Traditional Chinese Medicine Induced Liver Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Read Ebook / Pharmacy Informatics(Chinese Edition
5I7BMFUE1048 » Kindle » Pharmacy Informatics(Chinese Edition) Download PDF Online PHARMACY INFORMATICS(CHINESE EDITION) To read Pharmacy Informatics(Chinese Edition) PDF, make sure you refer to the hyperlink listed below and download the ebook or get access to other information which might be have conjunction with PHARMACY INFORMATICS(CHINESE EDITION) ebook. Download PDF Pharmacy Informatics(Chinese Edition) Authored by HU JIN HONG . CHU WEN GONG Released at - Filesize: 2.87 MB Reviews Unquestionably, this is the greatest operate by any article writer. I could comprehended everything out of this written e ebook. Your way of life span will be transform as soon as you total reading this book. -- Andy Erdman Very useful to all class of individuals. It is amongst the most awesome publication i actually have read through. You will like just how the blogger create this pdf. -- Lisa Jacobs Undoubtedly, this is actually the nest work by any author. Of course, it is perform, nonetheless an amazing and interesting literature. You will like just how the article writer publish this book. -- Dr. Isom Dibbert Jr. TERMS | DMCA IEQX7URS9TR8 » Doc » Pharmacy Informatics(Chinese Edition) Related Books Found around the world : pay attention to safety(Chinese Edition) Plants vs. Zombies game book - to play the stickers 2 (puzzle game swept the world. most played together(Chinese Edition) Genuine the book spiritual growth of children picture books: let the children learn to say no the A Bofu (AboffM)(Chinese Edition) 365 the night before going to bed good story books Mall genuine Wenxuan network(Chinese Edition) 0-4 years old baby enlightening story picture book set: Bedtime volume (latest edition to enlarge marked phonetic characters large capacity enlightenment small language)(Chinese Edition). -

Is Shuma the Chinese Analog of Soma/Haoma? a Study of Early Contacts Between Indo-Iranians and Chinese
SINO-PLATONIC PAPERS Number 216 October, 2011 Is Shuma the Chinese Analog of Soma/Haoma? A Study of Early Contacts between Indo-Iranians and Chinese by ZHANG He Victor H. Mair, Editor Sino-Platonic Papers Department of East Asian Languages and Civilizations University of Pennsylvania Philadelphia, PA 19104-6305 USA [email protected] www.sino-platonic.org SINO-PLATONIC PAPERS FOUNDED 1986 Editor-in-Chief VICTOR H. MAIR Associate Editors PAULA ROBERTS MARK SWOFFORD ISSN 2157-9679 (print) 2157-9687 (online) SINO-PLATONIC PAPERS is an occasional series dedicated to making available to specialists and the interested public the results of research that, because of its unconventional or controversial nature, might otherwise go unpublished. The editor-in-chief actively encourages younger, not yet well established, scholars and independent authors to submit manuscripts for consideration. Contributions in any of the major scholarly languages of the world, including romanized modern standard Mandarin (MSM) and Japanese, are acceptable. In special circumstances, papers written in one of the Sinitic topolects (fangyan) may be considered for publication. Although the chief focus of Sino-Platonic Papers is on the intercultural relations of China with other peoples, challenging and creative studies on a wide variety of philological subjects will be entertained. This series is not the place for safe, sober, and stodgy presentations. Sino- Platonic Papers prefers lively work that, while taking reasonable risks to advance the field, capitalizes on brilliant new insights into the development of civilization. Submissions are regularly sent out to be refereed, and extensive editorial suggestions for revision may be offered. Sino-Platonic Papers emphasizes substance over form. -

