Javier De Arteaga
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -

Anatomy and Physiology of Peritoneal Dialysis
Anatomy and Physiology of Peritoneal Dialysis Isaac Teitelbaum, MD Professor of Medicine Director, Acute & Home Dialysis Programs University of Colorado Hospital Denver, Colorado •1 Outline • Peritoneal cavity as a dialysis system • Models of peritoneal transport • Physiology of peritoneal transport Inverse relationship between solute transport and ultrafiltration • Kinetics of peritoneal transport • Synthesis & Application • Middle Molecules Anatomy of The Peritoneum • The lining of the abdominal cavity • Two layers: parietal - lines the anterior wall and undersurface of the diaphragm - 20% of total SA; blood supply from abdominal wall visceral - covers the abdominal organs - 80% of total SA; blood supply from mesenteric aa and portal vv Gokal R, Textbook of PD, pp. 61-70 •3 Anatomy of The Peritoneum • Size 1.5 – 2 m2; approximates BSA • Highly Vascular • Semi-permeable/bi-directional • “Lymphatic” drainage through diaphragmatic stomata • Continuous with Fallopian Tubes in females Gokal R, Textbook of PD, pp. 61-70 1. The two main properties of the peritoneal membrane are: a. Semi permeable – this allows substances of certain sizes to move from an area of greater concentration to less concentration. b. Bi Directional - substances move in either direction across the membrane. 2. So-called “lymphatic” drainage refers to bulk flow from the peritoneal cavity back to the circulation. This actually occurs across tissues as well as lymphatics. As this is convective flow, dissolved solutes move with the fluid. Thus, fluid reabsorption results in loss of solute clearance as well as loss of fluid removal. 3. It is important to be aware of the continuity of the peritoneal cavity with the Fallopian tubes as retrograde menstruation- which may occur in any woman but goes undetected- will cause bloody dialysate and create concern in the PD patient. -

Comparison of Clinical Effects Between
Kanno et al. Renal Replacement Therapy (2020) 6:7 https://doi.org/10.1186/s41100-019-0253-4 REVIEW Open Access Comparison of clinical effects between icodextrin and glucose solutions on outcomes of peritoneal dialysis: systematic review and meta-analysis of randomized controlled trials Atsuhiro Kanno1*, Yasushi Tsujimoto2, Takayuki Fujii3, Emi Fujikura4, Kimio Watanabe5, Hidemichi Yuasa6, Munekazu Ryuzaki7, Yasuhiko Ito8 and Hidetomo Nakamoto9 Abstract Background: Icodextrin enhances peritoneal filtration for patients on peritoneal dialysis (PD). However, clinically important outcomes have not yet been analyzed using authentic, objective statistical methods. The present systematic review aimed to determine the risks and benefits of icodextrin compared with a glucose-based solution with respect to clinically important and patient-centered outcomes. Methods: We systematically investigated only randomized controlled trials (RCTs) by adopting the Cochrane Database of Systematic Review (2014) and searched the CENTRAL, MEDLINE, and EMBASE databases for eligible studies reported in the literature. The quality of the evidence was assessed using the GRADE approach. Results: We finally evaluated important outcomes in 13 RCTs. Icodextrin significantly decreased the number of reported episodes of uncontrolled fluid overload in four RCTs that involved 236 patients (relative risk [RR], 0.31; 95% confidence interval [CI], 0.12 to 0.82; moderate certainty evidence). However, the inclusion of icodextrin for peritoneal ultrafiltration did not significantly differ in six RCTs involving 252 patients (mean difference [MD], 186.76 mL; 95% CI, − 47.08 to 420.59; low certainty evidence). Regarding other clinically important outcomes, all-cause mortality in 10 RCTs involving 1106 patients (RR, 0.75; 95% CI, 0.33 to 1.71; low certainty evidence) and technical survival in five RCTs involving 470 patients (RR, 0.57; 95%CI, 0.29 to 1.12; low certainty evidence) were not significant. -

