Prior Authorization Criteria June 2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
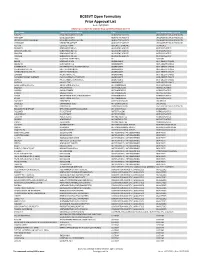
BCBSVT Open Formulary Prior Approval List
BCBSVT Open Formulary Prior Approval List As of: 10/27/2020 Helpful Tip: To search for a specific drug, use the find feature (Ctrl + F) Trade Name Chemical/Biological Name Class Prior Authorization Program FUSILEV LEVOLEUCOVORIN CALCIUM ADJUNCTIVE AGENTS UNCLASSIFIED DRUG PRODUCTS KHAPZORY LEVOLEUCOVORIN ADJUNCTIVE AGENTS UNCLASSIFIED DRUG PRODUCTS LEVOLEUCOVORIN CALCIUM LEVOLEUCOVORIN CALCIUM ADJUNCTIVE AGENTS UNCLASSIFIED DRUG PRODUCTS VISTOGARD URIDINE TRIACETATE ADJUNCTIVE AGENTS UNCLASSIFIED DRUG PRODUCTS ACTHAR CORTICOTROPIN ADRENAL HORMONES HORMONES BELRAPZO BENDAMUSTINE HCL ALKYLATING AGENTS ANTINEOPLASTICS BENDAMUSTINE HCL BENDAMUSTINE HCL ALKYLATING AGENTS ANTINEOPLASTICS BENDEKA BENDAMUSTINE HCL ALKYLATING AGENTS ANTINEOPLASTICS TREANDA BENDAMUSTINE HCL ALKYLATING AGENTS ANTINEOPLASTICS DAW (DISPENSE AS WRITTEN) ALL CUSTOM BELVIQ LORCASERIN HCL ANOREXIANTS ANTI‐OBESITY DRUGS BELVIQ XR LORCASERIN HCL ANOREXIANTS ANTI‐OBESITY DRUGS CONTRAVE ER NALTREXONE HCL/BUPROPION HCL ANOREXIANTS ANTI‐OBESITY DRUGS DIETHYLPROPION HCL DIETHYLPROPION HCL ANOREXIANTS ANTI‐OBESITY DRUGS DIETHYLPROPION HCL ER DIETHYLPROPION HCL ANOREXIANTS ANTI‐OBESITY DRUGS LOMAIRA PHENTERMINE HCL ANOREXIANTS ANTI‐OBESITY DRUGS PHENDIMETRAZINE TARTRATE PHENDIMETRAZINE TARTRATE ANOREXIANTS ANTI‐OBESITY DRUGS QSYMIA PHENTERMINE/TOPIRAMATE ANOREXIANTS ANTI‐OBESITY DRUGS SAXENDA LIRAGLUTIDE ANOREXIANTS ANTI‐OBESITY DRUGS ABIRATERONE ACETATE ABIRATERONE ACETATE ANTIANDROGENS ANTINEOPLASTICS ERLEADA APALUTAMIDE ANTIANDROGENS ANTINEOPLASTICS NUBEQA DAROLUTAMIDE ANTIANDROGENS -

DRUGS REQUIRING PRIOR AUTHORIZATION in the MEDICAL BENEFIT Page 1
Effective Date: 08/01/2021 DRUGS REQUIRING PRIOR AUTHORIZATION IN THE MEDICAL BENEFIT Page 1 Therapeutic Category Drug Class Trade Name Generic Name HCPCS Procedure Code HCPCS Procedure Code Description Anti-infectives Antiretrovirals, HIV CABENUVA cabotegravir-rilpivirine C9077 Injection, cabotegravir and rilpivirine, 2mg/3mg Antithrombotic Agents von Willebrand Factor-Directed Antibody CABLIVI caplacizumab-yhdp C9047 Injection, caplacizumab-yhdp, 1 mg Cardiology Antilipemic EVKEEZA evinacumab-dgnb C9079 Injection, evinacumab-dgnb, 5 mg Cardiology Hemostatic Agent BERINERT c1 esterase J0597 Injection, C1 esterase inhibitor (human), Berinert, 10 units Cardiology Hemostatic Agent CINRYZE c1 esterase J0598 Injection, C1 esterase inhibitor (human), Cinryze, 10 units Cardiology Hemostatic Agent FIRAZYR icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent HAEGARDA c1 esterase J0599 Injection, C1 esterase inhibitor (human), (Haegarda), 10 units Cardiology Hemostatic Agent ICATIBANT (generic) icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent KALBITOR ecallantide J1290 Injection, ecallantide, 1 mg Cardiology Hemostatic Agent RUCONEST c1 esterase J0596 Injection, C1 esterase inhibitor (recombinant), Ruconest, 10 units Injection, lanadelumab-flyo, 1 mg (code may be used for Medicare when drug administered under Cardiology Hemostatic Agent TAKHZYRO lanadelumab-flyo J0593 direct supervision of a physician, not for use when drug is self-administered) Cardiology Pulmonary Arterial Hypertension EPOPROSTENOL (generic) -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Pharmacological Management of Acromegaly: a Current Perspective
