Potential Common Pathogenic Pathways for the Left Ventricular Noncompaction Cardiomyopathy (LVNC)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Extrinsic Regulators of Mrna Translation in Developing Brain: Story of Wnts
cells Article Extrinsic Regulators of mRNA Translation in Developing Brain: Story of WNTs Yongkyu Park * , Midori Lofton , Diana Li and Mladen-Roko Rasin * Department of Neuroscience and Cell Biology, Robert Wood Johnson Medical School, Rutgers University, Piscataway, NJ 08854, USA; [email protected] (M.L.); [email protected] (D.L.) * Correspondence: [email protected] (Y.P.); [email protected] (M.-R.R.) Abstract: Extrinsic molecules such as morphogens can regulate timed mRNA translation events in developing neurons. In particular, Wingless-type MMTV integration site family, member 3 (Wnt3), was shown to regulate the translation of Foxp2 mRNA encoding a Forkhead transcription factor P2 in the neocortex. However, the Wnt receptor that possibly mediates these translation events remains unknown. Here, we report Frizzled member 7 (Fzd7) as the Wnt3 receptor that lays downstream in Wnt3-regulated mRNA translation. Fzd7 proteins co-localize with Wnt3 ligands in developing neo- cortices. In addition, the Fzd7 proteins overlap in layer-specific neuronal subpopulations expressing different transcription factors, Foxp1 and Foxp2. When Fzd7 was silenced, we found decreased Foxp2 protein expression and increased Foxp1 protein expression, respectively. The Fzd7 silencing also dis- rupted the migration of neocortical glutamatergic neurons. In contrast, Fzd7 overexpression reversed the pattern of migratory defects and Foxp protein expression that we found in the Fzd7 silencing. We further discovered that Fzd7 is required for Wnt3-induced Foxp2 mRNA translation. Surprisingly, we also determined that the Fzd7 suppression of Foxp1 protein expression is not Wnt3 dependent. In conclusion, it is exhibited that the interaction between Wnt3 and Fzd7 regulates neuronal identity and the Fzd7 receptor functions as a downstream factor in ligand Wnt3 signaling for mRNA translation. -

(Numbl) Downregulation Increases Tumorigenicity, Cancer Stem Cell-Like Properties and Resistance to Chemotherapy
www.impactjournals.com/oncotarget/ Oncotarget, Vol. 7, No. 39 Research Paper Numb-like (NumbL) downregulation increases tumorigenicity, cancer stem cell-like properties and resistance to chemotherapy José M. García-Heredia1,2, Eva M. Verdugo Sivianes1, Antonio Lucena-Cacace1, Sonia Molina-Pinelo1,3, Amancio Carnero1 1Instituto de Biomedicina de Sevilla (IBIS), Hospital Universitario Virgen del Rocio, Universidad de Sevilla, Consejo Superior de Investigaciones Cientificas, Seville, Spain 2Department of Vegetal Biochemistry and Molecular Biology, University of Seville, Seville, Spain 3Present address: Instituto de Investigación Hospital 12 de Octubre, Madrid, Spain Correspondence to: Amancio Carnero, email: [email protected] Keywords: NumbL, Notch, cancer stem cells, tumor suppressor, tumorigenicity Received: April 22, 2016 Accepted: August 12, 2016 Published: August 23, 2016 ABSTRACT NumbL, or Numb-like, is a close homologue of Numb, and is part of an evolutionary conserved protein family implicated in some important cellular processes. Numb is a protein involved in cell development, in cell adhesion and migration, in asymmetric cell division, and in targeting proteins for endocytosis and ubiquitination. NumbL exhibits some overlapping functions with Numb, but its role in tumorigenesis is not fully known. Here we showed that the downregulation of NumbL alone is sufficient to increase NICD nuclear translocation and induce Notch pathway activation. Furthermore, NumbL downregulation increases epithelial-mesenchymal transition (EMT) and cancer stem cell (CSC)-related gene transcripts and CSC-like phenotypes, including an increase in the CSC-like pool. These data suggest that NumbL can act independently as a tumor suppressor gene. Furthermore, an absence of NumbL induces chemoresistance in tumor cells. An analysis of human tumors indicates that NumbL is downregulated in a variable percentage of human tumors, with lower levels of this gene correlated with worse prognosis in colon, breast and lung tumors. -

