Comparison of Disordered Swallowing Patterns in Patients with Recurrent Cortical/Subcortical Stroke and First-Time Brainstem Stroke
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Primary Lateral Sclerosis, Upper Motor Neuron Dominant Amyotrophic Lateral Sclerosis, and Hereditary Spastic Paraplegia
brain sciences Review Upper Motor Neuron Disorders: Primary Lateral Sclerosis, Upper Motor Neuron Dominant Amyotrophic Lateral Sclerosis, and Hereditary Spastic Paraplegia Timothy Fullam and Jeffrey Statland * Department of Neurology, University of Kansas Medical Center, Kansas, KS 66160, USA; [email protected] * Correspondence: [email protected] Abstract: Following the exclusion of potentially reversible causes, the differential for those patients presenting with a predominant upper motor neuron syndrome includes primary lateral sclerosis (PLS), hereditary spastic paraplegia (HSP), or upper motor neuron dominant ALS (UMNdALS). Differentiation of these disorders in the early phases of disease remains challenging. While no single clinical or diagnostic tests is specific, there are several developing biomarkers and neuroimaging technologies which may help distinguish PLS from HSP and UMNdALS. Recent consensus diagnostic criteria and use of evolving technologies will allow more precise delineation of PLS from other upper motor neuron disorders and aid in the targeting of potentially disease-modifying therapeutics. Keywords: primary lateral sclerosis; amyotrophic lateral sclerosis; hereditary spastic paraplegia Citation: Fullam, T.; Statland, J. Upper Motor Neuron Disorders: Primary Lateral Sclerosis, Upper 1. Introduction Motor Neuron Dominant Jean-Martin Charcot (1825–1893) and Wilhelm Erb (1840–1921) are credited with first Amyotrophic Lateral Sclerosis, and describing a distinct clinical syndrome of upper motor neuron (UMN) tract degeneration in Hereditary Spastic Paraplegia. Brain isolation with symptoms including spasticity, hyperreflexia, and mild weakness [1,2]. Many Sci. 2021, 11, 611. https:// of the earliest described cases included cases of hereditary spastic paraplegia, amyotrophic doi.org/10.3390/brainsci11050611 lateral sclerosis, and underrecognized structural, infectious, or inflammatory etiologies for upper motor neuron dysfunction which have since become routinely diagnosed with the Academic Editors: P. -

Pseudo Bulbar Palsy: a Rare Cause of Extubation Failure
Letters to the Editor 2. Deepak N A, Patel ND. Differential diagnosis of acute liver failure in Access this article online India. Ann Hepatol 2006;5:150‑6. Quick Response Code: 3. Singh V, Bhalla A, Sharma N, Mahi SK, Lal A, Singh P, et al. Website: Pathophysiology of jaundice in amoebic liver abscess. Am J Trop Med www.ijccm.org Hyg 2008;78:556‑9. 4. Kamarasu K, Malathi M, Rajagopal V, Subramani K, Jagadeeshramasamy D, Mathai E, et al. Serological evidence for wide DOI: distribution of spotted fevers & typhus fever in Tamil Nadu. Indian J 10.4103/ijccm.IJCCM_244_18 Med Res 2007;126:128‑30. 5. Poomalar GK, Rekha R. Scrub typhus in pregnancy. J Clin Diagn Res 2014;8:1‑3. How to cite this article: Mahto SK, Sheoran A, Goel A, Agarwal N. This is an open access journal, and articles are distributed under the terms of the Creative Uncommon cause of acute liver failure with encephalopathy. Indian J Crit Commons Attribution‑NonCommercial‑ShareAlike 4.0 License, which allows others to Care Med 2018;22:619‑20. remix, tweak, and build upon the work non‑commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms. © 2018 Indian Journal of Critical Care Medicine | Published by Wolters Kluwer ‑ Medknow Pseudo Bulbar Palsy: A Rare Cause of Extubation Failure Sir, Extubation Failure (EF) following weaning trials is a well known entity in Intensive Care Units (ICUs). The varied prevalence (2%–25%) of EF depends on the population studied and the time frame (24–72 h) included for analysis.[1] Airway edema and nonresolution of the primary disease are a common cause. -

