid arterial rethrombosis is associated with high-grade role in such rethrombosis following thrombolytic- residual stenosis and usually occurs at the site of the initial induced clot lysis. occlusion, resulting in reocclusion of the recanalized artery. Glycoprotein (GP) IIb/IIIa receptor blockers Platelets may play an active role in such rethrombosis after prevent thrombus formation by inhibiting the thrombolytic-induced clot lysis. Given that glycoprotein IIb/IIIa receptor blockers, like tirofiban, prevent thrombus final common pathway of platelet aggregation. formation by inhibiting the final common pathway of platelet There are three GP IIb/IIIa receptor blockers aggregation, they may be helpful for treating rethrombosis (abciximab, tirofiban, eptifibatide) available for after thrombolysis. A 64-year-old man presented with an acute clinical use. There are significant differences in the ischemic stroke due to internal carotid artery (ICA) occlusion. biological and plasma half-lives of abciximab and The ICA was recanalized by intravenous thrombolysis but the small molecule agents (tirofiban and eptifi- reoccluded shortly after recanalization. The reoccluded ICA batide). Tirofiban is a small, non-peptide molecule was successfully recanalized using intra-arterial tirofiban. A carotid stent was subsequently inserted to relieve severe that has been used intravenously, in combination stenosis and to prevent recurrent stroke. -

Glycoprotein (GP) Iib/Iiia Receptor Inhibitors for Use in Acute Coronary Syndromes (ACS) & Percutaneous Coronary Intervention (PCI)
Medical Advisory Panel Drug Class Review: Glycoprotein (GP) IIb/IIIa Receptor Inhibitors For Use in Acute Coronary Syndromes (ACS) & Percutaneous Coronary Intervention (PCI) Written by Sara Brouse, Pharm.D., BCPS and Kevin Roberts, BS Pharm., Pharm.D. Purpose: To review the safety, efficacy and administration of the available GP IIb/IIIa receptor inhibitors. I. Indications: 1-4, 37 Currently, there are three glycoprotein (GP) IIb/IIIa receptor inhibitors (Table 1) available in the US. The 2000 ACC/AHA unstable angina and non-ST-segment elevation myocardial infarction (MI) guidelines recommend administration of GP IIb/IIIa receptor inhibitors in patients with non-ST-segment elevation acute coronary syndromes (ACS) at high risk of death or a nonfatal myocardial infarction. Such high-risk features include positive biochemical markers of infarction (ex. troponin I), ST-segment depression on ECG, signs of left ventricular dysfunction, pulmonary edema, age greater than 75 years old, ongoing chest pain for greater than 20 minutes, or ischemia refractory to other medical therapy. Additionally, GP llb/llla inhibitors are utilized for patients who will undergo a percutaneous coronary intervention (PCI), such as balloon angioplasty, atherectomy, or stent implantation during cardiac catheterization. As demonstrated by table 2, only eptifibatide (Integrilin®) has FDA labeled support for both of these clinical indications. Table 1. GP IIb/IIIa Receptor Inhibitors Product Product Availability Product Treatment Cost Manufacturer # Cost (VA)1 Per Day (VA) Abciximab Single use 5ml vial (2 mg/ml) $249 $988* Centocor/ (ReoPro®®®) Eli Lilly Eptifibatide a. 100 ml premixed (750 mcg/ml) a. $97 $292^ COR/Key (Integrilin®®®) b. 10 ml/vial (2000 mcg/ml) b.