Inscriptional Records of the Western Zhou
INSCRIPTIONAL RECORDS OF THE WESTERN ZHOU Robert Eno Fall 2012 Note to Readers The translations in these pages cannot be considered scholarly. They were originally prepared in early 1988, under stringent time pressures, specifically for teaching use that term. Although I modified them sporadically between that time and 2012, my final year of teaching, their purpose as course materials, used in a week-long classroom exercise for undergraduate students in an early China history survey, did not warrant the type of robust academic apparatus that a scholarly edition would have required. Since no broad anthology of translations of bronze inscriptions was generally available, I have, since the late 1990s, made updated versions of this resource available online for use by teachers and students generally. As freely available materials, they may still be of use. However, as specialists have been aware all along, there are many imperfections in these translations, and I want to make sure that readers are aware that there is now a scholarly alternative, published last month: A Source Book of Ancient Chinese Bronze Inscriptions, edited by Constance Cook and Paul Goldin (Berkeley: Society for the Study of Early China, 2016). The “Source Book” includes translations of over one hundred inscriptions, prepared by ten contributors. I have chosen not to revise the materials here in light of this new resource, even in the case of a few items in the “Source Book” that were contributed by me, because a piecemeal revision seemed unhelpful, and I am now too distant from research on Western Zhou bronzes to undertake a more extensive one. -

Originally, the Descendants of Hua Xia Were Not the Descendants of Yan Huang
E-Leader Brno 2019 Originally, the Descendants of Hua Xia were not the Descendants of Yan Huang Soleilmavis Liu, Activist Peacepink, Yantai, Shandong, China Many Chinese people claimed that they are descendants of Yan Huang, while claiming that they are descendants of Hua Xia. (Yan refers to Yan Di, Huang refers to Huang Di and Xia refers to the Xia Dynasty). Are these true or false? We will find out from Shanhaijing ’s records and modern archaeological discoveries. Abstract Shanhaijing (Classic of Mountains and Seas ) records many ancient groups of people in Neolithic China. The five biggest were: Yan Di, Huang Di, Zhuan Xu, Di Jun and Shao Hao. These were not only the names of groups, but also the names of individuals, who were regarded by many groups as common male ancestors. These groups first lived in the Pamirs Plateau, soon gathered in the north of the Tibetan Plateau and west of the Qinghai Lake and learned from each other advanced sciences and technologies, later spread out to other places of China and built their unique ancient cultures during the Neolithic Age. The Yan Di’s offspring spread out to the west of the Taklamakan Desert;The Huang Di’s offspring spread out to the north of the Chishui River, Tianshan Mountains and further northern and northeastern areas;The Di Jun’s and Shao Hao’s offspring spread out to the middle and lower reaches of the Yellow River, where the Di Jun’s offspring lived in the west of the Shao Hao’s territories, which were near the sea or in the Shandong Peninsula.Modern archaeological discoveries have revealed the authenticity of Shanhaijing ’s records. -

