A Aaas. See Abdominal Aortic Aneurysms Aads. See Adjuvant
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Eptifibatide Is Noninferior to Abciximab: Implications for Clinical Practice
RESEARCH HIGHLIGHTS ANTIPLATELET THERAPY Eptifibatide is noninferior to abciximab: implications for clinical practice he glycoprotein IIb/IIIa (GPIIb/ randomized, open, parallel-group January 2004 and December 2007, IIIa) inhibitors eptifibatide and comparison of eptifibatide and abciximab and eptifibatide was used in 2,355 Tabciximab have comparable efficacy in 427 patients presenting within 12 h such procedures over this time frame. and safety in patients with ST-segment of STEMI onset and who underwent During the 1-year follow-up period, elevation myocardial infarction (STEMI) primary PCI. Enrolled patients were from no significant difference was reported undergoing primary percutaneous 22 centers in France and Germany. The for the incidence of death (8.0% and coronary intervention (PCI). These two study drugs were administered in 7.6%), myocardial infarction (9.0% and findings, from a randomized trial and a combination with background therapy 8.4%), or bleeding (2.7% and 3.2%) registry study, are reported in two papers comprising clopidogrel, aspirin, and between abciximab and eptifibatide, published in the Journal of the American heparin or enoxaparin. This study used respectively. Multivariable analysis College of Cardiology (JACC). the surrogate primary end point of showed that eptifibatide was noninferior Platelet aggregation and thrombus complete electrocardiographic ST-segment to abciximab for the prevention of death formation can be inhibited by blocking resolution (STR) 60 min after completion or myocardial infarction (odds ratio 0.94, the GPIIb/IIIa receptor on the platelet of PCI. 95% CI 0.82–1.09). membrane, thereby preventing the binding In the intention-to-treat analysis, These findings “fuel an already much of fibrinogen. -

(12) United States Patent (10) Patent No.: US 8,697,347 B2
USOO8697347B2 (12) UnitedO States Patent (10) Patent No.: US 8,697,347 B2 Sehgal (45) Date of Patent: *Apr. 15, 2014 (54) COMPOSITION FOR PRESERVING OTHER PUBLICATIONS PLATELETS AND METHOD OF USING THE SAME Furman et al., “GPllb-Illa Antagonist-induced Reduction in Platelet Surface Factor ViVa Binding and Phosphatidylserine Expression in (75) Inventor: Lakshman R. Sehgal, Monarch Beach, Whole Blood”. Thromb. Haemost. 84: 492-8 (2000).* CA (US) Uzan, 'Antithrombotic agents'. Chapter 12, Emerging Drugs 3 : 189-208 (1998).* (73) Assignee: Biovec Transfusion, LLC, Chicago, IL Agranenko et al., “Preparing platelet concentrates from banked blood (US) stored for 1-5 days by using tetracycline antibiotics”. Folia Haematologica 110 (6): 879-86 (1982), abstract only.* ( c ) Notice: Subject to any disclaimer, the term of this International Search Report (Application No. PCT/US2003/038.125, patent is extended or adjusted under 35 filed Dec. 2, 2003). U.S.C. 154(b) by 300 days. Abendschein. D.R., et al., “Effects of ZK-807834, a Novel Inhibitor of Factor Xa, on Arterial and Venous Thrombosis in Rabbits', J. This patent is Subject to a terminal dis- Cardiovasc. Pharmacol., vol. 35. No. 5, pp. 796-805, retrieved Oct. claimer. 11, 2006, <http:\\gateway.ut.ovid.com.gwllovidweb.cgi>, May 2000. (21) Appl. No.: 13/098,128 Ostrem, JA, et al., “Discovery of a Novel, Potent, and Specific Family of Factor Xa Inhibitors via Combinatorial Chemistry, Biochemistry, (22) Filed: Apr. 29, 2011 vol. 37, No. 4, pp. 1053-1059, 1998. Hirsh, J. et al., “New antithrombotic agents'. The Lancet, vol. 353, (65) Prior Publication Data pp. -

