Dead Bugs Don't Mutate: Susceptibility Issues in the Emergence of Bacterial Resistance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinically Isolated Chlamydia Trachomatis Strains
ANTIMICROBIAL AGENTS AND CHEMOTHERAPY, JUIY 1988, p. 1080-1081 Vol. 32, No. 7 0066-4804/88/071080-02$02.00/0 Copyright © 1988, American Society for Microbiology In Vitro Activities of T-3262, NY-198, Fleroxacin (AM-833; RO 23-6240), and Other New Quinolone Agents against Clinically Isolated Chlamydia trachomatis Strains HIROSHI MAEDA,* AKIRA FUJII, KATSUHISA NAKATA, SOICHI ARAKAWA, AND SADAO KAMIDONO Department of Urology, School of Medicine, Kobe University, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe-city, Japan Received 9 December 1987/Accepted 29 March 1988 The in vitro activities of three newly developed quinolone drugs (T-3262, NY-198, and fleroxacin [AM-833; RO 23-6240]) against 10 strains of clinically isolated Chiamydia trachomatis were assessed and compared with those of other quinolones and minocycline. T-3262 (MIC for 90% of isolates tested, 0.1 ,ug/ml) was the most active of the quinolones. The NY-198 and fleroxacin MICs for 90% of isolates were 3.13 and 62.5 ,ug/ml, respectively. Recently, it has become well known that Chlamydia 1-ml sample of suspension was seeded into flat-bottomed trachomatis is an important human pathogen. It is respon- tubes with glass cover slips and incubated at 37°C in 5% CO2 sible not only for trachoma but also for sexually transmitted for 24 h. The monolayer was inoculated with 103 inclusion- infections, including lymphogranuloma venereum. In forming units of C. trachomatis. The tubes were centrifuged women, it causes cervicitis, endometritis, and salpingitis at 2,000 x g at 25°C for 45 min and left undisturbed at room asymptomatically (19), while in men it causes nongono- temperature for 2 h. -

Gatifloxacin for Treating Enteric Fever Submission to the 18Th Expert
Gatifloxacin for enteric fever Gatifloxacin for treating enteric fever Submission to the 18th Expert Committee on the Selection and Use of Essential Medicines 1 Gatifloxacin for enteric fever Table of contents Gatifloxacin for treating enteric fever....................................................................................... 1 Submission to the 18th Expert Committee on the Selection and Use of Essential Medicines . 1 1 Summary statement of the proposal for inclusion........................................................... 4 1.1 Rationale for this submission................................................................................... 4 2 Focal point in WHO submitting the application ............................................................... 4 3 Organizations consulted and supporting the application ................................................ 5 4 International Nonproprietary Name (INN, generic name) of the medicine..................... 5 5 Formulation proposed for inclusion ................................................................................. 5 5.1 Prospective formulation improvements.................................................................. 6 6 International availability................................................................................................... 6 6.1 Patent status ............................................................................................................ 6 6.2 Production............................................................................................................... -

