Vibrio Vulnificus Hazard on the Half Shell KRISTI L
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABSTRACT DRAKE, STEPHENIE LYNN. the Ecology Vibrio
ABSTRACT DRAKE, STEPHENIE LYNN. The Ecology Vibrio vulnificus and Vibrio parahaemolyticus from Oyster Harvest Sites in the Gulf of Mexico. (Under the direction of Dr. Lee-Ann Jaykus). The Vibrionaceae are environmentally ubiquitous to estuarine waters. Two species in particular, V. vulnificus and V. parahaemolyticus, are important human pathogens that are transmitted by the consumption of contaminated molluscan shellfish. There is limited information available for the recent risk assessments; accordingly, the purpose of this study was to address some of these data gaps in the V. vulnificus and V. parahaemolyticus risk assessments. The objectives of this study were to (i) quantify the levels of total estuarine bacteria, total Vibrio spp., and specific levels of non-pathogenic and pathogenic V. vulnificus and V. parahaemolyticus over the harvest period; and (ii) determine if length of harvest time affects the levels of V. vulnificus. Oyster and water samples were harvested seasonally from 3 U.S. Gulf Coast sites over 2 years. Environmental parameters were monitored during harvesting. Both surface and bottom water samples (1 L) were taken at the beginning of harvesting and at the end of harvesting. Oyster samples (15 specimens for each time point) were taken at 0, 2.5, 5.0, 7.5, and 10 hrs intervals after being held at ambient temperature during harvesting. Samples were processed for many different bacteria. For enumeration of total V. parahaemolyticus, pathogenic V. parahaemolyticus, and V. vulnificus was done using colony lift hybridization (tlh, tdh+ and/or trh+, and vvhA gene targets, respectively). MPN methods were also used to obtain estimates of pathogenic V. -

Kellie ID Emergencies.Pptx
4/24/11 ID Alert! recognizing rapidly fatal infections Susan M. Kellie, MD, MPH Professor of Medicine Division of Infectious Diseases, UNMSOM Hospital Epidemiologist UNMHSC and NMVAHCS Fever and…. Rash and altered mental status Rash Muscle pain Lymphadenopathy Hypotension Shortness of breath Recent travel Abdominal pain and diarrhea Case 1. The cross-country trucker A 30 year-old trucker driving from Oklahoma to California is hospitalized in Deming with fever and headache He is treated with broad-spectrum antibiotics, but deteriorates with obtundation, low platelet count, and a centrifugal petechial rash and is transferred to UNMH 1 4/24/11 What is your diagnosis? What is the differential diagnosis of fever and headache with petechial rash? (in the US) Tickborne rickettsioses ◦ RMSF Bacteria ◦ Neisseria meningitidis Key diagnosis in this case: “doxycycline deficiency” Key vector-borne rickettsioses treated with doxycycline: RMSF-case-fatality 5-10% ◦ Fever, nausea, vomiting, myalgia, anorexia and headache ◦ Maculopapular rash progresses to petechial after 2-4 days of fever ◦ Occasionally without rash Human granulocytotropic anaplasmosis (HGA): case-fatality<1% Human monocytotropic ehrlichiosis (HME): case fatality 2-3% 2 4/24/11 Lab clues in rickettsioses The total white blood cell (WBC) count is typicallynormal in patients with RMSF, but increased numbers of immature bands are generally observed. Thrombocytopenia, mild elevations in hepatic transaminases, and hyponatremia might be observed with RMSF whereas leukopenia -

Vol. XXV Issue No. 2 June 2004
