And Consensus-Based Recommendations for the Use of Pegvaliase in Adults with Phenylketonuria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
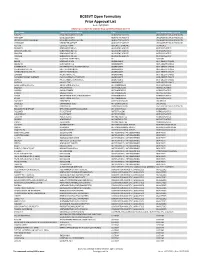
BCBSVT Open Formulary Prior Approval List
BCBSVT Open Formulary Prior Approval List As of: 10/27/2020 Helpful Tip: To search for a specific drug, use the find feature (Ctrl + F) Trade Name Chemical/Biological Name Class Prior Authorization Program FUSILEV LEVOLEUCOVORIN CALCIUM ADJUNCTIVE AGENTS UNCLASSIFIED DRUG PRODUCTS KHAPZORY LEVOLEUCOVORIN ADJUNCTIVE AGENTS UNCLASSIFIED DRUG PRODUCTS LEVOLEUCOVORIN CALCIUM LEVOLEUCOVORIN CALCIUM ADJUNCTIVE AGENTS UNCLASSIFIED DRUG PRODUCTS VISTOGARD URIDINE TRIACETATE ADJUNCTIVE AGENTS UNCLASSIFIED DRUG PRODUCTS ACTHAR CORTICOTROPIN ADRENAL HORMONES HORMONES BELRAPZO BENDAMUSTINE HCL ALKYLATING AGENTS ANTINEOPLASTICS BENDAMUSTINE HCL BENDAMUSTINE HCL ALKYLATING AGENTS ANTINEOPLASTICS BENDEKA BENDAMUSTINE HCL ALKYLATING AGENTS ANTINEOPLASTICS TREANDA BENDAMUSTINE HCL ALKYLATING AGENTS ANTINEOPLASTICS DAW (DISPENSE AS WRITTEN) ALL CUSTOM BELVIQ LORCASERIN HCL ANOREXIANTS ANTI‐OBESITY DRUGS BELVIQ XR LORCASERIN HCL ANOREXIANTS ANTI‐OBESITY DRUGS CONTRAVE ER NALTREXONE HCL/BUPROPION HCL ANOREXIANTS ANTI‐OBESITY DRUGS DIETHYLPROPION HCL DIETHYLPROPION HCL ANOREXIANTS ANTI‐OBESITY DRUGS DIETHYLPROPION HCL ER DIETHYLPROPION HCL ANOREXIANTS ANTI‐OBESITY DRUGS LOMAIRA PHENTERMINE HCL ANOREXIANTS ANTI‐OBESITY DRUGS PHENDIMETRAZINE TARTRATE PHENDIMETRAZINE TARTRATE ANOREXIANTS ANTI‐OBESITY DRUGS QSYMIA PHENTERMINE/TOPIRAMATE ANOREXIANTS ANTI‐OBESITY DRUGS SAXENDA LIRAGLUTIDE ANOREXIANTS ANTI‐OBESITY DRUGS ABIRATERONE ACETATE ABIRATERONE ACETATE ANTIANDROGENS ANTINEOPLASTICS ERLEADA APALUTAMIDE ANTIANDROGENS ANTINEOPLASTICS NUBEQA DAROLUTAMIDE ANTIANDROGENS -