Open Data for Differential Network Analysis in Glioma
International Journal of Molecular Sciences Article Open Data for Differential Network Analysis in Glioma , Claire Jean-Quartier * y , Fleur Jeanquartier y and Andreas Holzinger Holzinger Group HCI-KDD, Institute for Medical Informatics, Statistics and Documentation, Medical University Graz, Auenbruggerplatz 2/V, 8036 Graz, Austria; [email protected] (F.J.); [email protected] (A.H.) * Correspondence: [email protected] These authors contributed equally to this work. y Received: 27 October 2019; Accepted: 3 January 2020; Published: 15 January 2020 Abstract: The complexity of cancer diseases demands bioinformatic techniques and translational research based on big data and personalized medicine. Open data enables researchers to accelerate cancer studies, save resources and foster collaboration. Several tools and programming approaches are available for analyzing data, including annotation, clustering, comparison and extrapolation, merging, enrichment, functional association and statistics. We exploit openly available data via cancer gene expression analysis, we apply refinement as well as enrichment analysis via gene ontology and conclude with graph-based visualization of involved protein interaction networks as a basis for signaling. The different databases allowed for the construction of huge networks or specified ones consisting of high-confidence interactions only. Several genes associated to glioma were isolated via a network analysis from top hub nodes as well as from an outlier analysis. The latter approach highlights a mitogen-activated protein kinase next to a member of histondeacetylases and a protein phosphatase as genes uncommonly associated with glioma. Cluster analysis from top hub nodes lists several identified glioma-associated gene products to function within protein complexes, including epidermal growth factors as well as cell cycle proteins or RAS proto-oncogenes. -

A Concise Review of Human Brain Methylome During Aging and Neurodegenerative Diseases
BMB Rep. 2019; 52(10): 577-588 BMB www.bmbreports.org Reports Invited Mini Review A concise review of human brain methylome during aging and neurodegenerative diseases Renuka Prasad G & Eek-hoon Jho* Department of Life Science, University of Seoul, Seoul 02504, Korea DNA methylation at CpG sites is an essential epigenetic mark position of carbon in the cytosine within CG dinucleotides that regulates gene expression during mammalian development with resultant formation of 5mC. The symmetrical CG and diseases. Methylome refers to the entire set of methylation dinucleotides are also called as CpG, due to the presence of modifications present in the whole genome. Over the last phosphodiester bond between cytosine and guanine. The several years, an increasing number of reports on brain DNA human genome contains short lengths of DNA (∼1,000 bp) in methylome reported the association between aberrant which CpG is commonly located (∼1 per 10 bp) in methylation and the abnormalities in the expression of critical unmethylated form and referred as CpG islands; they genes known to have critical roles during aging and neuro- commonly overlap with the transcription start sites (TSSs) of degenerative diseases. Consequently, the role of methylation genes. In human DNA, 5mC is present in approximately 1.5% in understanding neurodegenerative diseases has been under of the whole genome and CpG base pairs are 5-fold enriched focus. This review outlines the current knowledge of the human in CpG islands than other regions of the genome (3, 4). CpG brain DNA methylomes during aging and neurodegenerative islands have the following salient features. In the human diseases. -