Deliverable 5.A Interim Report on the Study Results APPENDIX 2
Deliverable 5.a Interim report on the study results APPENDIX 2: Algorithms used to identify study variables for service contract EMA/2011/38/CN ‐ PIOGLITAZONE November 28th 2012 D5.a Interim report on the study results (Appendix 2) for Service Contract EMA/2011/38/CN PIOGLITAZONE Author(s): Vera Ehrenstein (AUH‐AS) APPENDIX 2. ALGORITHMS USED TO IDENTIFY STUDY VARIABLES Algorithms for AU Database DISEASE/CONDITION ICD-8 CODE (1977-1993) ICD-10 CODE (1994-) Diabetes type 2 250.00; 250.06; 250.07; 250.09 E11.0; E11.1; E11.9 Cancer of bladder 188 C67 Haematuria N/A R31 Haematuria, unspecified B18, K70.0–K70.3, K70.9, K71, K73, Mild hepatic impairment 571, 573.01, 573.04 K74, K76.0 Moderate to severe hepatic 070.00, 070.02, 070.04, 070.06, B15.0, B16.0, B16.2, B19.0, K70.4, impairment 070.08, 573.00, 456.00–456.09 K72, K76.6, I85 Acute myocardial infarction 410 I21-I23 Acute coronary syndrome 410, 413 I20-I24 Ischemic heart disease 410-414 I20-I25 427.09, 427.10, 427.11, 427.19, Congestive heart failure I50, I11.0, I13.0,I13.2 428.99, 782.49; Acute renal failure N/A N17 Diabetic coma N/A E10.0, E11.0, E12.0,E13.0, E14.0 Diabetic acidosis N/A E10.1, E11.1, E12.1,E13.1, E14.1 F10.1-F10.9, G31.2, G62.1, G72.1, Alcoholism 291, 303, 577.10, 571.09, 571.10 I42.6, K29.2, K86.0, Z72.1 Obesity 277.99 E65-E66 D5.a Interim report on the study results (Appendix 2) for Service Contract EMA/2011/38/CN PIOGLITAZONE Author(s): Vera Ehrenstein (AUH‐AS) Algorithms for defining acute events in Denmark, ICD-10 code Event ICD-10 code I21.x, I23.x http://apps.who.int/classifications/icd10/browse/2010/en#/I21 -

Antithrombotic Treatment After Stroke Due to Intracerebral Haemorrhage (Review)
Cochrane Database of Systematic Reviews Antithrombotic treatment after stroke due to intracerebral haemorrhage (Review) Perry LA, Berge E, Bowditch J, Forfang E, Rønning OM, Hankey GJ, Villanueva E, Al-Shahi Salman R Perry LA, Berge E, Bowditch J, Forfang E, Rønning OM, Hankey GJ, Villanueva E, Al-Shahi Salman R. Antithrombotic treatment after stroke due to intracerebral haemorrhage. Cochrane Database of Systematic Reviews 2017, Issue 5. Art. No.: CD012144. DOI: 10.1002/14651858.CD012144.pub2. www.cochranelibrary.com Antithrombotic treatment after stroke due to intracerebral haemorrhage (Review) Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 SUMMARY OF FINDINGS FOR THE MAIN COMPARISON . ..... 3 BACKGROUND .................................... 5 OBJECTIVES ..................................... 5 METHODS ...................................... 6 RESULTS....................................... 8 Figure1. ..................................... 9 Figure2. ..................................... 11 Figure3. ..................................... 12 DISCUSSION ..................................... 14 AUTHORS’CONCLUSIONS . 15 ACKNOWLEDGEMENTS . 15 REFERENCES ..................................... 15 CHARACTERISTICSOFSTUDIES . 18 DATAANDANALYSES. 31 Analysis 1.2. Comparison 1 Short-term antithrombotic treatment, Outcome 2 Death. 31 Analysis 1.6. Comparison 1 Short-term antithrombotic -

AHS Provincial High-Alert Medication List