Vol. XXV Issue No. 2 June 2004 Report on the Enhanced Surveillance for Chlamydia West Nile Virus - 2003 Summary and in Women - South Carolina, 1998-2002 the Upcoming Season WAYNE A. DUFFUS, MD, PhD LENA M. BRETOUS, MD, MPH Medical Consultant Medical Consultant Extent of Chlamydia Problem Chlamydia remains a significant health threat among In 2003, South Carolina recorded six human cases of women and adolescents. Most estimates predict that 1 in 20 West Nile Virus (WNV). Surveillance numbers for other WNV sexually active woman of childbearing age or 1 in 10 adoles- positives in 2003 include: 282 birds, 54 equine, 3 mosquito cent girls are infected with chlamydia. In fact, 90% of all pools, and 1 alpaca. See table on page reported cases are in individuals less than 24 years of age. three for human case description. INSIDE THIS ISSUE Unfortunately, 60 – 80% of infected women have no symp- Because of the long stretch of toms, and therefore are not aware of their infection and may warm weather in spring and fall, in- Report on the Enhanced not seek health care. fected mosquitoes have a longer win- Surveillance for Chlamydia is the most commonly reported sexually dow to spread the disease in South Chlamydia in Women - South Carolina, transmitted infection among women in the United States (US). Carolina. The first human WNV case 1998 - 2002 The southeast led the nation in chlamydia prevalence in 2002. in South Carolina during 2003 was also Pg. 1 For example, there were 451.1 cases/100,000 persons diag- the first recorded case in the country nosed in the U.S. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Vibrio Vulnificus Fact Sheet
DISTRICT OF COLUMBIA DEPARTMENT OF HEALTH Division of Epidemiology, Disease Surveillance and Investigation 899 N. Capitol Street, NE, Suite 580 Washington, D.C. 20002 (202) 442-9371 * Fax (202) 442-8060 www.dchealth.dc.gov What is the treatment for Vibrio vulnificus What is Vibrio vulnificus? infection? Vibrio vulnificus is a bacterium in the same family that Vibrio vulnificus infection is treated with antibiotics, causes cholera. The bacterium lives in warm seawater such as tetracycline, doxycycline, or cephalosporin and is a salt-requiring organism. It is frequently isolated (e.g., ceftazidime). from oysters and other shellfish in warm coastal waters during the summer months. How can Vibrio vulnificus infection be prevented? What is Vibrio vulnificus infection? • Do not eat raw oysters or other raw Vibrio vulnificus infection is an acute illness that shellfish. produces septicemia (blood infection) in persons with • Cook shellfish (oysters, clams, mussels) chronic liver disease, chronic alcoholism, or those who thoroughly. Boil until the shells open and are immunocompromised. When open wounds are continue boiling for 5 minutes, or steam exposed to warm seawater, Vibrio vulnificus infections until the shells open during cooking. Do not may lead to skin breakdown and ulceration. Bloodstream eat shellfish that do not open during infections, common in immunocompromised persons, cooking. Boil shucked oysters for at least 3 can be fatal. The majority of infections in the United minutes, or fry them in oil at least 10 States are reported from the Gulf Coast states. minutes at 375°F. • Avoid cross-contamination of cooked How does Vibrio vulnificus infection occur? seafood and other foods with raw seafood Infection occurs after eating contaminated raw or and their juices. -

CHAPTER E16 Atlas of Skin Manifestations of Internal Disease CHAPTER E16 Thomas J
CHAPTER e16 Atlas of Skin Manifestations of Internal Disease CHAPTER e16 Thomas J. Lawley Robert A. Swerlick In the practice of medicine, virtually every clinician encounters patients with skin disease. Physicians of all specialties face the daily task of determining the nature and clinical implication of dermatologic disease. In patients with skin eruptions and rashes, the physician must confront the question of whether the cutaneous Atlas of Skin Manifestations Internal Disease process is confined to the skin, representing a pure dermatologic event, or whether it is a manifestation of internal disease relating to the patient’s overall medical condition. Evaluation and accurate diagnosis of skin lesions are also critical given the marked rise in both melanoma and nonmelanoma skin cancer. Dermatologic conditions can be classified and categorized in many different ways, Figure e16-2 Acne rosacea with prominent facial erythema, telangiecta- and in this Atlas, a selected group of inflammatory skin eruptions sias, scattered papules, and small pustules. (Courtesy of Robert Swerlick, and