Five Phases Belief in Chu 楚: Sacrificing White Dogs to Save The
Name: Xueying Kong Department: East Asian Languages and Literatures 30th Hayes Graduate Research Forum (February, 2016) Five Phases Belief in Chu 楚: Sacrificing White Dogs to Save the Kingdom? Abstract: This paper is a corpus-based study on excavated bamboo-slip inscriptions from Chu state around 700 BCE. -300 BCE. It examines in detail a particular sacrifice made of white dogs and the historical and religious contexts for this ritual. The results show that this occult practice was performed as part of the five-god ritual system of Chu state. In the ritual Chu people singled out white dogs as appropriate sacrifice because in their belief, the energy flow from white dogs were able to destroy Chu state. The whole idea was based on the Five Phases theory, which served as a logical foundation for many cultural practices and social custom in early China. Key words: White dog sacrifice, five phases theory, Chu Bamboo-slip Inscriptions, five-god ritual system Introduction “Offering on the road a white dog, wine, and food as sacrifice,” reads a bamboo strip from Chu state (770BCE.-223 BCE.) in ancient China. 1 The same sentence or sentence structure with a dog (usually white) in it, recurs frequently in other bamboo slips from this time. For example, on bamboo slip No. 229 from Bao-shan Mountain, it reads: “making a sacrifice with a white dog, wine, and food” (Figure 2). Bamboo slip No. 233 says: “making sacrifice with a white dog, wine and food, killing the white dog at the main gate” (Figure 3). Bamboo-slip inscriptions (hereafter BSI) are one of the earliest types of written Chinese.2 From the beginning of 20th century, BSI have been unearthed from multiple ancient tombs, creating successive archeological sensations in China. -
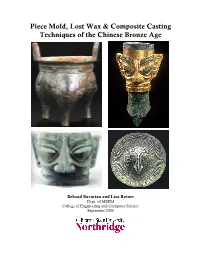
Piece Mold, Lost Wax & Composite Casting Techniques of The
Piece Mold, Lost Wax & Composite Casting Techniques of the Chinese Bronze Age Behzad Bavarian and Lisa Reiner Dept. of MSEM College of Engineering and Computer Science September 2006 Table of Contents Abstract Approximate timeline 1 Introduction 2 Bronze Transition from Clay 4 Elemental Analysis of Bronze Alloys 4 Melting Temperature 7 Casting Methods 8 Casting Molds 14 Casting Flaws 21 Lost Wax Method 25 Sanxingdui 28 Environmental Effects on Surface Appearance 32 Conclusion 35 References 36 China can claim a history rich in over 5,000 years of artistic, philosophical and political advancement. As well, it is birthplace to one of the world's oldest and most complex civilizations. By 1100 BC, a high level of artistic and technical skill in bronze casting had been achieved by the Chinese. Bronze artifacts initially were copies of clay objects, but soon evolved into shapes invoking bronze material characteristics. Essentially, the bronze alloys represented in the copper-tin-lead ternary diagram are not easily hot or cold worked and are difficult to shape by hammering, the most common techniques used by the ancient Europeans and Middle Easterners. This did not deter the Chinese, however, for they had demonstrated technical proficiency with hard, thin walled ceramics by the end of the Neolithic period and were able to use these skills to develop a most unusual casting method called the piece mold process. Advances in ceramic technology played an influential role in the progress of Chinese bronze casting where the piece mold process was more of a technological extension than a distinct innovation. Certainly, the long and specialized experience in handling clay was required to form the delicate inscriptions, to properly fit the molds together and to prevent them from cracking during the pour. -

Official Colours of Chinese Regimes: a Panchronic Philological Study with Historical Accounts of China
TRAMES, 2012, 16(66/61), 3, 237–285 OFFICIAL COLOURS OF CHINESE REGIMES: A PANCHRONIC PHILOLOGICAL STUDY WITH HISTORICAL ACCOUNTS OF CHINA Jingyi Gao Institute of the Estonian Language, University of Tartu, and Tallinn University Abstract. The paper reports a panchronic philological study on the official colours of Chinese regimes. The historical accounts of the Chinese regimes are introduced. The official colours are summarised with philological references of archaic texts. Remarkably, it has been suggested that the official colours of the most ancient regimes should be the three primitive colours: (1) white-yellow, (2) black-grue yellow, and (3) red-yellow, instead of the simple colours. There were inconsistent historical records on the official colours of the most ancient regimes because the composite colour categories had been split. It has solved the historical problem with the linguistic theory of composite colour categories. Besides, it is concluded how the official colours were determined: At first, the official colour might be naturally determined according to the substance of the ruling population. There might be three groups of people in the Far East. (1) The developed hunter gatherers with livestock preferred the white-yellow colour of milk. (2) The farmers preferred the red-yellow colour of sun and fire. (3) The herders preferred the black-grue-yellow colour of water bodies. Later, after the Han-Chinese consolidation, the official colour could be politically determined according to the main property of the five elements in Sino-metaphysics. The red colour has been predominate in China for many reasons. Keywords: colour symbolism, official colours, national colours, five elements, philology, Chinese history, Chinese language, etymology, basic colour terms DOI: 10.3176/tr.2012.3.03 1. -