Provincial High-alert Medication List Classes/Categories of Medications Specific Medications adrenergic agonists: IV (e.g., epiNEPHrine, ePHEDrine, isoproterenol, magnesium sulfate injection PHENYLephrine, norepinephrine, doBUTamine, doPAMine, salbutamol) methotrexate: oral for non-oncologic adrenergic antagonists: IV (e.g., propranolol, metoPROLOL, labetalol, use esmolol) nitroprusside sodium for injection anesthetic agents: general, inhaled and IV (e.g., propofol, ketamine, sevoflurane, isoflurane, desflurane, etomidate) opium tincture antiarrhythmics: IV (e.g., lidocaine, amiodarone, procainamide, oxytocin: IV adenosine, bretylium, ibutilide) potassium chloride for injection: antithrombotic agents: concentrate anticoagulants (e.g., warfarin, acenocoumarol, tinzaparin, potassium phosphates injection enoxaparin, dalteparin, danaparoid, unfractionated heparin, sodium citrate) promethazine: IV factor Xa inhibitors (e.g., fondaparinux, rivaroxaban) vasopressin: IV or intraosseous direct thrombin inhibitors (e.g., apixaban, argatroban, bivalirudin, dabigatran) thrombolytics (e.g., alteplase, tenecteplase) glycoprotein IIb/IIIa inhibitors (e.g.,eptifibitide, tirofiban, abciximab) cardioplegic solutions chemotherapeutic agents: parenteral and oral dextrose: 20% or greater (hypertonic) dialysis solutions: peritoneal and hemodialysis The following medications are also epidural or intrathecal medications associated with higher risk and must inotropic medications: IV (e.g., digoxin, milrinone) comply with the segregated storage and labelling -

(12) United States Patent (10) Patent No.: US 6,518,244 B2 Cardin Et Al
USOO651824.4B2 (12) United States Patent (10) Patent No.: US 6,518,244 B2 Cardin et al. (45) Date of Patent: Feb. 11, 2003 (54) COMBINATIONS OF HEPARIN COFACTOR OTHER PUBLICATIONS II AGONIST AND PLATELET IIB/IIIA Nicolini et al. Chem. Abst. 121:170,096 (1994).* ANTAGONIST, AND USES THEREOF Pavao et al., “A Unique Dermatan Sulfate-Like Glycosami noglycan from Ascidian,” J. Biol. Chem., (Dec. 29, 1995) (75) Inventors: Alan D. Cardin, Cincinnati, OH (US); 270(52):31027-31036. Cornelius L. Van Gorp, Springboro, Pouplard et al., “Antibodies to Platelet Factor 4-Heparin OH (US) After Cardiopulmonary Bypass in Patients Anticoagulated with Unfractionated Heparin or a Low Molecular Weight (73) Assignee: IntimaX Corporation, Cincinnati, OH Heparin:clinical Implications for Heparin-Induced Throm (US) bocytopenia.” Circulation (1999) 99:2539-2536. Prandoni et al., “Dermatan Sulfate: a Safe Approach to Notice: Subject to any disclaimer, the term of this Prevention of Postoperative Deep Vein Thrombosis,” Br. J. patent is extended or adjusted under 35 Surg. (1992) 79(6):505–509. U.S.C. 154(b) by 57 days. Adgey, “Bleeding Complications with New Antithrombotics Used in Ischemic Heart Disease,” Haemostasis (1996) 26(5):237-246. Agnelli et al., “A Randomized Double-Blind, Placebo-Con (21) Appl. No.: 09/802,775 trolled Trial of Dermatan Sulphate for Prevention of Deep (22) Filed: Mar. 9, 2001 Vein Thrombosis in Hip Fracture.” Thromb. Haemostas. (1992) 67:203-208. (65) Prior Publication Data Agnelli, “New Antithrombins and Nonheparin Glycosami noglycans in Clinical Development,” Vessels (1995) 1:9-16. US 2001/0036932 A1 Nov. 1, 2001 Ali et al., “Diffuse Alveolar Hemorrhage Following Admin istration of Tirofiban or Abciximab: a Nemesis of Platelet Related U.S. -
Antithrombotic Agents in the Management of Sepsis