Neurosurg Focus 29 (4):E14, 2010 Pharmacological management of acromegaly: a current perspective SUNIL MANJILA , M.D.,1 Osmo N D C. WU, B.A.,1 FAH D R. KHAN , M.D., M.S.E.,1 ME H ree N M. KHAN , M.D.,2 BAHA M. AR A F AH , M.D.,2 AN D WA rre N R. SE L M AN , M.D.1 1Department of Neurological Surgery, The Neurological Institute, and 2Division of Clinical and Molecular Endocrinology, University Hospitals Case Medical Center, Cleveland, Ohio Acromegaly is a chronic disorder of enhanced growth hormone (GH) secretion and elevated insulin-like growth factor–I (IGF-I) levels, the most frequent cause of which is a pituitary adenoma. Persistently elevated GH and IGF-I levels lead to substantial morbidity and mortality. Treatment goals include complete removal of the tumor causing the disease, symptomatic relief, reduction of multisystem complications, and control of local mass effect. While trans- sphenoidal tumor resection is considered first-line treatment of patients in whom a surgical cure can be expected, pharmacological therapy is playing an increased role in the armamentarium against acromegaly in patients unsuitable for or refusing surgery, after failure of surgical treatment (inadequate resection, cavernous sinus invasion, or transcap- sular intraarachnoid invasion), or in select cases as primary treatment. Three broad drug classes are available for the treatment of acromegaly: somatostatin analogs, dopamine agonists, and GH receptor antagonists. Somatostatin analogs are considered as the first-line pharmacological treatment of acromegaly, although effica- cy varies among the different formulations. Octreotide long-acting release (LAR) appears to be more efficacious than lanreotide sustained release (SR). -
Cross Discipline Team Leader Review
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 203255Orig1s000 CROSS DISCIPLINE TEAM LEADER REVIEW Cross Discipline Team Leader Review pituitary adenoma (pituitary acromegaly) and only very rarely to an ectopic source of GH. Therefore for practical purposes, acromegaly is a pituitary disease. Although the treatment of choice of pituitary acromegaly is surgical removal of the pituitary mass via transsfenoidal route, the success rate is variable (90% in patients with microadenoma and below 50% in patients with macroadenomas). Patients who fail surgery (or cannot undergo surgery for a variety of reasons) benefit from radiation or pharmacological therapy. Because the effects of radiation may take years to reach effectiveness, medical therapy is almost invariably used in patients who respond poorly or incompletely to surgical management. Tight GH control and a normalization of serum IGF-1 are the goals of medical treatment. GH reductions to ≤1 μg/L using a modern sensitive immunoassay (approximately equivalent to 2.5 μg/L measured by RAI)2 following an oral glucose load are desirable. There are three drug products that have been approved by the FDA for the medical treatment of acromegaly. From a mechanism of action perspective they belong to two distinct classes: somatostatin analogs (octreotide and lanreotide) and GH receptor antagonists (pegvisomant). Pegvisomant (SOMAVERT) is a pegylated GH analog and acts as a GH receptor antagonist. It competes with endogenous GH for GH receptor binding. Once bound to the GH receptor it prevents receptor dimerization and subsequent intracellular signaling, thus blocking generation of IGF-1. The major safety signal identified with pegvisomant is transient liver enzyme elevation; however, no drug-induced liver failure has been documented to date. -

Oregon Medicaid Pharmaceutical Services Prior Authorization Criteria