View with the Dorsal Side Up
Nieber et al. BMC Developmental Biology 2013, 13:36 http://www.biomedcentral.com/1471-213X/13/36 RESEARCH ARTICLE Open Access NumbL is essential for Xenopus primary neurogenesis Frank Nieber1,2, Marie Hedderich1,2, Olaf Jahn2,3, Tomas Pieler1,2 and Kristine A Henningfeld1,2* Abstract Background: Members of the vertebrate Numb family of cell fate determinants serve multiple functions throughout early embryogenesis, including an essential role in the development of the nervous system. The Numb proteins interact with various partner proteins and correspondingly participate in multiple cellular activities, including inhibition of the Notch pathway. Results: Here, we describe the expression characteristics of Numb and Numblike (NumbL) during Xenopus development and characterize the function of NumbL during primary neurogenesis. NumbL, in contrast to Numb,is expressed in the territories of primary neurogenesis and is positively regulated by the Neurogenin family of proneural transcription factors. Knockdown of NumbL afforded a complete loss of primary neurons and did not lead to an increase in Notch signaling in the open neural plate. Furthermore, we provide evidence that interaction of NumbL with the AP-2 complex is required for NumbL function during primary neurogenesis. Conclusion: We demonstrate an essential role of NumbL during Xenopus primary neurogenesis and provide evidence for a Notch-independent function of NumbL in this context. Keywords: Numb, Notch, Primary neurogenesis, Neurogenin, Neuronal differentiation, Xenopus Background In vertebrates, there are two closely related genes that Numb type proteins define an evolutionary conserved are homologues of Drosophila Numb, namely Numb and class of adaptor proteins that have been implicated in a Numblike (NumbL) [9-11]. -
![NUMBL Mouse Monoclonal Antibody [Clone ID: OTI8D2] Product Data](https://docslib.b-cdn.net/cover/2196/numbl-mouse-monoclonal-antibody-clone-id-oti8d2-product-data-2402196.webp)
NUMBL Mouse Monoclonal Antibody [Clone ID: OTI8D2] Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for TA812202 NUMBL Mouse Monoclonal Antibody [Clone ID: OTI8D2] Product data: Product Type: Primary Antibodies Clone Name: OTI8D2 Applications: WB Recommended Dilution: WB 1:2000 Reactivity: Human, Mouse, Rat Host: Mouse Isotype: IgG1 Clonality: Monoclonal Immunogen: Human recombinant protein fragment corresponding to amino acids 1-225 of human NUMBL (NP_004747) produced in E.coli. Formulation: PBS (PH 7.3) containing 1% BSA, 50% glycerol and 0.02% sodium azide. Concentration: 1 mg/ml Purification: Purified from mouse ascites fluids or tissue culture supernatant by affinity chromatography (protein A/G) Conjugation: Unconjugated Storage: Store at -20°C as received. Stability: Stable for 12 months from date of receipt. Predicted Protein Size: 64.7 kDa Gene Name: NUMB like, endocytic adaptor protein Database Link: NP_004747 Entrez Gene 18223 MouseEntrez Gene 292732 RatEntrez Gene 9253 Human Q9Y6R0 Synonyms: CAG3A; CTG3a; NBL; NUMB-R; NUMBLIKE; NUMBR; TNRC23 Protein Pathways: Notch signaling pathway This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 2 NUMBL Mouse Monoclonal Antibody [Clone ID: OTI8D2] – TA812202 Product images: HEK293T cells were transfected with the pCMV6- ENTRY control (Cat# [PS100001], Left lane) or pCMV6-ENTRY NUMBL (Cat# [RC216869], Right lane) cDNA for 48 hrs and lysed. Equivalent amounts of cell lysates (5 ug per lane) were separated by SDS-PAGE and immunoblotted with anti-NUMBL antibody (Cat# TA812202). -

NUMB and NUMBL Differences in Gene Regulation
www.impactjournals.com/oncotarget/ Oncotarget, 2018, Vol. 9, (No. 10), pp: 9219-9234 Research Paper NUMB and NUMBL differences in gene regulation José Manuel García-Heredia1,2,3 and Amancio Carnero1,3 1Instituto de Biomedicina de Sevilla, IBIS, Hospital Universitario Virgen del Rocío, Universidad de Sevilla, Consejo Superior de Investigaciones Científicas, Seville, Spain 2Department of Vegetal Biochemistry and Molecular Biology, University of Seville, Seville, Spain 3CIBER de Cáncer, Instituto de Salud Carlos III, Pabellón 11, Planta 0, Madrid, Spain Correspondence to: Amancio Carnero, email: [email protected] Keywords: NUMB; NUMBL; cancer; Notch pathway; WNT pathway Received: September 06, 2017 Accepted: January 03, 2018 Published: January 11, 2018 Copyright: García-Heredia et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License 3.0 (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. ABSTRACT NUMB, and its close homologue NUMBL, behave as tumor suppressor genes by regulating the Notch pathway. The downregulation of these genes in tumors is common, allowing aberrant Notch pathway activation and tumor progression. However, some known differences between NUMB and NUMBL have raised unanswered questions regarding the redundancy and/or combined regulation of the Notch pathway by these genes during the tumorigenic process. We have found that NUMB and NUMBL exhibit mutual exclusivity in human tumors, suggesting that the associated tumor suppressor role is regulated by only one of the two proteins in a specific cell, avoiding duplicate signaling and simplifying the regulatory network. We have also found differences in gene expression due to NUMB or NUMBL downregulation. -