WHO Report on Surveillance of Antibiotic Consumption: 2016-2018 Early Implementation ISBN 978-92-4-151488-0 © World Health Organization 2018 Some Rights Reserved
WHO Report on Surveillance of Antibiotic Consumption 2016-2018 Early implementation WHO Report on Surveillance of Antibiotic Consumption 2016 - 2018 Early implementation WHO report on surveillance of antibiotic consumption: 2016-2018 early implementation ISBN 978-92-4-151488-0 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons. org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non- commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. WHO report on surveillance of antibiotic consumption: 2016-2018 early implementation. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Ciprofloxacin, Enoxacin, and Ofloxacin Against Aerobic and Anaerobic Bacteria Isolated from Bite Wounds ELLIE J
ANTIMICROBIAL AGENTS AND CHEMOTHERAPY, Aug. 1988, p. 1143-1148 Vol. 32, No. 8 0066-4804/88/081143-06$02.00/0 Copyright © 1988, American Society for Microbiology Comparative Activities of Cefuroxime, Amoxicillin-Clavulanic Acid, Ciprofloxacin, Enoxacin, and Ofloxacin against Aerobic and Anaerobic Bacteria Isolated from Bite Wounds ELLIE J. C. GOLDSTEIN* AND DIANE M. CITRON R. M. Alden Research Laboratory, Santa Monica Hospital Medical Center, Santa Monica, California 90404 Received 29 March 1988/Accepted 21 May 1988 We studied the comparative in vitro activities of 10 oral antimicrobial agents against 147 aerobic and 61 anaerobic bacteria making up species in 13 genera (Staphylococcus aureus, streptococci, Eikenella corrodens, Pasteurella multocida, Haemophilus-Actinobacillus spp., M-5, EF-4, Moraxella spp., Flavobacterium Ilb, Bacteroides melaninogenicus, Bacteroides spp., Fusobacterium spp., and Peptostreptococcus spp.) that were isolated from bite wounds. Cefuroxime was generally >fourfold more active than cephalexin and cefadroxil against all aerobic isolates, including Pasteurella multocida. The fluoroquinolones were highly active against most aerobic isolates but were less active against anaerobic isolates. Ciprofloxacin was generally more active than either enoxacin or ofloxacin. Discrepancies of >30% in the interpretation of susceptibilities between break points suggested by the National Committee for Clinical Laboratory Standards and those related to oral dose peak levels (one-half to one-quarter of maximum achievable concentrations) were noted in 14% (18 of 130) of the instances. The choice of an appropriate antimicrobial regimen for wound isolates to these new antimicrobial agents and com- infections caused by animal and human bites poses a di- pared their activities with the activities of the older antimi- lemma for clinicians. -

The Grohe Method and Quinolone Antibiotics
The Grohe method and quinolone antibiotics Antibiotics are medicines that are used to treat bacterial for modern fluoroquinolones. The Grohe process and the infections. They contain active ingredients belonging to var- synthesis of ciprofloxacin sparked Bayer AG’s extensive ious substance classes, with modern fluoroquinolones one research on fluoroquinolones and the global competition of the most important and an indispensable part of both that produced additional potent antibiotics. human and veterinary medicine. It is largely thanks to Klaus Grohe – the “father of Bayer quinolones” – that this entirely In chemical terms, the antibiotics referred to for simplicity synthetic class of antibiotics now plays such a vital role for as quinolones are derived from 1,4-dihydro-4-oxo-3-quin- medical practitioners. From 1965 to 1997, Grohe worked oline carboxylic acid (1) substituted in position 1. as a chemist, carrying out basic research at Bayer AG’s Fluoroquinolones possess a fluorine atom in position 6. In main research laboratory (WHL) in Leverkusen. During this addition, ciprofloxacin (2) has a cyclopropyl group in posi- period, in 1975, he developed the Grohe process – a new tion 1 and also a piperazine group in position 7 (Figure A). multi-stage synthesis method for quinolones. It was this This substituent pattern plays a key role in its excellent achievement that first enabled him to synthesize active an- antibacterial efficacy. tibacterial substances such as ciprofloxacin – the prototype O 5 O 4 3 6 COOH F COOH 7 2 N N N 8 1 H N R (1) (2) Figure A: Basic structure of quinolone (1) (R = various substituents) and ciprofloxacin (2) Quinolones owe their antibacterial efficacy to their inhibition This unique mode of action also makes fluoroquinolones of essential bacterial enzymes – DNA gyrase (topoisomer- highly effective against a large number of pathogenic ase II) and topoisomerase IV. -