The Rituals of Zhou in East Asian History
STATECRAFT AND CLASSICAL LEARNING: THE RITUALS OF ZHOU IN EAST ASIAN HISTORY Edited by Benjamin A. Elman and Martin Kern CHAPTER FOUR CENTERING THE REALM: WANG MANG, THE ZHOULI, AND EARLY CHINESE STATECRAFT Michael Puett, Harvard University In this chapter I address a basic problem: why would a text like the Rituals of Zhou (Zhouli !"), which purports to describe the adminis- trative structure of the Western Zhou ! dynasty (ca. 1050–771 BCE), come to be employed by Wang Mang #$ (45 BCE–23 CE) and, later, Wang Anshi #%& (1021–1086) in projects of strong state cen- tralization? Answering this question for the case of Wang Mang, how- ever, is no easy task. In contrast to what we have later for Wang Anshi, there are almost no sources to help us understand precisely how Wang Mang used, appropriated, and presented the Zhouli. We are told in the History of the [Western] Han (Hanshu '() that Wang Mang em- ployed the Zhouli, but we possess no commentaries on the text by ei- ther Wang Mang or one of his associates. In fact, we have no full commentary until Zheng Xuan )* (127–200 CE), who was far re- moved from the events of Wang Mang’s time and was concerned with different issues. Even the statements in the Hanshu about the uses of the Zhouli— referred to as the Offices of Zhou (Zhouguan !+) by Wang Mang— are brief. We are told that Wang Mang changed the ritual system of the time to follow that of the Zhouguan,1 that he used the Zhouguan for the taxation system,2 and that he used the Zhouguan, along with the “The Regulations of the King” (“Wangzhi” #,) chapter of the Records of Ritual (Liji "-), to organize state offices.3 I propose to tackle this problem in a way that is admittedly highly speculative. -
Views of the Qin Instructor: Anthony Barbieri-Low Tuesdays, 9:00Am-11:50 Am Office: HSSB 4225 Location: HSSB 2252 Office Hours: Mon
History 184R: Views of the Qin Instructor: Anthony Barbieri-Low Tuesdays, 9:00am-11:50 am Office: HSSB 4225 Location: HSSB 2252 Office hours: Mon. 12:00-2:00 pm [email protected] Course Description: The Qin Dynasty (221-207 BC) was the first imperial house to rule the bulk of the territory we now think of as China. The Qin established the pattern for the imperial bureaucratic state that would rule China for the next two thousand years, and its unification of the various written scripts and metal currencies of feudal China ensured the cultural and economic unification of the land as well. But the Qin Dynasty has also been disparaged by later writers for its harsh laws, its excessive labor mobilizations, the autocratic rule of its emperors, and of course, the famous “burning of the books,” one of the most notorious literary inquisitions in history. In this course, students will look at the Qin Dynasty from a wide variety of perspectives. They will come to learn how this brief period in Chinese history has been viewed by later authors and through the lens of contemporary culture. The types of material that students will read or view in this course include primary historical documents, legal codes and casebooks, legends and literature, historical essays, archaeological materials, historical fiction, movies, comic books, and video games. Course Goals: The primary purpose of this course is to train you in the research and writing of a polished historical paper. This course will take you through the stages of a complete research paper -

Proof of Investors' Binding Borrowing Constraint Appendix 2: System Of
Appendix 1: Proof of Investors’ Binding Borrowing Constraint PROOF: Use the Kuhn-Tucker condition to check whether the collateral constraint is binding. We have h I RI I mt[mt pt ht + ht − bt ] = 0 If (11) is not binding, then mt = 0: We can write the investor’s FOC Equation (18) as: I I I I h I I I I i Ut;cI ct ;ht ;nt = bIEt (1 + it)Ut+1;cI ct+1;ht+1;nt+1 (42) At steady state, we have bI (1 + i) = 1 However from (6); we know bR (1 + i) = 1 at steady state. With parameter restrictions that bR > bI; therefore bI (1 + i) < 1; contradiction. Therefore we cannot have mt = 0: Therefore, mt > 0; and I h I RI thus we have bt = mt pt ht + ht : Q.E.D. Appendix 2: System of Steady-State Conditions This appendix lays out the system of equilibrium conditions in steady state. Y cR + prhR = + idR (43) N R R R r R R R UhR c ;h = pt UcR c ;h (44) R R R R R R UnR c ;h = −WUcR c ;h (45) 1 = bR(1 + i) (46) Y cI + phd hI + hRI + ibI = + I + prhRI (47) t N I I I h I I I h [1 − bI (1 − d)]UcI c ;h p = UhI c ;h + mmp (48) I I I h I I I r h [1 − bI (1 − d)]UcI c ;h p = UcI c ;h p + mmp (49) I I I [1 − bI (1 + i)]UcI c ;h = m (50) bI = mphhI (51) 26 ©International Monetary Fund. -