neoplastic conditions are grouped in the following manner: MD; with permission.) (A) common skin diseases and lesions, (B) nonmelanoma skin cancer, (C) melanoma and pigmented lesions, (D) infectious dis- ease and the skin, (E) immunologically mediated skin disease, and (F) skin manifestations of internal disease. COMMON SKIN DISEASES AND LESIONS ( Figs. e16-1 to e16-19) In this section, several common inflamma- tory skin diseases and benign neoplastic and reactive lesions are presented. While most of these dermatoses usually present as a pre- dominantly dermatologic process, underlying systemic associations may be made in some settings. Atopic dermatitis is often present in patients with an atopic diathesis, including asthma and sinusitis. -
Ecthyma Gangrenosum of a Single Limb
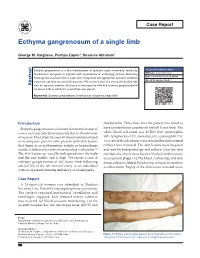
Case Report Ecthyma gangrenosum of a single limb George M. Varghese, Pushpa Eapen1, Susanne Abraham1 Ecthyma gangrenosum is a skin manifestation of systemic sepsis commonly caused by Access this article online Pseudomonas aeruginosa in patients with neutropenia or underlying immune deficiency. Website: www.ijccm.org Although the usual outcome is poor, early recognition and appropriate systemic antibiotic DOI: 10.4103/0972-5229.84898 treatment can lead to successful outcome. We report a case of a previously healthy lady Quick Response Code: Abstract with no apparent immune deficiency or neutropenia who had ecthyma gangrenosum of left lower limb in which the arterial line was placed. Keywords: Ecthyma gangrenosum, Pseudomonas aeruginosa, single limb Introduction thachycardia. Three days later the patient was noted to Ecthyma gangrenosum is a known skin manifestation of have erythematous papules on the left lower limb. The 3 severe systemic infection commonly due to Pseudomonas white blood cell count was 16,500/mm (neutrophils aeruginosa. Most often it is seen in immunocompromised 84%, lymphocytes 12%, monocytes 3%, eosinophils 1%). or neutropenic patients who present with skin lesions Two sets of blood cultures were sent and the intra-arterial that begin as an erythematous nodule or hemorrhagic catheter was removed. The skin lesions were biopsied vesicle, which evolves into a necrotic ulcer with eschar. [1] and sent for histopathology and culture. Over the next The skin lesions are usually widespread over the body few days the skin lesions became blackish with necrotic and the case fatality rate is high. We report a case of areas (arrow) [Figure 1]. The blood, catheter tip, and skin ecthyma gangrenosum of left lower limb following lesion cultures yielded Pseudomonas aeruginosa sensitive arterial line in the left femoral artery in an individual to ceftazidime. -

Investigation Into Rising Vibrio Populations in Eastern Coast Oysters Eric Grigg, Donna L
Investigation into Rising Vibrio Populations in Eastern Coast Oysters Eric Grigg, Donna L. Rhoads, M.Sc. Introduction Results and Discussion Conclusion Vibrio parahaemolyticus is a gram-negative, rod-shaped, and halophilic bacteria that is the leading cause of Oyster Collection: The study found an increasing trend of both Vibrio parahaemolyticus CFUs and Vibrio vulnificus CFUs. This seafood-borne bacterial gastroenteritis. The gastroenteritis is caused when Vibrio parahaemolyticus is consumed with shows that the risk of infection with Vibrio bacteria via raw oysters rises during the summer months. In addition, raw oysters and various other forms of seafood. The gastroenteritis is mainly characterized by watery diarrhea along Our results show an overall increase in Vibrio CFUs over the course of the summer. Our first four collections show a constant heavy rainfall seems to have an effect on Vibrio populations. After Hurricane Arthur passed, the CFUs for Vibrio with nausea, vomiting, abdominal cramps, chills, and fever.1 Vibrio vulnificus causes the same gastroenteritis, but can increase in number of Vv CFUs until our fifth collection. The fifth collection was performed after Hurricane Arthur passed through the vulnificus