Malta Medicines List April 08
Defined Daily Doses Pharmacological Dispensing Active Ingredients Trade Name Dosage strength Dosage form ATC Code Comments (WHO) Classification Class Glucobay 50 50mg Alpha Glucosidase Inhibitor - Blood Acarbose Tablet 300mg A10BF01 PoM Glucose Lowering Glucobay 100 100mg Medicine Rantudil® Forte 60mg Capsule hard Anti-inflammatory and Acemetacine 0.12g anti rheumatic, non M01AB11 PoM steroidal Rantudil® Retard 90mg Slow release capsule Carbonic Anhydrase Inhibitor - Acetazolamide Diamox 250mg Tablet 750mg S01EC01 PoM Antiglaucoma Preparation Parasympatho- Powder and solvent for solution for mimetic - Acetylcholine Chloride Miovisin® 10mg/ml Refer to PIL S01EB09 PoM eye irrigation Antiglaucoma Preparation Acetylcysteine 200mg/ml Concentrate for solution for Acetylcysteine 200mg/ml Refer to PIL Antidote PoM Injection injection V03AB23 Zovirax™ Suspension 200mg/5ml Oral suspension Aciclovir Medovir 200 200mg Tablet Virucid 200 Zovirax® 200mg Dispersible film-coated tablets 4g Antiviral J05AB01 PoM Zovirax® 800mg Aciclovir Medovir 800 800mg Tablet Aciclovir Virucid 800 Virucid 400 400mg Tablet Aciclovir Merck 250mg Powder for solution for inj Immunovir® Zovirax® Cream PoM PoM Numark Cold Sore Cream 5% w/w (5g/100g)Cream Refer to PIL Antiviral D06BB03 Vitasorb Cold Sore OTC Cream Medovir PoM Neotigason® 10mg Acitretin Capsule 35mg Retinoid - Antipsoriatic D05BB02 PoM Neotigason® 25mg Acrivastine Benadryl® Allergy Relief 8mg Capsule 24mg Antihistamine R06AX18 OTC Carbomix 81.3%w/w Granules for oral suspension Antidiarrhoeal and Activated Charcoal -

Fluid and Pharmacological Agents for Adhesion Prevention After Gynaecological Surgery (Review)
Fluid and pharmacological agents for adhesion prevention after gynaecological surgery (Review) Ahmad G, Mackie FL, Iles DA, O’Flynn H, Dias S, Metwally M, Watson A This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2014, Issue 7 http://www.thecochranelibrary.com Fluid and pharmacological agents for adhesion prevention after gynaecological surgery (Review) Copyright © 2014 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 SUMMARY OF FINDINGS FOR THE MAIN COMPARISON . ..... 4 BACKGROUND .................................... 6 OBJECTIVES ..................................... 7 METHODS ...................................... 7 RESULTS....................................... 9 Figure1. ..................................... 10 Figure2. ..................................... 12 Figure3. ..................................... 13 Figure4. ..................................... 14 Figure5. ..................................... 15 Figure6. ..................................... 16 Figure7. ..................................... 17 Figure8. ..................................... 18 Figure9. ..................................... 18 Figure10. ..................................... 19 ADDITIONALSUMMARYOFFINDINGS . 22 DISCUSSION ..................................... 32 AUTHORS’CONCLUSIONS . 33 ACKNOWLEDGEMENTS . 33 REFERENCES .................................... -

Country-Specific Glucose Monitor List
Country-Specific Glucose Monitor List Country Name: USA Important Information This is a non-comprehensive list, current as of March 2015. Absence of a specific glucose monitor or test strips from this list does NOT imply compatibility or incompatibility with EXTRANEAL (Icodextrin) PD solution. Similarly, other glucose-measuring technologies which are not listed below (such as continuous glucose monitoring systems) may or may not be compatible with EXTRANEAL. Always contact the device manufacturer for current information. If the manufacturer cannot provide information regarding compatibility of the device with icodextrin and maltose, Baxter does NOT recommend that Extraneal patients use the product. Baxter reserves the right to change this list without notice and does not represent that it includes all potentially incompatible products. The glucose monitors manufacturers listed have certified to Baxter that they have tested (as per 2013 ISO 15197) their monitors with maltose and icodextrin to Baxter’s recommended limits: 278 mg/dL (maltose) and 1094 mg/dL (icodextrin). The manufacturers certified that their “green” monitors, below, showed no interference of blood glucose readings under these conditions, with the exception of the “green” monitors specifically notated6 for which certification of testing to Baxter’s recommended limits has not yet been received. This list is compiled from a search via: Internet, literature, Baxter internal studies, information from government agencies, test strip leaflets, safety alerts, and direct information from the product manufacturers. While efforts have been made to provide accurate and current information, Baxter does not manufacture these glucose monitors or test strips and thus does not guarantee the initial or continued accuracy of this information. -