Antithrombotic Agents in the Management of Sepsis !"#$ Loyola University Medical Center, Maywood, Illinois-60153, USA ABSTRACT Sepsis, a systemic inflammatory syndrome, is a response to infection and when associated with mul- tiple organ dysfunction is termed, severe sepsis. It remains a leading cause of mortality in the critically ill. The response to the invading bacteria may be considered as a balance between proinflammatory and antiinflammatory reaction. While an inadequate proinflammatory reaction and a strong antiinflammatory response could lead to overwhelming infection and death of the patient, a strong and uncontrolled pro- inflammatory response, manifested by the release of proinflammatory mediators may lead to microvas- cular thrombosis and multiple organ failure. Endotoxin triggers sepsis by releasing various mediators inc- luding tumor necrosis factor-alpha and interleukin-1(IL-1). These cytokines activate the complement and coagulation systems, release adhesion molecules, prostaglandins, leukotrienes, reactive oxygen speci- es and nitric oxide (NO). Other mediators involved in the sepsis syndrome include IL-1, IL-6 and IL-8; arachidonic acid metabolites; platelet activating factor (PAF); histamine; bradykinin; angiotensin; comp- lement components and vasoactive intestinal peptide. These proinflammatory responses are counterac- ted by IL-10. Most of the trials targeting the different mediators of proinflammatory response have failed due a lack of correct definition of sepsis. Understanding the exact pathophysiology of the disease will enable better treatment options. Targeting the coagulation system with various anticoagulant agents inc- luding antithrombin, activated protein C (APC), tissue factor pathway inhibitor (TFPI) is a rational appro- ach. Many clinical trials have been conducted to evaluate these agents in severe sepsis. -

(12) United States Patent (10) Patent No.: US 8,835,407 B2 Mosher Et Al
US008835407B2 (12) United States Patent (10) Patent No.: US 8,835,407 B2 Mosher et al. (45) Date of Patent: *Sep. 16, 2014 (54) PHARMACEUTICAL COMPOSITIONS 5,324,718 A 6/1994 Loftsson COMPRISING PRASUGREL AND 5,376,645 A 12, 1994 Stella et al. CYCLODEXTRIN DERVATIVES AND 3:3: A .22 seal. METHODS OF MAKING AND USING THE 5576,328 A 1 1/1996 Herbert et al. SAME 5,632,275 A 5/1997 Browne et al. 5,874,418 A 2f1999 Stella et al. (75) Inventors: Gerold L. Mosher, Kansas City, MO 357. A 1 A.28 t al (US), Stephen G. Michatha, Waltham, 6,071,514. A 6/2000 GrinnellCai Ca. et al. MA (US); Daniel J. Cushing, 6,133,248. A 10/2000 Stella Phoenixville, PA (US) 6,153,746 A 1 1/2000 Shah et al. 6,204.256 B1 3/2001 Shalaby et al. (73) Assignee: CyDex Pharmaceuticals, Inc., La Jolla, 6.248,729 B1 6/2001 Coniglio et al. CA (US) 6,294,192 B1 9/2001 Patel et al. 6,383,471 B1 5, 2002 Chen et al. (*) Notice: Subject to any disclaimer, the term of this 6,451,3396,429,210 B2B1 9/20028, 2002 B styletet alal. patent is extended or adjusted under 35 6,504,030 B1 1/2003 Bousquet et al. U.S.C. 154(b) by 0 days. 6,509.348 B1 1/2003 Ogletree 6,569.463 B2 5/2003 Patel et al. This patent is Subject to a terminal dis- 6,573.381 B1 6/2003 Bousquet et al. -

Undergoing Elective Angioplasty in Patients with Stable Coronary Artery
Downloaded from heart.bmjjournals.com on 17 October 2006 Pharmacodynamics and safety of lefradafiban, an oral platelet glycoprotein IIb/IIIa receptor antagonist, in patients with stable coronary artery disease undergoing elective angioplasty K M Akkerhuis, M J B M van den Brand, C van der Zwaan, H O J Peels, H Suryapranata, L R van der Wieken, J Stibbe, J Hoffmann, T Baardman, J W Deckers and M L Simoons Heart 2001;85;444-450 doi:10.1136/heart.85.4.444 Updated information and services can be found at: http://heart.bmjjournals.com/cgi/content/full/85/4/444 These include: References This article cites 27 articles, 17 of which can be accessed free at: http://heart.bmjjournals.com/cgi/content/full/85/4/444#BIBL 1 online articles that cite this article can be accessed at: http://heart.bmjjournals.com/cgi/content/full/85/4/444#otherarticles