Management of Neurogenic Dysphagia
694 Postgrad Med J 2001;77:694–699 Postgrad Med J: first published as 10.1136/pmj.77.913.694 on 1 November 2001. Downloaded from Management of neurogenic dysphagia A M O Bakheit Dysphagia is common in patients with neuro- of the cerebral cortex, basal ganglia, brain logical disorders. It may result from lesions in stem, cerebellum, and lower cranial nerves may the central or peripheral nervous system as well result in dysphagia. Degeneration of the as from diseases of muscle and disorders of the myenteric ganglion cells in the oesophagus, neuromuscular junction. Drugs that are com- muscle diseases and disorders of neuromusc- monly used in the management of neurological ular transmission, for example myasthenia conditions may also precipitate or aggravate gravis and Eaton-Lambers syndrome, are other swallowing diYculties in some patients. Neuro- less common causes. genic dysphagia often results in serious compli- cations, including pulmonary aspiration, dehy- CEREBRAL CORTEX dration, and malnutrition. These The commonest condition associated with complications are usually preventable if the dysphagia resulting from cortical lesions is stroke. Acute stroke is complicated by dys- dysphagia is recognised early and managed 1 appropriately. phagia in about 25%–42% of all cases. Dysphagia in these patients is usually associ- Physiological mechanisms of neurogenic ated with hemiplegia due to lesions of the brain stem or the involvement of one or both dysphagia The act of swallowing may be viewed as three hemispheres. However, on rare occasions, dys- discrete but inter-related physiological stages: phagia may be the sole manifestation of a cer- the oral, pharyngeal, and oesophageal phases. -

ICD9 & ICD10 Neuromuscular Codes
ICD-9-CM and ICD-10-CM NEUROMUSCULAR DIAGNOSIS CODES ICD-9-CM ICD-10-CM Focal Neuropathy Mononeuropathy G56.00 Carpal tunnel syndrome, unspecified Carpal tunnel syndrome 354.00 G56.00 upper limb Other lesions of median nerve, Other median nerve lesion 354.10 G56.10 unspecified upper limb Lesion of ulnar nerve, unspecified Lesion of ulnar nerve 354.20 G56.20 upper limb Lesion of radial nerve, unspecified Lesion of radial nerve 354.30 G56.30 upper limb Lesion of sciatic nerve, unspecified Sciatic nerve lesion (Piriformis syndrome) 355.00 G57.00 lower limb Meralgia paresthetica, unspecified Meralgia paresthetica 355.10 G57.10 lower limb Lesion of lateral popiteal nerve, Peroneal nerve (lesion of lateral popiteal nerve) 355.30 G57.30 unspecified lower limb Tarsal tunnel syndrome, unspecified Tarsal tunnel syndrome 355.50 G57.50 lower limb Plexus Brachial plexus lesion 353.00 Brachial plexus disorders G54.0 Brachial neuralgia (or radiculitis NOS) 723.40 Radiculopathy, cervical region M54.12 Radiculopathy, cervicothoracic region M54.13 Thoracic outlet syndrome (Thoracic root Thoracic root disorders, not elsewhere 353.00 G54.3 lesions, not elsewhere classified) classified Lumbosacral plexus lesion 353.10 Lumbosacral plexus disorders G54.1 Neuralgic amyotrophy 353.50 Neuralgic amyotrophy G54.5 Root Cervical radiculopathy (Intervertebral disc Cervical disc disorder with myelopathy, 722.71 M50.00 disorder with myelopathy, cervical region) unspecified cervical region Lumbosacral root lesions (Degeneration of Other intervertebral disc degeneration, -

Melioidosis: a Potentially Life Threatening Infection
CONTINUING MEDICAL EDUCATION Melioidosis: A Potentially Life Threatening Infection SH How, MMed*, CK Liam, FRCP*· *Department of Internal Medicine, Kulliyyah of Medicine, International Islamic University Malaysia, FO.Box 141, 27510, Kuantan, Pahang, Malaysia, **Department of Medicine, Faculty of Medicine, University of Malaya, 50603, Kuala Lumpur, MalaysIa Introduction example in Thailand, it is most commonly seen in the north-eastern region with an incidence of 4.4 per Melioidosis is caused by the gram-negative bacillus, 100,000 population per year'. In Northern Australia, Burkholderia pseudomallei, a common soil and fresh the incidence is higher (16.5 per 100,000 populations water saprophyte in tropical and subtropical regions. It 4 per yearY than that in Thailand • The incidence in is endemic in tropical Australial and in Southeast Asian Pahang and Singapore is 6.1 per 100, 000 population 23 4 countries, particularly Malaysia , Thailand and per year3 and 1.7 per 100,000 population per yearS, Singapores. However, only few doctors in these respectively. However, the true incidence may be endemic areas are fully aware of this infection. Hence, higher than that reported as most of these studies the management of this infection is often not included culture-confirmed cases only. Furthermore, appropriate and suboptimal. A recent study in Pahang some patients with mild infection from the rural areas has shown the incidence of this infection in Pahang3 is may not present to the hospital. More and more 4 comparable with that in northern Thailand • The melioidosis cases are being reported from previously overall mortality from this infection remains extremely unreported parts of the world especially southern high despite recent advancement in its treatment. -