Rabbit Anti-NUMBL/FITC Conjugated Antibody
SunLong Biotech Co.,LTD Tel: 0086-571- 56623320 Fax:0086-571- 56623318 E-mail:[email protected] www.sunlongbiotech.com Rabbit Anti-NUMBL/FITC Conjugated antibody SL11974R-FITC Product Name: Anti-NUMBL/FITC Chinese Name: FITC标记的膜相关蛋白样蛋白NUMBL抗体 CAG 3A; CAG3A; CTG 3a; CTG3a; NBL; NUMB Drosophilia Homolog Like; Numb homolog (Drosophila) like; Numb homolog like; Numb like protein; NUMB R; Numb- Alias: like protein; Numb-R; Numb-related protein; NUMBL; NUMBL_HUMAN; NUMBR; TNRC 23; TNRC23. Organism Species: Rabbit Clonality: Polyclonal React Species: Human,Mouse,Rat,Dog,Cow,Horse,Rabbit,Sheep, ICC=1:50-200IF=1:50-200 Applications: not yet tested in other applications. optimal dilutions/concentrations should be determined by the end user. Molecular weight: 65kDa Form: Lyophilized or Liquid Concentration: 1mg/ml immunogen: KLH conjugated synthetic peptide derived from human NUMBL (75-120aa) Lsotype: IgG Purification: affinitywww.sunlongbiotech.com purified by Protein A Storage Buffer: 0.01M TBS(pH7.4) with 1% BSA, 0.03% Proclin300 and 50% Glycerol. Store at -20 °C for one year. Avoid repeated freeze/thaw cycles. The lyophilized antibody is stable at room temperature for at least one month and for greater than a year Storage: when kept at -20°C. When reconstituted in sterile pH 7.4 0.01M PBS or diluent of antibody the antibody is stable for at least two weeks at 2-4 °C. background: In Drosophila, neuronal cell fate decisions are directed by NUMB, a signaling adapter protein with two protein-protein interaction domains, namely a phosphotyrosine-binding Product Detail: domain and a proline-rich SH3-binding region (PRR). -

Numbl CRISPR/Cas9 KO Plasmid (H): Sc-408169
SANTA CRUZ BIOTECHNOLOGY, INC. NumbL CRISPR/Cas9 KO Plasmid (h): sc-408169 BACKGROUND APPLICATIONS The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and NumbL CRISPR/Cas9 KO Plasmid (h) is recommended for the disruption of CRISPR-associated protein (Cas9) system is an adaptive immune response gene expression in human cells. defense mechanism used by archea and bacteria for the degradation of foreign genetic material (4,6). This mechanism can be repurposed for other 20 nt non-coding RNA sequence: guides Cas9 functions, including genomic engineering for mammalian systems, such as to a specific target location in the genomic DNA gene knockout (KO) (1,2,3,5). CRISPR/Cas9 KO Plasmid products enable the U6 promoter: drives gRNA scaffold: helps Cas9 identification and cleavage of specific genes by utilizing guide RNA (gRNA) expression of gRNA bind to target DNA sequences derived from the Genome-scale CRISPR Knock-Out (GeCKO) v2 library developed in the Zhang Laboratory at the Broad Institute (3,5). Termination signal Green Fluorescent Protein: to visually REFERENCES verify transfection CRISPR/Cas9 Knockout Plasmid CBh (chicken β-Actin 1. Cong, L., et al. 2013. Multiplex genome engineering using CRISPR/Cas hybrid) promoter: drives expression of Cas9 systems. Science 339: 819-823. 2A peptide: allows production of both Cas9 and GFP from the 2. Mali, P., et al. 2013. RNA-guided human genome engineering via Cas9. same CBh promoter Science 339: 823-826. Nuclear localization signal 3. Ran, F.A., et al. 2013. Genome engineering using the CRISPR-Cas9 system. Nuclear localization signal SpCas9 ribonuclease Nat. Protoc. 8: 2281-2308. -
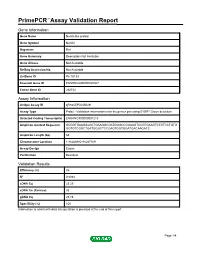
Primepcr™Assay Validation Report
PrimePCR™Assay Validation Report Gene Information Gene Name Numb-like protein Gene Symbol Numbl Organism Rat Gene Summary Description Not Available Gene Aliases Not Available RefSeq Accession No. Not Available UniGene ID Rn.15133 Ensembl Gene ID ENSRNOG00000020867 Entrez Gene ID 292732 Assay Information Unique Assay ID qRnoCEP0045029 Assay Type Probe - Validation information is for the primer pair using SYBR® Green detection Detected Coding Transcript(s) ENSRNOT00000057213 Amplicon Context Sequence GCGGTGAAGAAGCTGAAGGCGATGGGCCGGAAGTCCGTGAAGTCTGTCCTGTG GGTGTCGGCTGATGGGCTCCGAGTGGTGGATGACAAGACC Amplicon Length (bp) 63 Chromosome Location 1:85286982-85287169 Assay Design Exonic Purification Desalted Validation Results Efficiency (%) 89 R2 0.9984 cDNA Cq 23.25 cDNA Tm (Celsius) 83 gDNA Cq 26.16 Specificity (%) 100 Information to assist with data interpretation is provided at the end of this report. Page 1/4 PrimePCR™Assay Validation Report Numbl, Rat Amplification Plot Amplification of cDNA generated from 25 ng of universal reference RNA Melt Peak Melt curve analysis of above amplification Standard Curve Standard curve generated using 20 million copies of template diluted 10-fold to 20 copies Page 2/4 PrimePCR™Assay Validation Report Products used to generate validation data Real-Time PCR Instrument CFX384 Real-Time PCR Detection System Reverse Transcription Reagent iScript™ Advanced cDNA Synthesis Kit for RT-qPCR Real-Time PCR Supermix SsoAdvanced™ SYBR® Green Supermix Experimental Sample qPCR Reference Total RNA Data Interpretation Unique Assay ID This is a unique identifier that can be used to identify the assay in the literature and online. Detected Coding Transcript(s) This is a list of the Ensembl transcript ID(s) that this assay will detect. Details for each transcript can be found on the Ensembl website at www.ensembl.org. -