Oregon Medicaid Pharmaceutical Services Prior Authorization Criteria HEALTH SYSTEMS DIVISION Prior authorization (PA) criteria for fee-for-service prescriptions for Oregon Health Plan clients March 1, 2021 Contents Contents ................................................................................................................................................................ 2 Introduction........................................................................................................................................................... 7 About this guide ......................................................................................................................................... 7 How to use this guide ................................................................................................................................. 7 Administrative rules and supplemental information .................................................................................. 7 Update information............................................................................................................................................... 8 Effective March 1, 2021 ............................................................................................................................ 8 Substantive updates and new criteria ............................................................................................. 8 Clerical changes ............................................................................................................................ -

To Download a List of Prescription Drugs Requiring Prior Authorization
Essential Health Benefits Standard Specialty PA and QL List July 2016 The following products require prior authorization. In addition, there may be quantity limits for these drugs, which is notated below. Therapeutic Category Drug Name Quantity Limit Anti-infectives Antiretrovirals, HIV SELZENTRY (maraviroc) None Cardiology Antilipemic JUXTAPID (lomitapide) 1 tab/day PRALUENT (alirocumab) 2 syringes/28 days REPATHA (evolocumab) 3 syringes/28 days Pulmonary Arterial Hypertension ADCIRCA (tadalafil) 2 tabs/day ADEMPAS (riociguat) 3 tabs/day FLOLAN (epoprostenol) None LETAIRIS (ambrisentan) 1 tab/day OPSUMIT (macitentan) 1 tab/day ORENITRAM (treprostinil diolamine) None REMODULIN (treprostinil) None REVATIO (sildenafil) Soln None REVATIO (sildenafil) Tabs 3 tabs/day TRACLEER (bosentan) 2 tabs/day TYVASO (treprostinil) 1 ampule/day UPTRAVI (selexipag) 2 tabs/day UPTRAVI (selexipag) Pack 2 packs/year VELETRI (epoprostenol) None VENTAVIS (iloprost) 9 ampules/day Central Nervous System Anticonvulsants SABRIL (vigabatrin) pack None Depressant XYREM (sodium oxybate) 3 bottles (540 mL)/30 days Neurotoxins BOTOX (onabotulinumtoxinA) None DYSPORT (abobotulinumtoxinA) None MYOBLOC (rimabotulinumtoxinB) None XEOMIN (incobotulinumtoxinA) None Parkinson's APOKYN (apomorphine) 20 cartridges/30 days Sleep Disorder HETLIOZ (tasimelteon) 1 cap/day Dermatology Alkylating Agents VALCHLOR (mechlorethamine) Gel None Electrolyte & Renal Agents Diuretics KEVEYIS (dichlorphenamide) 4 tabs/day Endocrinology & Metabolism Gonadotropins ELIGARD (leuprolide) 22.5 mg -

Medicines Not Reimbursed Through National Prices and Directly Commissioned by Nhs England V14 Changes to Version 13