History-Of-Movement-Disorders.Pdf
Comp. by: NJayamalathiProof0000876237 Date:20/11/08 Time:10:08:14 Stage:First Proof File Path://spiina1001z/Womat/Production/PRODENV/0000000001/0000011393/0000000016/ 0000876237.3D Proof by: QC by: ProjectAcronym:BS:FINGER Volume:02133 Handbook of Clinical Neurology, Vol. 95 (3rd series) History of Neurology S. Finger, F. Boller, K.L. Tyler, Editors # 2009 Elsevier B.V. All rights reserved Chapter 33 The history of movement disorders DOUGLAS J. LANSKA* Veterans Affairs Medical Center, Tomah, WI, USA, and University of Wisconsin School of Medicine and Public Health, Madison, WI, USA THE BASAL GANGLIA AND DISORDERS Eduard Hitzig (1838–1907) on the cerebral cortex of dogs OF MOVEMENT (Fritsch and Hitzig, 1870/1960), British physiologist Distinction between cortex, white matter, David Ferrier’s (1843–1928) stimulation and ablation and subcortical nuclei experiments on rabbits, cats, dogs and primates begun in 1873 (Ferrier, 1876), and Jackson’s careful clinical The distinction between cortex, white matter, and sub- and clinical-pathologic studies in people (late 1860s cortical nuclei was appreciated by Andreas Vesalius and early 1870s) that the role of the motor cortex was (1514–1564) and Francisco Piccolomini (1520–1604) in appreciated, so that by 1876 Jackson could consider the the 16th century (Vesalius, 1542; Piccolomini, 1630; “motor centers in Hitzig and Ferrier’s region ...higher Goetz et al., 2001a), and a century later British physician in degree of evolution that the corpus striatum” Thomas Willis (1621–1675) implicated the corpus -

Deep Brain Stimulation in the Treatment of Dyskinesia and Dystonia
Neurosurg Focus 17 (1):E2, 2004, Click here to return to Table of Contents Deep brain stimulation in the treatment of dyskinesia and dystonia HIROKI TODA, M.D., PH.D., CLEMENT HAMANI, M.D., PH.D., AND ANDRES LOZANO, M.D., PH.D., F.R.C.S.(C) Division of Neurosurgery, Department of Surgery, Toronto Western Hospital, University of Toronto, Ontario, Cananda Deep brain stimulation (DBS) has become a mainstay of treatment for patients with movement disorders. This modality is directed at modulating pathological activity within basal ganglia output structures by stimulating some of their nuclei, such as the subthalamic nucleus (STN) and the globus pallidus internus (GPi), without making permanent lesions. With the accumulation of experience, indications for the use of DBS have become clearer and the effective- ness and limitations of this form of therapy in different clinical conditions have been better appreciated. In this review the authors discuss the efficacy of DBS in the treatment of dystonia and levodopa-induced dyskinesias. The use of DBS of the STN and GPi is very effective for the treatment of movement disorders induced by levodopa. The relative ben- efits of using the GPi as opposed to the STN as a target are still being investigated. Bilateral GPi stimulation is gain- ing importance in the therapeutic armamentarium for the treatment of dystonia. The DYT1 forms of generalized dys- tonia and cervical dystonias respond to DBS better than secondary dystonia does. Discrimination between the diverse forms of dystonia and a better understanding of the pathophysiological features of this condition will serve as a plat- form for improved outcomes. -