Rapid responses You can respond to this article at: http://heart.bmjjournals.com/cgi/eletter-submit/85/4/444 Email alerting Receive free email alerts when new articles cite this article - sign up in the box at the service top right corner of the article Topic collections Articles on similar topics can be found in the following collections Drugs: cardiovascular system (857 articles) Ischemic heart disease (2078 articles) Notes To order reprints of this article go to: http://www.bmjjournals.com/cgi/reprintform To subscribe to Heart go to: http://www.bmjjournals.com/subscriptions/ Downloaded from heart.bmjjournals.com on 17 October 2006 444 Heart 2001;85:444–450 Pharmacodynamics and safety of lefradafiban, an oral platelet glycoprotein IIb/IIIa receptor antagonist, in patients with stable coronary artery disease undergoing elective angioplasty K M Akkerhuis, MJBMvandenBrand, C van der Zwaan, HOJPeels, H Suryapranata, L R van der Wieken, J Stibbe, J HoVmann, T Baardman, J W Deckers, M L Simoons Abstract Objective—Lefradafiban is the orally active prodrug of fradafiban, a glycoprotein IIb/IIIa receptor antagonist. -

The Efficacy and Safety of Combination Glycoprotein Iibiiia Inhibitors And
Interventional Cardiology The efficacy and safety of combination glycoprotein IIbIIIa inhibitors and reduced-dose thrombolytic therapy–facilitated percutaneous coronary intervention for ST-elevation myocardial infarction: A meta-analysis of randomized clinical trials Mohamad C.N. Sinno, MD, Sanjaya Khanal, MD, FACC, Mouaz H. Al-Mallah, MD, Muhammad Arida, MD, and W. Douglas Weaver, MD Detroit, MI Objective We reviewed the literature and performed a meta-analysis comparing the safety and efficacy of adjunctive use of reduced-dose thrombolytics and glycoprotein (Gp) IIbIIIa inhibitors to the sole use of Gp IIbIIIa inhibitors before percutaneous coronary intervention (PCI) in patients presenting with acute ST-segment elevation myocardial infarction (STEMI). Background Early reperfusion in STEMI is associated with improved outcomes. The use of reduced-dose thrombolytic and Gp IIbIIIa inhibitors combination before PCI in the setting of acute STEMI remains controversial. Methods We performed a literature search and identified randomized trials comparing the use of combination therapy–facilitated PCI versus PCI done with Gp IIbIIIa inhibitor alone. Included studies were reviewed to determine Thrombolysis in Myocardial Infarction (TIMI)-3 flow at baseline, major bleeding, 30-day mortality, TIMI-3 flow after PCI,and 30-day reinfarction. We performed a random-effect model meta-analysis. We quantified heterogeneity between studies with I2. A value N50% represents substantial heterogeneity. Results We identified 4 clinical trials randomizing 725 patients; 424 patients were pretreated with combination therapy before PCI, and 301 patients had Gp IIbIIIa inhibitor alone during PCI. Combination therapy–facilitated PCI was associated with a 2-fold increase in TIMI-3 flow upon arrival to the catheterization laboratory compared with the sole use of upstream Gp IIbIIIa inhibitors (192/390 patients [49%] versus 60/284 [21%]; relative risk [RR], 2.2; P b .00001). -

Antiplatelet Therapy in Cardiovascular Disease M W H Behan, R F Storey