DRUGS REQUIRING PRIOR AUTHORIZATION in the MEDICAL BENEFIT Page 1
Effective Date: 08/01/2021 DRUGS REQUIRING PRIOR AUTHORIZATION IN THE MEDICAL BENEFIT Page 1 Therapeutic Category Drug Class Trade Name Generic Name HCPCS Procedure Code HCPCS Procedure Code Description Anti-infectives Antiretrovirals, HIV CABENUVA cabotegravir-rilpivirine C9077 Injection, cabotegravir and rilpivirine, 2mg/3mg Antithrombotic Agents von Willebrand Factor-Directed Antibody CABLIVI caplacizumab-yhdp C9047 Injection, caplacizumab-yhdp, 1 mg Cardiology Antilipemic EVKEEZA evinacumab-dgnb C9079 Injection, evinacumab-dgnb, 5 mg Cardiology Hemostatic Agent BERINERT c1 esterase J0597 Injection, C1 esterase inhibitor (human), Berinert, 10 units Cardiology Hemostatic Agent CINRYZE c1 esterase J0598 Injection, C1 esterase inhibitor (human), Cinryze, 10 units Cardiology Hemostatic Agent FIRAZYR icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent HAEGARDA c1 esterase J0599 Injection, C1 esterase inhibitor (human), (Haegarda), 10 units Cardiology Hemostatic Agent ICATIBANT (generic) icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent KALBITOR ecallantide J1290 Injection, ecallantide, 1 mg Cardiology Hemostatic Agent RUCONEST c1 esterase J0596 Injection, C1 esterase inhibitor (recombinant), Ruconest, 10 units Injection, lanadelumab-flyo, 1 mg (code may be used for Medicare when drug administered under Cardiology Hemostatic Agent TAKHZYRO lanadelumab-flyo J0593 direct supervision of a physician, not for use when drug is self-administered) Cardiology Pulmonary Arterial Hypertension EPOPROSTENOL (generic) -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Oregon Medicaid Pharmaceutical Services Prior Authorization Criteria
Oregon Medicaid Pharmaceutical Services Prior Authorization Criteria HEALTH SYSTEMS DIVISION Prior authorization (PA) criteria for fee-for-service prescriptions for Oregon Health Plan clients March 1, 2021 Contents Contents ................................................................................................................................................................ 2 Introduction........................................................................................................................................................... 7 About this guide ......................................................................................................................................... 7 How to use this guide ................................................................................................................................. 7 Administrative rules and supplemental information .................................................................................. 7 Update information............................................................................................................................................... 8 Effective March 1, 2021 ............................................................................................................................ 8 Substantive updates and new criteria ............................................................................................. 8 Clerical changes ............................................................................................................................ -

Medicines Not Reimbursed Through National Prices and Directly Commissioned by Nhs England V14 Changes to Version 13
MEDICINES NOT REIMBURSED THROUGH NATIONAL PRICES AND DIRECTLY COMMISSIONED BY NHS ENGLAND V14 CHANGES TO VERSION 13 PUBLISHED APRIL 2019 Changes to v13 Lines removed SUITABLE SPECIALIST FOR CENTRE SUITABLE FOR SHARED ONLY SHARED CARE CARE PRIOR (includng WITH PRIMARY BETWEEN STOPPING MONITORING/ AUDIT APPROVAL outreach CARE (IF DRUG NAME INDICATION COMMISSIONER PBR CATEGORY TA/POLICY STARTING CRITERIA SPECIALIST COMMENT CRITERIA REQUIREMENTS PROFORMA when SUPPORTED AND REQUIRED delivered as BY LOCAL SECONDARY part of a PRESCRIBING CARE VIA provider COMMITTEE) NETWORK network) MODEL PAEDIATRIC INDICATIONS (IN LINE WITH NHS ENGLAND AS PER ADULT TA'S (TA195, TA373, ABATACEPT NHS ENGLAND CYTOKINE MODULATORS NICE NICE NICE √ MEDICINES FOR CHILDREN TA375) POLICY) Now covered by comment 8 PAEDIATRIC INDICATIONS (IN AS PER TA455 OR ADULT TA'S (TA130 LINE WITH NHS ENGLAND (replaced by TA375), TA143 (repalced by ADALIMUMAB NHS ENGLAND CYTOKINE MODULATORS NICE NICE NICE AUDIT √ √ MEDICINES FOR CHILDREN TA383), TA146, TA187, TA199, TA329, POLICY) TA392, TA460) Now covered by comment 8 ALBUTREPENONACOG ALFA HAEMOPHILIA B PRODUCTS ON CMU Blood factor products simplified NHS ENGLAND BLOOD-RELATED PRODUCTS SSC 1652 SSC 1652 SSC 1652 √ FRAMEWORK to blood factor product VIII etc PAEDIATRIC INDICATIONS (IN LINE WITH NHS ENGLAND AS PER IFR AS PER IFR ANAKINRA NHS ENGLAND CYTOKINE MODULATORS NOT ROUTINELY COMMISSIONED AS PER IFR APPROVAL √ MEDICINES FOR CHILDREN APPROVAL APPROVAL POLICY) Now covered by comment 8 AS PER BCSH GUIDELINES ANTIHAEMOPHILIC FACTOR/VON -