THE SYNDROMES of the ARTERIES of the BRAIN and SPINAL CORD Part 1 by LESLIE G
65 Postgrad Med J: first published as 10.1136/pgmj.29.328.65 on 1 February 1953. Downloaded from THE SYNDROMES OF THE ARTERIES OF THE BRAIN AND SPINAL CORD Part 1 By LESLIE G. KILOH, M.D., M.R.C.P., D.P.M. First Assistant in the Joint Department of Psychological Medicine, Royal Victoria Infirmary and University of Durham Introduction general circulatory efficiency at the time of the Little interest is shown at present in the syn- catastrophe is of the greatest importance. An dromes of the arteries of the brain and spinal cord, occlusion, producing little effect in the presence of and this perhaps is related to the tendency to a normal blood pressure, may cause widespread minimize the importance of cerebral localization. pathological changes if hypotension co-exists. Yet these syndromes are far from being fully A marked discrepancy has been noted between elucidated and understood. It must be admitted the effects of ligation and of spontaneous throm- that in many cases precise localization is often of bosis of an artery. The former seldom produces little more than academic interest and ill effects whilst the latter frequently determines provides Protected by copyright. nothing but a measure of personal satisfaction to infarction. This is probably due to the tendency the physician. But it is worth recalling that the of a spontaneous thrombus to extend along the detailed study of the distribution of the bronchi affected vessel, sealing its branches and blocking and of the pathological anatomy of congenital its collateral circulation, and to the fact that the abnormalities of the heart, was similarly neglected arterial disease is so often generalized. -
Part Ii – Neurological Disorders
Part ii – Neurological Disorders CHAPTER 14 MOVEMENT DISORDERS AND MOTOR NEURONE DISEASE Dr William P. Howlett 2012 Kilimanjaro Christian Medical Centre, Moshi, Kilimanjaro, Tanzania BRIC 2012 University of Bergen PO Box 7800 NO-5020 Bergen Norway NEUROLOGY IN AFRICA William Howlett Illustrations: Ellinor Moldeklev Hoff, Department of Photos and Drawings, UiB Cover: Tor Vegard Tobiassen Layout: Christian Bakke, Division of Communication, University of Bergen E JØM RKE IL T M 2 Printed by Bodoni, Bergen, Norway 4 9 1 9 6 Trykksak Copyright © 2012 William Howlett NEUROLOGY IN AFRICA is freely available to download at Bergen Open Research Archive (https://bora.uib.no) www.uib.no/cih/en/resources/neurology-in-africa ISBN 978-82-7453-085-0 Notice/Disclaimer This publication is intended to give accurate information with regard to the subject matter covered. However medical knowledge is constantly changing and information may alter. It is the responsibility of the practitioner to determine the best treatment for the patient and readers are therefore obliged to check and verify information contained within the book. This recommendation is most important with regard to drugs used, their dose, route and duration of administration, indications and contraindications and side effects. The author and the publisher waive any and all liability for damages, injury or death to persons or property incurred, directly or indirectly by this publication. CONTENTS MOVEMENT DISORDERS AND MOTOR NEURONE DISEASE 329 PARKINSON’S DISEASE (PD) � � � � � � � � � � � -