dropped sharply. This occurred again after heavy rainfall during the eighth week of the study. Given these infect the bloodstream of immunocompromised people causing fever, chills, lowered blood pressure, and skin lesions.2 Connecticut area around the 4th of July. The hurricane contributed to the drop in Vv numbers by decreasing the salinity of the water results, routine surveillance of oyster beds should be instituted. In addition, a more thorough means of cleaning the Fifty percent of people infected with Vibrio vulnificus succumb to the infection.2 and increasing the amount of sediment and runoff from the mainland. -

Skin and Soft Tissue Infections Following Marine Injuries
CHAPTER 6 Skin and Soft Tissue Infections Following Marine Injuries V. Savini, R. Marrollo, R. Nigro, C. Fusella, P. Fazii Spirito Santo Hospital, Pescara, Italy 1. INTRODUCTION Bacterial diseases following aquatic injuries occur frequently worldwide and usually develop on the extremities of fishermen and vacationers, who are exposed to freshwater and saltwater.1,2 Though plenty of bacterial species have been isolated from marine lesions, superficial soft tissue and invasive systemic infections after aquatic injuries and exposures are related to a restricted number of microorganisms including, in alphabetical order, Aeromonas hydrophila, Chromobacterium violaceum, Edwardsiella tarda, Erysipelothrix rhusiopathiae, Myco- bacterium fortuitum, Mycobacterium marinum, Shewanella species, Streptococcus iniae, and Vibrio vulnificus.1,2 In particular, skin disorders represent the third most common cause of morbidity in returning travelers and are usually represented by bacterial infections.3–12 Bacterial skin and soft tissue infectious conditions in travelers often follow insect bites and can show a wide range of clinical pictures including impetigo, ecthyma, erysipelas, abscesses, necro- tizing cellulitis, myonecrosis.3–12 In general, even minor abrasions and lacerations sustained in marine waters should be considered potentially contaminated with marine bacteria.3–12 Despite variability of the causative agents and outcomes, the initial presentations of skin and soft tissue infections (SSTIs) complicating marine injuries are similar to those occurring after terrestrial exposures and usually include erysipelas, impetigo, cellulitis, and necrotizing infections.3 Erysipelas is characterized by fiery red, tender, painful plaques showing well-demarcated edges, and, though Streptococcus pyogenes is the major agent of this pro- cess, E. rhusiopathiae infections typically cause erysipeloid displays.3 Impetigo is initially characterized by bullous lesions and is usually due to Staphylococcus aureus or S. -

Kentucky Reportable Disease Form Department for Public Health Division of Epidemiology and Health Planning 275 East Main St., Mailstop HS1E-C
EPID 200 (Rev. Jan/03) Kentucky Reportable Disease Form Department for Public Health Division of Epidemiology and Health Planning 275 East Main St., Mailstop HS1E-C Frankfort, KY 40621-0001 Disease Name_____________________ Mail Form to Local Health Department DEMOGRAPHIC DATA Patient’s Last Name First M.I. Date of Birth Age Gender / / M F Unk Address City State Zip County of Residence Phone Number Patient ID Number Ethnic Origin Race His. Non-His. W B A/PI Am.Ind. Other DISEASE INFORMATION Disease/Organism Date of Onset Date of Diagnosis / / / / List Symptoms/Comments Highest Temperature Days of Diarrhea Hospitalized? Admission Date Discharge Date Died? Date of Death Yes No / / / / Yes No Unk / / Hospital Name: Is Patient Pregnant? Yes No If yes, # wks_____ School/Daycare Associated? Yes No Outbreak Associated? Yes No Name of School/Daycare: Food Handler? Yes No Person or Agency Completing form: Attending Physician: Name: Agency: Name: Address: Address: Phone: Date of Report: / / Phone: LABORATORY INFORMATION Date Name or Type of Test Name of Laboratory Specimen Source Results ADDITIONAL INFORMATION FOR SEXUALLY TRANSMITTED DISEASES ONLY Method of case detection: Prenatal