The Role of Epinephrine in the Treatment of Anaphylaxis Anne K
The Role of Epinephrine in the Treatment of Anaphylaxis Anne K. Ellis, MD, and James H. Day, MD, FRCP(C) Address Beneficial Effects of Epinephrine Division of Allergy, Kingston General Hospital, 76 Stuart Street, in Anaphylaxis Kingston, ON K7L 2V7, Canada. Epinephrine is both an alpha (α) and a beta (β) adrener- E-mail: [email protected] gic receptor agonist. Through α-adrenergic stimulation, Current Allergy and Asthma Reports 2003, 3:11–14 epinephrine increases peripheral vascular resistance, Current Science Inc. ISSN 1529-7322 Copyright © 2003 by Current Science Inc. improving blood pressure and coronary artery perfusion, reversing peripheral vasodilation, and decreasing angioedema and urticaria [5]. β-1 adrenergic stimulation Epinephrine is the cornerstone of anaphylaxis manage- has positive inotropic and chronotropic effects on the ment. Its administration should be immediate upon evi- myocardium, and β-2 adrenergic effects include bron- dence of the occurrence of anaphylaxis. Delays in chodilation [6]. β-adrenergic receptors also increase administration may be fatal. The most appropriate admin- intracellular cyclic adenosine monophosphate (cAMP) istration is 0.3 to 0.5 mL of 1:1000 dilution intramuscu- production in mast cells and basophils, which inhibits larly for adults and 0.01 mg/kg for children, given in the further inflammatory mediator release [7,8]. lateral thigh. Patients with known anaphylactic reactivity should be prescribed an epinephrine auto-injector to be carried at all times for treatment of potential recur- Dosage and Routes of Administration rences. Education of the patient or parent regarding the for Epinephrine proper use of this tool is paramount. Some discrepancy exists in the literature concerning the appropriate dosage of epinephrine for anaphylaxis. -

Guideline (S2k) on Acute Therapy and Management of Anaphylaxis: 2021 Update
guidelines Allergo J Int (2021) 30:1–25 https://doi.org/10.1007/s40629-020-00158-y Guideline (S2k) on acute therapy and management of anaphylaxis: 2021 update S2k-Guideline of the German Society for Allergology and Clinical Immunology (DGAKI), the Medical Association of German Allergologists (AeDA), the Society of Pediatric Allergology and Environmental Medicine (GPA), the German Academy of Allergology and Environmental Medicine (DAAU), the German Professional Association of Pediatricians (BVKJ), the Society for Neonatology and Pediatric Intensive Care (GNPI), the German Society of Dermatology (DDG), the Austrian Society for Allergology and Immunology (ÖGAI), the Swiss Society for Allergy and Immunology (SGAI), the German Society of Anaesthesiology and Intensive Care Medicine (DGAI), the German Society of Pharmacology (DGP), the German Respiratory Society (DGP), the patient organization German Allergy and Asthma Association (DAAB), the German Working Group of Anaphylaxis Training and Education (AGATE) Johannes Ring · Kirsten Beyer · Tilo Biedermann · Andreas Bircher · Matthias Fischer · Thomas Fuchs · Axel Heller · Florian Hoffmann · Isidor Huttegger · Thilo Jakob · Ludger Klimek · Matthias V. Kopp · Claudia Kugler · Lars Lange · Oliver Pfaar · Ernst Rietschel · Franziska Rueff · Sabine Schnadt · Roland Seifert · Britta Stöcker · Regina Treudler · Christian Vogelberg · Thomas Werfel · Margitta Worm · Helmut Sitter · Knut Brockow Published online: 28 January 2021 © The Author(s) 2021 Keywords Anaphylaxis · Food allergy · Drug LT Leukotriene -