Cranial Nerve Disorders 11/05/2012
Version 2.0 Cranial Nerve Disorders 11/05/2012 General Lesion possible locations: muscle, NMJ, nerve outside or inside brainstem Conditions that can affect any CN: DM, MS, Tumours, Sarcoid, Vasculitis (e.g. PAN), SLE, Syphilis, chronic meningitis (tends to pick off lower CN one by one). Olfactory (I) Nerve • Anatomy: Olfactory cells are a series of bipolar neurones which pass through the cribriform plate to the olfactory bulb. • Signs: Reduced taste and smell, but not to ammonia which stimulates the pain fibres carried in the trigeminal nerve. • Causes: Trauma; frontal lobe tumour; meningitis. Optic (II) Nerve • Anatomy: The optic nerve fibres are the axons of the retinal ganglion cells. Fibres from the nasal parts of retina decussate at optic chiasm, join with the non-decussating fibres and pass back in optic tracts to visual cortex. • Signs and causes: o Visual field defects: Field defects start as small areas of visual loss (scotomas). Monocular blindness: Lesions of one eye or optic nerve eg MS, giant cell arteritis. Bilateral blindness: Methyl alcohol, tobacco amblyopia; neurosyphilis. Bitemporal hemianopia: Optic chiasm compression eg internal carotid artery aneurysm, pituitary adenoma or craniopharyngioma Homonymous hemianopia: Affects half the visual field contralateral to the lesion in each eye. Lesions lie beyond the optic chiasm in the tracts, radiation or occipital cortex e.g. stroke, abscess, tumour. o Pupillary Abnormalities see pupillary abnormalities article. o Optic neuritis (pain on moving eye, loss of central vision, afferent pupillary defect, papilloedema). Causes: demyelination; rarely sinusitis, syphilis, collagen vascular disorders. o Optic atrophy (pale optic discs and reduced acuity): MS; frontal tumours; Friedreich's ataxia; retinitis pigmentosa; syphilis; glaucoma; Leber's optic atrophy; optic nerve compression. -
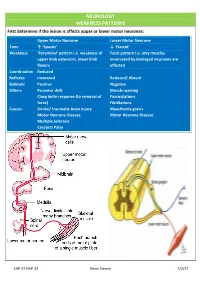
NEUROLOGY WEAKNESS PATTERNS First Determine If the Lesion Is Affects Upper Or Lower Motor Neurones
NEUROLOGY WEAKNESS PATTERNS First determine if the lesion is affects upper or lower motor neurones: Upper Motor Neurone Lower Motor Neurone Tone ↑ ‘Spastic’ ↓ ‘Flaccid’ Weakness ‘Pyramidal’ pattern i.e. weakness of Focal pattern i.e. only muscles upper limb extensors, lower limb innervated by damaged neurones are flexors affected Coordination Reduced Reflexes Increased Reduced/ Absent Babinski Positive Negative Others Pronator drift Muscle wasting Clasp knife response (to removal of Fasciculations force) Fibrillations Causes Stroke/ traumatic brain injury Myasthenia gravis Motor Neurone Disease Motor Neurone Disease Multiple Sclerosis Cerebral Palsy CAP 37 HAP 33 Kevin Gervin 7/2/17 What do we mean by extrapyramidal? Extrapyramidal symptoms Symptoms affecting tracts other than corticospinal and corticobulbar Extrapyramidal tracts don’t travel through the medullary pyramids The system regulates posture and muscle tone so pathology usually leads to movement disorders Most common cause is typical antipsychotics affecting Dopamine (D2) receptors e.g. haloperidol Treatment is anticholinergics e.g. procyclidine Extrapyramidal conditions: Acute dystonic reactions → muscle spasms e.g. neck, jaw, back. Akathisia- feeling of internal restlessness Drug induced Parkinsonism- tremor, rigidity etc. Tardive dyskinesia- involuntary muscle movements of lower face and extremities, often permanent What’s the difference between a Bulbar and Pseudobulbar palsy? Bulbar Pseudobulbar Pathophysiology LMN lesion CN V, VII, IX- XII Disease of corticobulbar -

Isolated Facial Palsy: a New Lacunar Syndrome
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.47.1.84 on 1 January 1984. Downloaded from Journal ofNeurology, Neurosuirgery, and Psychiatry 1984;47: 84-86 Short report Isolated facial palsy: a new lacunar syndrome CHENYA HUANG, GERALD BROE From the Department ofMedicine, University ofHong Kong, Queen Mary Hospital, Hong Kong and Department ofNeurology, Lidcombe Hospital, Lidcombe, Australia SUMMARY Three cases of sudden isolated upper motor neuron facial palsy and two with associated pseudobulbar palsy have been seen. All were without significant limb weakness. Computed tomography demonstrated small deep infarcts in the internal capsular/corona radiata regions. Pure upper motor neuron facial palsy may be another lacunar syndrome, due to a lesion in the internal capsule or corona radiata. palsies are lower motor neuron lesions. On examination blood pressure was 130/90 mm Hg. He Most facial facial paresis, complete an isolated facial palsy is seen had a left upper motor neuron Occasionally however, and aphagia. Jaw jerk was not increased. Tone, motor neuron in nature. anarthria which appears to be upper power, coordination and sensation were normal; however Protected by copyright. Prior to the availability of CT scan, the site of such the patient veered slightly to the left on walking. CSF lesion was unknown. Some have been ascribed to examination showed 1 mononuclear cell/mm' with normal peripheral facial nerve lesions. ' Puvenendren, Wong biochemistry and serology. EMG of facial muscles showed and Ransome described in 1979 five patients with no abnormality. CT scan showed small low density lesions sudden onset of dysarthria, dysphagia and upper bilaterally in the region of corona radiata adjacent to the motor neuron facial palsy.' EEG and isotope scans basal ganglia (fig 1).