MEDICINES NOT REIMBURSED THROUGH NATIONAL PRICES AND DIRECTLY COMMISSIONED BY NHS ENGLAND V14 CHANGES TO VERSION 13 PUBLISHED APRIL 2019 Changes to v13 Lines removed SUITABLE SPECIALIST FOR CENTRE SUITABLE FOR SHARED ONLY SHARED CARE CARE PRIOR (includng WITH PRIMARY BETWEEN STOPPING MONITORING/ AUDIT APPROVAL outreach CARE (IF DRUG NAME INDICATION COMMISSIONER PBR CATEGORY TA/POLICY STARTING CRITERIA SPECIALIST COMMENT CRITERIA REQUIREMENTS PROFORMA when SUPPORTED AND REQUIRED delivered as BY LOCAL SECONDARY part of a PRESCRIBING CARE VIA provider COMMITTEE) NETWORK network) MODEL PAEDIATRIC INDICATIONS (IN LINE WITH NHS ENGLAND AS PER ADULT TA'S (TA195, TA373, ABATACEPT NHS ENGLAND CYTOKINE MODULATORS NICE NICE NICE √ MEDICINES FOR CHILDREN TA375) POLICY) Now covered by comment 8 PAEDIATRIC INDICATIONS (IN AS PER TA455 OR ADULT TA'S (TA130 LINE WITH NHS ENGLAND (replaced by TA375), TA143 (repalced by ADALIMUMAB NHS ENGLAND CYTOKINE MODULATORS NICE NICE NICE AUDIT √ √ MEDICINES FOR CHILDREN TA383), TA146, TA187, TA199, TA329, POLICY) TA392, TA460) Now covered by comment 8 ALBUTREPENONACOG ALFA HAEMOPHILIA B PRODUCTS ON CMU Blood factor products simplified NHS ENGLAND BLOOD-RELATED PRODUCTS SSC 1652 SSC 1652 SSC 1652 √ FRAMEWORK to blood factor product VIII etc PAEDIATRIC INDICATIONS (IN LINE WITH NHS ENGLAND AS PER IFR AS PER IFR ANAKINRA NHS ENGLAND CYTOKINE MODULATORS NOT ROUTINELY COMMISSIONED AS PER IFR APPROVAL √ MEDICINES FOR CHILDREN APPROVAL APPROVAL POLICY) Now covered by comment 8 AS PER BCSH GUIDELINES ANTIHAEMOPHILIC FACTOR/VON -

Hypothalamic-Pituitary Axes
Hypothalamic-Pituitary Axes Hypothalamic Factors Releasing/Inhibiting Pituitary Anterior Pituitary Hormones Circulating ACTH PRL GH Hormones February 11, 2008 LH FSH TSH Posterior Target Pituitary Gland and Hormones Tissue Effects ADH, oxytocin The GH/IGF-I Axis Growth Hormone Somatostatin GHRH Hypothalamus • Synthesized in the anterior lobe of the pituitary gland in somatotroph cells PITUITARY • ~75% of GH in the pituitary and in circulation is Ghrelin 191 amino acid single chain peptide, 2 intra-molecular disulfide bonds GH Weight; 22kD • Amount of GH secreted: IGF-I Women: 500 µg/m2/day Synthesis IGF- I Men: 350 µg/m2/day LIVER Local IGF-I Synthesis CIRCULATION GH Secretion: Primarily Pulsatile Pattern of GH Secretion Regulation by two hypothalamic in a Healthy Adult hormones 25 Sleep 20 Growth - SMS Hormone 15 Somatostatin Releasing GHRH + GH (µg/L) Hormone Inhibitory of 10 Stimulatory of GH Secretion GH Secretion 05 0 GHRH induces GH Somatostatin: Decreases to allow 0900 2100 0900 synthesis and secretion Clocktime GH secretory in somatotrophs Bursts GH From: “Acromegaly” by Alan G. Harris, M.D. 1 Other Physiological Regulators of GH Secretion Pharmacologic Agents Used to Stimulate GH Secretion Amino Sleep Exercise Stress Acids Fasting Glucose Stimulate hypothalamic GHRH or Inhibit Somatostatin Hypothalamus GHRH SMS Hypoglycemia(Insulin) Pituitary L-dopa Arginine Clonidine GHRH + - SMS Pyridostigmine GH Target Tissues Metabolic & Growth Promoting GH Effects IGF-I Insulin-like growth factor I (IGF-I) Major Determinants of Circulating -

Long-Term Treatment with Pegvisomant
6 179 M Buchfelder and others Findings from pegvisomant use 179:6 419–427 Clinical Study in ACROSTUDY Long-term treatment with pegvisomant: observations from 2090 acromegaly patients in ACROSTUDY Michael Buchfelder1, Aart-Jan van der Lely2, Beverly M K Biller3, Susan M Webb4, Thierry Brue5, Christian J Strasburger6, Ezio Ghigo7, Cecilia Camacho-Hubner8, Kaijie Pan9, Joanne Lavenberg9, Peter Jönsson10 and Juliana H Hey-Hadavi8 1Department of Neurosurgery, University of Erlangen-Nürnberg, Erlangen, Germany, 2Department of Medicine, Erasmus University MC, Rotterdam, the Netherlands, 3Neuroendocrine Unit, Massachusetts General Hospital, Boston, Massachusetts, USA, 4Endocrinologia (Malalties de la Hipòfisi), Hospital Sant Pau, Universitat Autònoma de Barcelona (UAB), Barcelona, Spain, 5Department of Endocrinology, Centre de Référence des Maladies Rares d’Origine Hypophysaire, Hôpital