Queensland Health List of Approved Medicines
Queensland Health List of Approved Medicines Drug Form Strength Restriction abacavir * For use in accord with PBS Section 100 indications * oral liquid See above 20 mg/mL See above tablet See above 300 mg See above abacavir + lamivudine * For use in accord with PBS Section 100 indications * tablet See above 600 mg + 300 mg See above abacavir + lamivudine + * For use in accord with PBS Section 100 indications * zidovudine tablet See above 300 mg + 150 mg + 300 mg See above abatacept injection 250 mg * For use in accord with PBS Section 100 indications * abciximab (a) Interventional Cardiologists for complex angioplasty (b) Interventional and Neuro-interventional Radiologists for rescue treatment of thromboembolic events that occur during neuroendovascular procedures. * Where a medicine is not TGA approved, patients should be made fully aware of the status of the medicine and appropriate consent obtained * injection See above 10 mg/5 mL See above abiraterone For use by medical oncologists as per the PBS indications for outpatient and discharge use only tablet See above 250 mg See above 500 mg See above acamprosate Drug and alcohol treatment physicians for use with a comprehensive treatment program for alcohol dependence with the goal of maintaining abstinence. enteric tablet See above 333 mg See above acarbose For non-insulin dependent diabetics with inadequate control despite diet; exercise and maximal tolerated doses of other anti-diabetic agents tablet See above 50 mg See above 100 mg See above acetazolamide injection 500 mg tablet 250 mg acetic acid ear drops 3% 15mL solution 2% 100mL green 3% 1 litre 6% 1 Litre 6% 200mL Generated on: 30-Aug-2021 Page 1 of 142 Drug Form Strength Restriction acetylcysteine injection For management of paracetamol overdose 2 g/10 mL See above 6 g/30 mL See above aciclovir cream Infectious disease physicians, haematologists and oncologists 5% See above eye ointment For use on the advice of Ophthalmologists only. -
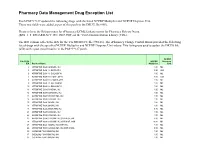
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

A Abacavir Abacavirum Abakaviiri Abagovomab Abagovomabum
A abacavir abacavirum abakaviiri abagovomab abagovomabum abagovomabi abamectin abamectinum abamektiini abametapir abametapirum abametapiiri abanoquil abanoquilum abanokiili abaperidone abaperidonum abaperidoni abarelix abarelixum abareliksi abatacept abataceptum abatasepti abciximab abciximabum absiksimabi abecarnil abecarnilum abekarniili abediterol abediterolum abediteroli abetimus abetimusum abetimuusi abexinostat abexinostatum abeksinostaatti abicipar pegol abiciparum pegolum abisipaaripegoli abiraterone abirateronum abirateroni abitesartan abitesartanum abitesartaani ablukast ablukastum ablukasti abrilumab abrilumabum abrilumabi abrineurin abrineurinum abrineuriini abunidazol abunidazolum abunidatsoli acadesine acadesinum akadesiini acamprosate acamprosatum akamprosaatti acarbose acarbosum akarboosi acebrochol acebrocholum asebrokoli aceburic acid acidum aceburicum asebuurihappo acebutolol acebutololum asebutololi acecainide acecainidum asekainidi acecarbromal acecarbromalum asekarbromaali aceclidine aceclidinum aseklidiini aceclofenac aceclofenacum aseklofenaakki acedapsone acedapsonum asedapsoni acediasulfone sodium acediasulfonum natricum asediasulfoninatrium acefluranol acefluranolum asefluranoli acefurtiamine acefurtiaminum asefurtiamiini acefylline clofibrol acefyllinum clofibrolum asefylliiniklofibroli acefylline piperazine acefyllinum piperazinum asefylliinipiperatsiini aceglatone aceglatonum aseglatoni aceglutamide aceglutamidum aseglutamidi acemannan acemannanum asemannaani acemetacin acemetacinum asemetasiini aceneuramic -