Surveillance of Antimicrobial Consumption in Europe 2013-2014 SURVEILLANCE REPORT
SURVEILLANCE REPORT SURVEILLANCE REPORT Surveillance of antimicrobial consumption in Europe in Europe consumption of antimicrobial Surveillance Surveillance of antimicrobial consumption in Europe 2013-2014 2012 www.ecdc.europa.eu ECDC SURVEILLANCE REPORT Surveillance of antimicrobial consumption in Europe 2013–2014 This report of the European Centre for Disease Prevention and Control (ECDC) was coordinated by Klaus Weist. Contributing authors Klaus Weist, Arno Muller, Ana Hoxha, Vera Vlahović-Palčevski, Christelle Elias, Dominique Monnet and Ole Heuer. Data analysis: Klaus Weist, Arno Muller and Ana Hoxha. Acknowledgements The authors would like to thank the ESAC-Net Disease Network Coordination Committee members (Marcel Bruch, Philippe Cavalié, Herman Goossens, Jenny Hellman, Susan Hopkins, Stephanie Natsch, Anna Olczak-Pienkowska, Ajay Oza, Arjana Tambić Andrasevic, Peter Zarb) and observers (Jane Robertson, Arno Muller, Mike Sharland, Theo Verheij) for providing valuable comments and scientific advice during the production of the report. All ESAC-Net participants and National Coordinators are acknowledged for providing data and valuable comments on this report. The authors also acknowledge Gaetan Guyodo, Catalin Albu and Anna Renau-Rosell for managing the data and providing technical support to the participating countries. Suggested citation: European Centre for Disease Prevention and Control. Surveillance of antimicrobial consumption in Europe, 2013‒2014. Stockholm: ECDC; 2018. Stockholm, May 2018 ISBN 978-92-9498-187-5 ISSN 2315-0955 -

Customs Tariff - Schedule
CUSTOMS TARIFF - SCHEDULE 99 - i Chapter 99 SPECIAL CLASSIFICATION PROVISIONS - COMMERCIAL Notes. 1. The provisions of this Chapter are not subject to the rule of specificity in General Interpretative Rule 3 (a). 2. Goods which may be classified under the provisions of Chapter 99, if also eligible for classification under the provisions of Chapter 98, shall be classified in Chapter 98. 3. Goods may be classified under a tariff item in this Chapter and be entitled to the Most-Favoured-Nation Tariff or a preferential tariff rate of customs duty under this Chapter that applies to those goods according to the tariff treatment applicable to their country of origin only after classification under a tariff item in Chapters 1 to 97 has been determined and the conditions of any Chapter 99 provision and any applicable regulations or orders in relation thereto have been met. 4. The words and expressions used in this Chapter have the same meaning as in Chapters 1 to 97. Issued January 1, 2019 99 - 1 CUSTOMS TARIFF - SCHEDULE Tariff Unit of MFN Applicable SS Description of Goods Item Meas. Tariff Preferential Tariffs 9901.00.00 Articles and materials for use in the manufacture or repair of the Free CCCT, LDCT, GPT, UST, following to be employed in commercial fishing or the commercial MT, MUST, CIAT, CT, harvesting of marine plants: CRT, IT, NT, SLT, PT, COLT, JT, PAT, HNT, Artificial bait; KRT, CEUT, UAT, CPTPT: Free Carapace measures; Cordage, fishing lines (including marlines), rope and twine, of a circumference not exceeding 38 mm; Devices for keeping nets open; Fish hooks; Fishing nets and netting; Jiggers; Line floats; Lobster traps; Lures; Marker buoys of any material excluding wood; Net floats; Scallop drag nets; Spat collectors and collector holders; Swivels. -

European Surveillance of Healthcare-Associated Infections in Intensive Care Units
TECHNICAL DOCUMENT European surveillance of healthcare-associated infections in intensive care units HAI-Net ICU protocol Protocol version 1.02 www.ecdc.europa.eu ECDC TECHNICAL DOCUMENT European surveillance of healthcare- associated infections in intensive care units HAI-Net ICU protocol, version 1.02 This technical document of the European Centre for Disease Prevention and Control (ECDC) was coordinated by Carl Suetens. In accordance with the Staff Regulations for Officials and Conditions of Employment of Other Servants of the European Union and the ECDC Independence Policy, ECDC staff members shall not, in the performance of their duties, deal with a matter in which, directly or indirectly, they have any personal interest such as to impair their independence. This is version 1.02 of the HAI-Net ICU protocol. Differences between versions 1.01 (December 2010) and 1.02 are purely editorial. Suggested citation: European Centre for Disease Prevention and Control. European surveillance of healthcare- associated infections in intensive care units – HAI-Net ICU protocol, version 1.02. Stockholm: ECDC; 2015. Stockholm, March 2015 ISBN 978-92-9193-627-4 doi 10.2900/371526 Catalogue number TQ-04-15-186-EN-N © European Centre for Disease Prevention and Control, 2015 Reproduction is authorised, provided the source is acknowledged. TECHNICAL DOCUMENT HAI-Net ICU protocol, version 1.02 Table of contents Abbreviations ............................................................................................................................................... -