Mutasem Rawas.Qalaji
FORMULATION AND ASSESSMENT OF FAST- DISINTEGRATING SUBLINGUAL EPINEPHRINE TABLETS FOR TI.IE POTENTIAI- EMERGENCY TREATMENT OF ANAPHYLAXIS By MUTASEM RAWAS.QALAJI A THESIS SUBMITTED TO THE FACULTY OF GRADUATE STUDIES IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY FACULTY OF PHARMACY UNIVERSITY OF MANITOBA WINNIPEG, MANITOBA, CANADA JUNE, 2006 THE UNIVERSITY OF MANITOBA FACULTY OF GRADUATE STUDIES COPYRIGHT PERMISSION Formulation and Assessment of Fast-Disintegrating Sublingual Epinephrine Tablets for the Potential Emergency Treatment of Anaphylaxis By Mutasem Rawas-Qalaji A Thesis/Practicum submitted to the Faculty of Graduate Studies of The University of Manitoba in partial fïlfitlment of the requirement of the degree of Doctor of Philosophy Mutasem Rawas-Qalaji @ 2006 Permission has been granted to the Library of the University of Manitoba to lend or sell copies of this thesis/practicum, to the National Library of Canada to microfilm this thesis and to lend or sell copies of the film, and to University Microfilms Inc. to publish an abstract of this thesis/practicum. This reproduction or copy of this thesis has been made available by authority of the copyright owner solely for the purpose of private study and research, and may only be reproduced and copied as permitted by copyright laws or with express written authorization from the copyright o\ilner. DEDICATION To my father Mohamad Rawas-ealaji and my mother wedad Duqsi (in memoriam) lwould like to dedicate this work. ABSTRACT Objectives; To formulate, characterize, and evaluate the stability of sublingual (sL) epinephrine (E) tablets that are bioequivatent to E 0.3 mg intramuscular injection (lM) for the feasibility of SL E administration for the potential out-of-hospital emergency treatment of anaphylaxis. -

Pegvaliase-Pqpz
Pharmacy Benefit Coverage Criteria Effective Date………….………….....................12/1/2020 Next Review Date………………………………. 12/1/2021 Coverage Policy Number ................................ P0055 Pegvaliase-pqpz Table of Contents Related Coverage Resources Medical Necessity Criteria ................................... 1 Sapropterin FDA Approved Indications ................................... 2 Recommended Dosing ........................................ 2 General Background ............................................ 3 References .......................................................... 3 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage Policy. In the event of a conflict, a customer’s -

2019 Express Scripts National Preferred Formulary
The following is a list of the most commonly prescribed drugs. It represents an abbreviated version of the drug list (formulary) that is at the core of your prescription plan. The list is not all-inclusive and does not guarantee coverage. In addition to using this list, you are encouraged to ask your doctor to prescribe generic drugs whenever appropriate. 2019 Express Scripts PLEASE NOTE: Brand-name drugs may move to nonformulary status if a generic version becomes available during the year. Not all the drugs listed are covered by National Preferred Formulary all prescription plans; check your benefit materials for the specific drugs covered and the copayments for your prescription plan. For specific questions about your coverage, please call the phone number printed on your member ID card. KEY BD AUTOSHIELD clonidine enalapril GENOTROPIN [INJ] [INJ] - Injectable Drug DUO NEEDLES clopidogrel ENBREL [INJ] GENVOYA Brand-name drugs are listed BD ULTRAFINE clotrimazole/betamethasone enoxaparin [INJ] GILENYA in CAPITAL letters. INSULIN SYRINGES dipropionate ENSTILAR GILOTRIF Generic drugs are listed BD ULTRAFINE PEN NEEDLES COLCRYS ENTRESTO glimepiride in lower case letters. BELBUCA COMBIGAN EPCLUSA glipizide benazepril COMBIPATCH EPIDIOLEX glipizide ext-release A benzonatate COMBIVENT RESPIMAT EPIDUO FORTE GLUCAGEN [INJ] BEPREVE COPAXONE 40 MG [INJ] epinephrine autoinjector GLUCAGON [INJ] ABILIFY MAINTENA [INJ] BETASERON [INJ] CORLANOR (by Mylan) [INJ] glyburide ABSORICA BETHKIS COSENTYX [INJ] EPIPEN, EPIPEN JR [INJ] GLYXAMBI ACANYA BEVESPI -