Delayed Allergic Cutaneous Hypersensitivity to Icodextrin by Nikesh Adunuri MD and Saira Zafar MD FRCPC
Case Report Delayed Allergic Cutaneous Hypersensitivity to Icodextrin By Nikesh Adunuri MD and Saira Zafar MD FRCPC About the Authors Nikesh Adunuri is with the Department of Internal Medicine at the University of Western Ontario. Saira Zafar is with the Department of Internal Medicine at the University of Western Ontario. Submitted: March 18, 2017. Accepted May 7, 2017. Published December 29, 2017. Abstract Rashes pose a unique challenge to general internists. Here we present a case of a 51-year-old female with end-stage renal disease (ESRD) on peritoneal dialysis who presented to a General Internal Medicine clinic with a vesiculobullous rash on palms and soles 6 months after using icodextrin dialysate, a widely used osmotic agent in peritoneal dialysis. The investigations were positive for an elevated eosinophil count, elevated IgE level and a skin biopsy consistent with an allergic reaction. Her symptoms and labs normalized after stopping icodextrin. There are some reports of allergic reactions to icodextrin which usually occur within a month of initiation of the agent and are self-limiting. Here we hope to report a case of a reaction that occurred 6 months after using icodextrin. Résumé Les éruptions cutanées posent un défi particulier aux internistes généraux. Nous rapportons ici le cas d’une femme de 51 ans atteinte d’insuffisance rénale terminale (IRT), sous dialyse péritonéale, qui se présente à une clinique de médecine interne générale avec une éruption cutanée vésiculo-bulleuse sur les paumes et la plante des pieds. Depuis six mois, la patiente utilise un dialysat d’icodextrine, un agent osmotique largement utilisé en dialyse péritonéale. -

Glucose Monitors Or Test Strips
Country Specific Glucose Monitor List Country Name: USA Important Information This list is compiled from a search via: Internet, literature, Baxter internal studies, information from government agencies, test strip leaflets, safety alerts, and direct information from the product manufacturers. While efforts have been made to provide accurate and current information, Baxter does not manufacture these glucose monitor or test strips and does not guarantee the initial or continued accuracy of this information. Please contact the manufacturer(s) of the glucose monitor and test strip to obtain the latest compatibility information before using in conjunction with EXTRANEAL (icodextrin) peritoneal dialysis (PD) solution. 1. EXTRANEAL (icodextrin) PD solution contains icodextrin. Maltose, a metabolite of icodextrin, may interfere with certain glucose monitors or test strips. This interference will result in a falsely elevated glucose reading using these monitors or test strips. 2. This interference may mask true hypoglycemia or lead to the erroneous diagnosis of hyperglycemia. Thus, a blood glucose reading within or above the normal range in a patient on EXTRANEAL (icodextrin) PD solution, using these monitors or test strips, may mask true low blood sugar. This would cause a patient or health care professional to not take the appropriate steps to bring the blood sugar into a normal range. Or, a falsely-elevated blood glucose reading could cause a patient to get more insulin than needed. Both of these situations can lead to life-threatening events, including loss of consciousness, coma, neurological damage or death. 3. The dialysis unit or patient should contact the manufacturer(s) of the glucose monitor and/or test strips to determine if the monitor or test strips they are using are subject to interference by icodextrin or maltose, or if they measure only glucose. -

EXTRANEAL (ICODEXTRIN 7.5%) Icodextrin
EXTRANEAL (ICODEXTRIN 7.5%) Icodextrin Consumer Medicine Information Blood glucose management with BEFORE THE USE OF • Use cardiac glycosides, such as Extraneal must be done with a EXTRANEAL digoxin. Your doctor may need to glucose-specific method to avoid FORMULA monitor your blood levels of interference resulting in calcium, potassium and unrecognised hypoglycemia. If magnesium. non-specific glucose test methods (GDH-PQQ) are used, loss of Do not use Extraneal if: Tell your doctor if you have had abdominal (stomach area): consciousness, neurological You have a known allergy to any of damage and death may occur. the ingredients listed at the end of • Surgery in the past 30 days this leaflet or to starch. • Tumors • You have a glycogen storage disease. Open wounds • Hernia WHAT IS IN THIS Additionally tell your doctor if you LEAFLET have recently had surgery on your Use during pregnancy or stomach or if you have any other breastfeeding Extraneal is not recommended if you This leaflet answers some more stomach complaints. common questions about are pregnant or breastfeeding. Your doctor should make sure that you are Extraneal. It does not contain all of Precautions: the available information. not pregnant before using Extraneal. Blood glucose measurement must be If you are of child bearing age, you All medicines have risks and done with a glucose-specific method must use a reliable method of birth benefits. Your doctor has weighed to prevent maltose interference with control while using Extraneal. the risks of you taking Extraneal test results. Since falsely elevated against the benefit they expect it will Use on the elderly glucose levels have been observed have for you.