A Concise Review of Human Brain Methylome During Aging and Neurodegenerative Diseases
BMB Rep. 2019; 52(10): 577-588 BMB www.bmbreports.org Reports Invited Mini Review A concise review of human brain methylome during aging and neurodegenerative diseases Renuka Prasad G & Eek-hoon Jho* Department of Life Science, University of Seoul, Seoul 02504, Korea DNA methylation at CpG sites is an essential epigenetic mark position of carbon in the cytosine within CG dinucleotides that regulates gene expression during mammalian development with resultant formation of 5mC. The symmetrical CG and diseases. Methylome refers to the entire set of methylation dinucleotides are also called as CpG, due to the presence of modifications present in the whole genome. Over the last phosphodiester bond between cytosine and guanine. The several years, an increasing number of reports on brain DNA human genome contains short lengths of DNA (∼1,000 bp) in methylome reported the association between aberrant which CpG is commonly located (∼1 per 10 bp) in methylation and the abnormalities in the expression of critical unmethylated form and referred as CpG islands; they genes known to have critical roles during aging and neuro- commonly overlap with the transcription start sites (TSSs) of degenerative diseases. Consequently, the role of methylation genes. In human DNA, 5mC is present in approximately 1.5% in understanding neurodegenerative diseases has been under of the whole genome and CpG base pairs are 5-fold enriched focus. This review outlines the current knowledge of the human in CpG islands than other regions of the genome (3, 4). CpG brain DNA methylomes during aging and neurodegenerative islands have the following salient features. In the human diseases. -

COPD GWAS Variant at 19Q13.2 in Relation with DNA Methylation And
Human Molecular Genetics, 2018, Vol. 27, No. 2 396–405 doi: 10.1093/hmg/ddx390 Advance Access Publication Date: 28 October 2017 Association Studies Article ASSOCIATION STUDIES ARTICLE COPD GWAS variant at 19q13.2 in relation with DNA methylation and gene expression Ivana Nedeljkovic1, Lies Lahousse1,2,3, Elena Carnero-Montoro1,4, Alen Faiz5, Judith M. Vonk5,6, Kim de Jong5,6, Diana A. van der Plaat5,6, Cleo C. van Diemen7, Maarten van den Berge5,8, Ma’en Obeidat9, Yohan Bosse´ 10, David C. Nickle11, BIOS Consortium†, Andre G. Uitterlinden1,12, Joyce B.J. van Meurs12, Bruno H.C. Stricker1, Guy G. Brusselle1,3,13, Dirkje S. Postma5,8, H. Marike Boezen5,6, Cornelia M. van Duijn1 and Najaf Amin1,* 1Department of Epidemiology, Erasmus Medical Center, Rotterdam, The Netherlands, 2Department of Bioanalysis, Pharmaceutical Care Unit, 3Department of Respiratory Medicine, Ghent University Hospital, Ghent, Belgium, 4GENYO Center for Genomics and Oncological Research, Pfizer/University of Granada/Andalusian Region Government, Granada, Spain, 5University of Groningen, Groningen Research Institute for Asthma and COPD (GRIAC), Groningen, The Netherlands, 6Department of Epidemiology, 7Department of Genetics, 8Department of Pulmonology, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands, 9Center for Heart Lung Innovation, University of British Columbia, Vancouver, BC, Canada, 10Department of Molecular Medicine, Institut Universitaire de Cardiologie et de Pneumologie de Que´bec, Universite´ Laval, Quebec, QC, Canada, 11Merck Research Laboratories, Genetics and Pharmacogenomics (GpGx), Seattle, WA, USA, 12Department of Internal Medicine and 13Department of Respiratory Medicine, Erasmus Medical Center, Rotterdam, The Netherlands *To whom correspondence should be addressed at: Department of Epidemiology, Erasmus MC, PO Box 2040, 3000 CA Rotterdam, The Netherlands.