de la Conception, Marseille, France, 6Department of Medicine for Endocrinology, Diabetes and Nutritional Correspondence Medicine, Charité Universitätsmedizin, Campus Mitte, Berlin, Germany, 7University Hospital Città Salute e Scienza, should be addressed Turin, Italy, 8Endocrine Care Global Medical Affairs, Pfizer Inc., New York City, New York, USA, 9Endocrine Care to M Buchfelder Global Clinical Affairs, Pfizer Inc., Collegeville, Pennsylvania, USA, and 10Endocrine Care, Pfizer Health AB, Email Sollentuna, Sweden Michael.Buchfelder@ uk-erlangen.de Abstract Objectives: ACROSTUDY is an international, non-interventional study of acromegaly patients treated with pegvisomant (PEGV), a growth hormone receptor antagonist and has been conducted since 2004 in 15 countries to study the long-term safety and efficacy of PEGV. This report comprises the second interim analysis of 2090 patients as of May 12, 2016. Methods: Descriptive analyses of safety, pituitary imaging and outcomes on PEGV treatment up to 12 years were performed. -

Laboratory Investigations in the Diagnosis and Follow-Up of GH
review Laboratory investigations in the diagnosis and follow-up of GH-related disorders 1 Medizinische Klinik und Poliklinik Katharina Schilbach1 IV, Klinikum der Universität http://orcid.org/0000-0002-8667-0296 München, Munich, Germany Martin Bidlingmaier1 http://orcid.org/0000-0002-4681-6668 ABSTRACT In addition to auxiological, clinical and metabolic features measurements of growth hormone (GH) and insulin-like growth factor I (IGF-I) complement our tools in diagnosis and follow-up of GH-related disorders. While comparably robust during the pre-analytical phase, measurement and interpretation of concentrations of both hormones can be challenging due to analytical issues and biological confounders. Assay methods differ in terms of antibody specificity, interference from binding proteins, reference preparations and sensitivity. GH assays have different specificity towards different GH- isoforms (e.g. 20 kDa GH, placental GH) and interference from the GH antagonist Pegvisomant. The efficacy to prevent binding protein interference is most important in IGF-I assays. Methodological differences between assays require that reference intervals and diagnostic cut-offs are assay-specific. Among biological variables, pubertal development and age are most relevant for IGF-I, making detailed Correspondence to: reference intervals mandatory for interpretation. GH has pulsatile secretion and short half-life. Its Martin Bidlingmaier concentration is modified by acute factors such as stress, exercise and sleep, but also by intake of oral Medizinische Klinik und Poliklinik IV Klinikum der Universität München estrogens and anthropometric factors (e.g. BMI). Other GH dependent biomarkers such as free IGF-I, Ziemssenstr. 1 IGF binding protein 3 (IGFBP 3) and acid labile subunit (ALS) have been proposed. -

Pegvaliase-Pqpz
Pharmacy Benefit Coverage Criteria Effective Date………….………….....................12/1/2020 Next Review Date………………………………. 12/1/2021 Coverage Policy Number ................................ P0055 Pegvaliase-pqpz Table of Contents Related Coverage Resources Medical Necessity Criteria ................................... 1 Sapropterin FDA Approved Indications ................................... 2 Recommended Dosing ........................................ 2 General Background ............................................ 3 References .......................................................... 3 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage Policy. In the event of a conflict, a customer’s