155 Postgrad Med J: first published as 10.1136/pgmj.2003.007062 on 11 March 2004. Downloaded from CARDIOLOGY UPDATE Antiplatelet therapy in cardiovascular disease M W H Behan, R F Storey ............................................................................................................................... Postgrad Med J 2004;80:155–164. doi: 10.1136/pgmj.2003.007062 Platelet activation and aggregation are considered to be and collagen covered by a layer of connective tissue. Also present in the core are cholesterol- central to arterial thrombus formation. Antiplatelet therapy containing macrophages (foam cells), derived is therefore important for both the treatment and prevention from monocytes that have crossed the endothe- of cardiovascular disease. Aspirin, the most widely used lium from the arterial lumen. These cells produce large amounts of prothrombotic tissue factor antiplatelet agent, inhibits platelet cyclo-oxygenase and the together with several inflammatory cell media- conversion of arachidonic acid to the potent platelet tors such as tumour necrosis factor-a and various agonist thromboxane A but does not prevent platelet interleukins.3910 2 The process of thrombosis starts when the activation occurring via various signalling pathways that atherosclerotic plaque tears and exposes the are independent of thromboxane A2 release. Therefore a lipid-rich core to blood in the arterial lumen. number of other compounds have been developed to Platelet adherence to the exposed subendothe- lium and collagen results in platelet activation complement aspirin’s beneficial effect. These include the and the release and local accumulation of soluble thienopyridines (clopidogrel and ticlopidine), platelet agonists (thrombin, adenosine dipho- dipyridamole, and the a b (glycoprotein IIb/IIIa) receptor sphate (ADP), serotonin, and thromboxane A2). IIb 3 This in turn causes further platelet aggregation, inhibitors. -
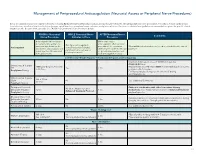
Neuraxial Access Or Peripheral Nerve Procedures)
Management of Periprocedural Anticoagulation (Neuraxial Access or Peripheral Nerve Procedures) Below are guidelines to prevent spinal hematoma following Epidural/Intrathecal/Spinal procedures and perineural hematoma following peripheral nerve procedures. Procedures include epidural injec- tions/infusions, intrathecal injections/infusions/pumps, spinal injections, peripheral nerve catheters, and plexus infusions. Decisions to deviate from guideline recommendations given the specific clinical situation are the decision of the provider. See ‘Additional Comments’ section for more details. PRIOR to Neuraxial/ WHILE Neuraxial/Nerve AFTER Neuraxial/Nerve Comments Nerve Procedure Catheter in Place Procedure How long should I hold prior When can I restart to neuraxial procedure? (i.e. anticoagulants after neuraxial Can I give anticoagulants minimum time between the procedures? (i.e. minimum What additional information do I need to consider for the care of Anticoagulant concurrently with neuraxial, last dose of anticoagulant and time between catheter removal patients? peripheral nerve catheter, or spinal injection OR neuraxial/ or spinal/nerve injection and plexus placement? nerve placement) next anticoagulation dose) Low-Molecular Weight Heparin, Unfractionated Heparin, and Fondaparinux Maximum total heparin dose of 10,000 units per day (5000 SQ Q12 hrs) Unfractionated Heparin 5000 units Q 12 hrs – no time Heparin 5000 units SQ 8 hrs is NOT recommended with concurrent SQ Yes 2 hrs restrictions neuraxial catheter in place Prophylaxis Dosing For IV prophylactic dosing, use ‘treatment’ IV dosing recommendations. Unfractionated Heparin SQ: 8-10 hrs SQ/IV No 2 hrs See ‘Additional Comments’ IV: 4 hrs Treatment Dosing Enoxaparin (Lovenox), Caution in combination with other hemostasis-altering No (Note: May be used for Dalteparin (Fragmin) 12 hrs 4 hrs medications.