A Review on Antibiotic Resistance and Way of Combating Antimicrobial Resistance
A review on antibiotic resistance and way of combating antimicrobial resistance Shifa Begum1, Tofa Begum2, Naziza Rahman 3 and Ruhul A. Khan4, * 1Department of Genetic Engineering and Biotechnology, University of Chittagong, Chittagong, Bangladesh. 2Research Laboratories in Sciences Applied to Food, Canadian Irradiation Center, INRS-Institut Armand-Frappier, 531, Boulevard des Prairies, Laval, Quebec, Canada, H7V 1B7. 3Department of Microbiology, University of Dhaka, Bangladesh. 4Institute of Radiation and Polymer Technology, Atomic Energy Research Establishment, Savar, Dhaka, Bangladesh. GSC Biological and Pharmaceutical Sciences, 2021, 14(02), 087–097 Publication history: Received on 13 January 2021; revised on 07 February 2021; accepted on 09 February 2021 Article DOI: https://doi.org/10.30574/gscbps.2021.14.2.0037 Abstract Antibiotics are widely used most effective medication since the twentieth century against bacterial infections (Tetanus, Strep Throat, Urinary Tract Infections, etc.) and thus save one’s life. Before 20th-century infectious disease played the main role in the death. Thus, antibiotics opened a revolutionary era in the field of medication. These cannot fight against viral infections. Antibiotics are also known as an antibacterial that kill or slow down bacterial growth and prohibit the bacteria to harm. Resistance comes as a curse with antibiotics that occurs when bacteria change in some way that reduces or eliminates the effectiveness of drugs, chemicals or other agents designed to cure or prevent infections. It is now a significant threat to public health that is affecting humans worldwide outside the environment of the hospital. When a bacterium once become resistant to antibiotic then the bacterial infections cannot be cured with that antibiotic. -

Pharmacology-2/ Dr
1 Pharmacology-2/ Dr. Y. Abusamra Pharmacology-2 Quinolones, trimethoprim & sulfonamides Dr. Yousef Abdel - Kareem Abusamra Faculty of Pharmacy Philadelphia University 2 3 LEARNING OUTCOMES After completing studying this chapter, the student should be able to: Classify the drugs into subgroups such as quinolones and sulfonamides. Recognize the bacterial spectrum of all these antibiotic and antibacterial groups. Summarize the most remarkable pharmacokinetic features of these drugs. Numerate the most important side effects associated with these agents. Select the antibiotic of choice to be used in certain infections, as associated with the patient status including comorbidity, the species of bacteria causing the infection and concurrently prescribed drugs. Reason some remarkable clinical considerations related to the use or contraindication or precaution of a certain drug. Illustrate the mechanism of action of each of these drugs. • Following synthesis of na lidixic a c id in the early 1960s, continued modification of the quinolone nucleus expanded the spectrum of activity, improved pharmacokinetics, and stabilized compounds against common mechanisms of resistance. • Overuse resulted in rising rates of resistance in gram-negative and gram-positive organisms, increased frequency of Clostridium difficile infections, and identification of numerous tough adverse effects. • Consequently, these agents have been relegated to second-line options for various indications. 4 Pharmacology-2/ Dr. Y. Abusamra Only will be mentioned here 5 Pharmacology-2/ Dr. Y. Abusamra Most bacterial species maintain two distinct type II topoisomerases that assist with deoxyribonucleic acid Topoisomerases: Supercoiling Unwinding (DNA) replication: . DNA gyrase {supercoiling} and . Topoisomerase IV {Unwinding}. Following cell wall entry through porin channels, fluoroquinolones bind to these enzymes and interfere with DNA ligation. -