Pharmacy Laws on Epinephrine Autoinjectors
Pharmacy Laws on Epinephrine Autoinjectors Updated 1/13/2020 Ohio has several laws intended to promote the accessibility of epinephrine autoinjectors. This document will provide a general overview of the following laws: . Section 4729.382 - Pharmacist's authority to dispense an epinephrine autoinjector by substitution. Section 4729.47 - Authority to dispense epinephrine without a prescription (FAQ starts on page 5 of this document). For questions regarding either provision, please review the following frequently asked questions. If you need additional information, the most expedient way to have your questions answered will be to e-mail the Board office by visiting: http://www.pharmacy.ohio.gov/contact.aspx. Section 4729.382 - Pharmacist's authority to dispense an epinephrine autoinjector by substitution. Section 4729.382 of the Ohio Revised Code expands a pharmacist’s ability to substitute epinephrine autoinjectors. NOTE: Nothing in this provision applies to the following: . Generic substitution of products deemed as being therapeutically equivalent in the FDA Orange Book and in accordance with section 4729.38 of the Revised Code; or . Obtaining a new verbal prescription from a prescriber for a different epinephrine autoinjector. Q1) Under what circumstances am I permitted to substitute the prescribed autoinjector? In addition to generic substitution (i.e. an AB rating in the Orange Book), epinephrine autoinjector substitution may occur if the form of epinephrine in the dispensed autoinjector, when compared to the form of the drug in the prescribed autoinjector, complies with all the following: 1. Is a pharmaceutical equivalent of the form of epinephrine in the type of autoinjector that was prescribed in that it contains identical amounts of the identical active ingredients, but not necessarily the same inactive ingredients. -

Specialty Pharmacy Program Drug List
Specialty Pharmacy Program Drug List The Specialty Pharmacy Program covers certain drugs commonly referred to as high-cost Specialty Drugs. To receive in- network benefits/coverage for these drugs, these drugs must be dispensed through a select group of contracted specialty pharmacies or your medical provider. Please call the BCBSLA Customer Service number on the back of your member ID card for information about our contracted specialty pharmacies. All specialty drugs listed below are limited to the retail day supply listed in your benefit plan (typically a 30-day supply). As benefits may vary by group and individual plans, the inclusion of a medication on this list does not imply prescription drug coverage. Please refer to your benefit plan for a complete list of benefits, including specific exclusions, limitations and member cost-sharing amounts you are responsible for such as a deductible, copayment and coinsurance. Brand Name Generic Name Drug Classification 8-MOP methoxsalen Psoralen ACTEMRA SC tocilizumab Monoclonal Antibody/Arthritis ACTHAR corticotropin Adrenocortical Insufficiency ACTIMMUNE interferon gamma 1b Interferon ADCIRCA tadalafil Pulmonary Vasodilator ADEMPAS riociguat Pulmonary Vasodilator AFINITOR everolimus Oncology ALECENSA alectinib Oncology ALKERAN (oral) melphalan Oncology ALUNBRIG brigatinib Oncology AMPYRA ER dalfampridine Multiple Sclerosis APTIVUS tipranavir HIV/AIDS APOKYN apomorphine Parkinson's Disease ARCALYST rilonacept Interleukin Blocker/CAPS ATRIPLA efavirenz-emtricitabine-tenofovir HIV/AIDS AUBAGIO