Community & Screening Delivery Instit. Screening Reactor Provider Report Volunteer Disease: Stage Disease: Site: (Check all that apply) Resistance: Primary (lesion) Secondary (symptoms) Gonorrhea Genital, uncomplicated Ophthalmic Penicillin Syphilis Early Latent Late Latent Chlamydia Pharyngeal PID/Acute Tetracycline Congenital Other Chancroid Anorectal Salpingitis Other ___________ Other___________________ Date of spec. Laboratory Name Type of Test Results Treatment Date Medication Dose Collection If syphilis, was previous treatment given for this infection? Yes No If yes, give approximate date and place_______________________________________________________________ 902 KAR 2:020 requires health professionals to report the following diseases to the local health departments serving the jurisdiction in which the patient resides or to the Kentucky Department for Public Health (KDPH). -

Cutaneous Manifestations of Infection in the Immunocompromised Host
Cutaneous Manifestations of Infection in the Immunocompromised Host Marc E. Grossman • Lindy P. Fox • Carrie Kovarik Misha Rosenbach Cutaneous Manifestations of Infection in the Immunocompromised Host Second Edition Authors Marc E. Grossman, M.D. Carrie Kovarik, M.D. Professor of Clinical Dermatology Assistant Professor of Dermatology College of Physicians and Surgeons Dermatopathology, and Infectious Diseases Director, Hospital Consultation Service University of Pennsylvania New York Presbyterian Hospital Philadelphia, Pennsylvania, USA Columbia University Medical Center New York, New York, USA Misha Rosenbach, M.D. Assistant Professor of Dermatology Lindy P. Fox, M.D. and Internal Medicine Associate Professor of Clinical Dermatology Director, Dermatology Inpatient Consult Service Director, Hospital Consultation Service University of Pennsylvania University of California, San Francisco Philadelphia, Pennsylvania, USA San Francisco, California, USA ISBN 978-1-4419-1577-1 e-ISBN 978-1-4419-1578-8 DOI 10.1007/978-1-4419-1578-8 Springer New York Dordrecht Heidelberg London Library of Congress Control Number: 2011933837 Springer Science+Business Media, LLC 2012 All rights reserved. Th is work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter devel- oped is forbidden. Th e use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identifi ed as such, is not to be taken as an expression of opinion as to whether or not they are subject to proprietary rights. -

Calhoun County Reportable Disease
Page 1 of 5 FLORIDA DEPARTMENT OF HEALTH Date: 10/13/2014 MERLIN Registry System Time: 04:14:54 pm CONFIRMED, PROBABLE, SUSPECT, UNKNOWN CASES OF MULTIPLE DISEASES WITH REPORT DATE FROM 12/29/2013 TO Period Comparison Selection Date Compare Date 1 Compare Date 2 Compare Date 3 12/29/2013 - 10/13/2014 12/29/2012 - 10/13/2013 12/29/2011 - 10/13/2012 12/29/2010 - 10/13/2011 Disease Name Cases Rates* Cases Rates* Cases Rates* Cases Rates* County: CALHOUN Brucellosis - 02300 0 0.00 0 0.00 1 6.81 0 0.00 Campylobacteriosis - 03840 0 0.00 0 0.00 3 20.44 0 0.00 Cryptosporidiosis - 13680 1 6.82 0 0.00 0 0.00 0 0.00 Giardiasis, Acute - 00710 0 0.00 0 0.00 1 6.81 0 0.00 Haemophilus influenzae Invasive Disease - 0 0.00 1 6.77 0 0.00 0 0.00 03841 Hepatitis B, Chronic - 07032 1 6.82 0 0.00 2 13.63 0 0.00 Hepatitis C, Chronic - 07054 22 149.95 11 74.44 11 74.95 15 102.46 Lead Poisoning - 94890 0 0.00 1 6.77 0 0.00 1 6.83 Meningococcal Disease - 03630 0 0.00 0 0.00 0 0.00 1 6.83 Rabies, Animal - 07102 0 0.00 0 0.00 0 0.00 1 6.83 Rabies, Possible Exposure - 07101 1 6.82 0 0.00 4 27.26 2 13.66 Salmonellosis - 00300 1 6.82 3 20.30 4 27.26 3 20.49 Varicella (Chickenpox) - 05290 0 0.00 0 0.00 0 0.00 2 13.66 Vibriosis (Vibrio parahaemolyticus) - 00540 0 0.00 1 6.77 0 0.00 0 0.00 Total: 26 177.23 17 115.05 26 177.16 25 170.77 STATEWIDE TOTAL Amebic Encephalitis - 13620 1 0.01 1 0.01 0 0.00 1 0.01 Anthrax - 02200 0 0.00 0 0.00 0 0.00 1 0.01 Arboviral Disease, Other - 06000 1 0.01 0 0.00 0 0.00 0 0.00 Arsenic Poisoning - 98080 2 0.01 12 0.06 6 0.03 4 0.02 Botulism,