Wo 2008/127291 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (43) International Publication Date PCT (10) International Publication Number 23 October 2008 (23.10.2008) WO 2008/127291 A2 (51) International Patent Classification: Jeffrey, J. [US/US]; 106 Glenview Drive, Los Alamos, GOlN 33/53 (2006.01) GOlN 33/68 (2006.01) NM 87544 (US). HARRIS, Michael, N. [US/US]; 295 GOlN 21/76 (2006.01) GOlN 23/223 (2006.01) Kilby Avenue, Los Alamos, NM 87544 (US). BURRELL, Anthony, K. [NZ/US]; 2431 Canyon Glen, Los Alamos, (21) International Application Number: NM 87544 (US). PCT/US2007/021888 (74) Agents: COTTRELL, Bruce, H. et al.; Los Alamos (22) International Filing Date: 10 October 2007 (10.10.2007) National Laboratory, LGTP, MS A187, Los Alamos, NM 87545 (US). (25) Filing Language: English (81) Designated States (unless otherwise indicated, for every (26) Publication Language: English kind of national protection available): AE, AG, AL, AM, AT,AU, AZ, BA, BB, BG, BH, BR, BW, BY,BZ, CA, CH, (30) Priority Data: CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, 60/850,594 10 October 2006 (10.10.2006) US ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, KZ, LA, LC, LK, (71) Applicants (for all designated States except US): LOS LR, LS, LT, LU, LY,MA, MD, ME, MG, MK, MN, MW, ALAMOS NATIONAL SECURITY,LLC [US/US]; Los MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PG, PH, PL, Alamos National Laboratory, Lc/ip, Ms A187, Los Alamos, PT, RO, RS, RU, SC, SD, SE, SG, SK, SL, SM, SV, SY, NM 87545 (US). -
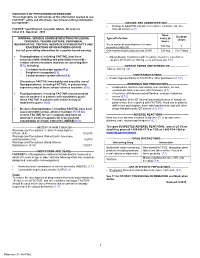
FACTIVE® Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use FACTIVE® safely and effectively. See full prescribing information for FACTIVE®. --------------------- DOSAGE AND ADMINISTRATION --------------------- • Dosage in Adult Patients with a Creatinine Clearance Greater FACTIVE® (gemifloxacin mesylate) tablets, for oral use than 40 mL/min (2.1) Initial U.S. Approval: 2003 Dose Duration WARNING: SERIOUS ADVERSE REACTIONS INCLUDING Type of Infection every 24 (days) TENDINITIS, TENDON RUPTURE, PERIPHERAL hours NEUROPHATHY, CENTRAL NERVOUS SYSTEM EFFECTS AND Acute bacterial exacerbation of chronic 320 mg 5 EXACERBATIONS OF MYASTHENIS GRAVIS bronchitis (ABECB) See full prescribing information for complete boxed warning. Community-acquired pneumonia (CAP) 320 mg 5 to 7 days • Fluoroquinolones, including FACTIVE, have been • Adjust dosage for patients with creatinine clearance less than or associated with disabling and potentially irreversible equal to 40 mL/min to 160 mg every 24 hours.(22, 8.8) serious adverse reactions that have occurred together (5.1), including: ---------------------DOSAGE FORMS AND STRENGTHS--------------------- Tablets: 320 mg (3) o Tendinitis and tendon rupture(5.2) o Peripheral neuropathy(5.3) Central nervous system effects(5.4) -------------------------------CONTRAINDICATIONS----------------------------- o • Known hypersensitivity to FACTIVE or other quinolones (4, 5.7) Discontinue FACTIVE immediately and avoid the use of fluoroquinolones, including FACTIVE, in patients