(And Misreading) the Draft Constitution in China, 1954
Textual Anxiety Reading (and Misreading) the Draft Constitution in China, 1954 ✣ Neil J. Diamant and Feng Xiaocai In 1927, Mao Zedong famously wrote that a revolution is “not the same as inviting people to dinner” and is instead “an act of violence whereby one class overthrows the authority of another.” From the establishment of the People’s Republic of China (PRC) in 1949 until Mao’s death in 1976, his revolutionary vision became woven into the fabric of everyday life, but few years were as violent as the early 1950s.1 Rushing to consolidate power after finally defeating the Nationalist Party (Kuomintang, or KMT) in a decades- long power struggle, the Chinese Communist Party (CCP) threatened the lives and livelihood of millions. During the Land Reform Campaign (1948– 1953), landowners, “local tyrants,” and wealthier villagers were targeted for repression. In the Campaign to Suppress Counterrevolutionaries in 1951, the CCP attacked former KMT activists, secret society and gang members, and various “enemy agents.”2 That same year, university faculty and secondary school teachers were forced into “thought reform” meetings, and businessmen were harshly investigated during the “Five Antis” Campaign in 1952.3 1. See Mao’s “Report of an Investigation into the Peasant Movement in Hunan,” in Stuart Schram, ed., The Political Thought of Mao Tse-tung (New York: Praeger, 1969), pp. 252–253. Although the Cultural Revolution (1966–1976) was extremely violent, the death toll, estimated at roughly 1.5 million, paled in comparison to that of the early 1950s. The nearest competitor is 1958–1959, during the Great Leap Forward. -

The Later Han Empire (25-220CE) & Its Northwestern Frontier
University of Pennsylvania ScholarlyCommons Publicly Accessible Penn Dissertations 2012 Dynamics of Disintegration: The Later Han Empire (25-220CE) & Its Northwestern Frontier Wai Kit Wicky Tse University of Pennsylvania, [email protected] Follow this and additional works at: https://repository.upenn.edu/edissertations Part of the Asian History Commons, Asian Studies Commons, and the Military History Commons Recommended Citation Tse, Wai Kit Wicky, "Dynamics of Disintegration: The Later Han Empire (25-220CE) & Its Northwestern Frontier" (2012). Publicly Accessible Penn Dissertations. 589. https://repository.upenn.edu/edissertations/589 This paper is posted at ScholarlyCommons. https://repository.upenn.edu/edissertations/589 For more information, please contact [email protected]. Dynamics of Disintegration: The Later Han Empire (25-220CE) & Its Northwestern Frontier Abstract As a frontier region of the Qin-Han (221BCE-220CE) empire, the northwest was a new territory to the Chinese realm. Until the Later Han (25-220CE) times, some portions of the northwestern region had only been part of imperial soil for one hundred years. Its coalescence into the Chinese empire was a product of long-term expansion and conquest, which arguably defined the egionr 's military nature. Furthermore, in the harsh natural environment of the region, only tough people could survive, and unsurprisingly, the region fostered vigorous warriors. Mixed culture and multi-ethnicity featured prominently in this highly militarized frontier society, which contrasted sharply with the imperial center that promoted unified cultural values and stood in the way of a greater degree of transregional integration. As this project shows, it was the northwesterners who went through a process of political peripheralization during the Later Han times played a harbinger role of the disintegration of the empire and eventually led to the breakdown of the early imperial system in Chinese history.