Hamstring Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Cov2 MNB SO 11.Indd
essential skills BY BEN E. BENJAMIN 94 massage & bodywork september/october 2011 082-105 SO MNB 11.indd 94 7/29/11 1:33 PM PULLED HAMSTRING, PART 1 Pulled hamstring is a term often used to describe pain in the back of the thigh, but the hamstring can also be “pulled” in the lower buttock, behind the knee, or near the front of the knee—either medially or laterally. What this indicates is that some fibers—belonging to either a hamstring muscle or tendon—are strained. The (a) Semimembranosis pain can be felt anywhere along the three important muscle tendon units. (b) Semitendinosis There are three hamstrings: a) the (c) Biceps Femoris semimembranosis on the medial side, b) the semitendinosis in the middle, and c) the biceps femoris on the lateral aspect (Image 1). All of the hamstrings begin at a common tendon at the ischial tuberosity at the base of the pelvis. This is the part of the pelvis that makes contact with the chair when seated. Sobotta: Atlas der Anatomie des These muscles in the posterior thigh Menschen @Elsevier GmbH, Urban & are among the longest in the body Fischer Verlag Munich. and span two joints: the hip and the knee. They extend the hip and flex the knee to help you walk, run, jump, and climb stairs. The semimembranosis and the semitendinosis control the HOW AND WhY IT HAPPENS If a client has pain in the posterior medial half of the posterior thigh and Suddenly it appears—pain in the back thigh when using the hamstring attach just below the anterior medial of the thigh. -
Hamstring Muscle Injuries
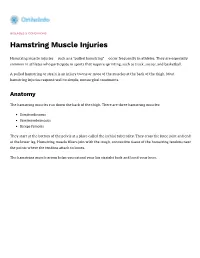
DISEASES & CONDITIONS Hamstring Muscle Injuries Hamstring muscle injuries — such as a "pulled hamstring" — occur frequently in athletes. They are especially common in athletes who participate in sports that require sprinting, such as track, soccer, and basketball. A pulled hamstring or strain is an injury to one or more of the muscles at the back of the thigh. Most hamstring injuries respond well to simple, nonsurgical treatments. Anatomy The hamstring muscles run down the back of the thigh. There are three hamstring muscles: Semitendinosus Semimembranosus Biceps femoris They start at the bottom of the pelvis at a place called the ischial tuberosity. They cross the knee joint and end at the lower leg. Hamstring muscle fibers join with the tough, connective tissue of the hamstring tendons near the points where the tendons attach to bones. The hamstring muscle group helps you extend your leg straight back and bend your knee. Normal hamstring anatomy. The three hamstring muscles start at the bottom of the pelvis and end near the top of the lower leg. Description A hamstring strain can be a pull, a partial tear, or a complete tear. Muscle strains are graded according to their severity. A grade 1 strain is mild and usually heals readily; a grade 3 strain is a complete tear of the muscle that may take months to heal. Most hamstring injuries occur in the thick, central part of the muscle or where the muscle fibers join tendon fibers. In the most severe hamstring injuries, the tendon tears completely away from the bone. It may even pull a piece of bone away with it. -

Your Chiropractor May/June 2021
FREE YOUR CHIROPRACTOR ! JULY/AUGUST 2021 This month we discuss... THREE CHIROPRACTIC LOCATIONS TAKING CARE OF BACK ACHE FROM MANAGE STRESS - GETTING YOUR DOSE YOUR HAMSTRINGS WALKING & STANDING BOOST YOUR HEALTH OF VITAMIN D 19 Ocean Drive, Port Macquarie 42 Cameron St, Wauchope 89 Bold Street, Laurieton Frozen shoulders can thaw P: 02 6583 9393 F: 02 6583 9389 Is your shoulder painful, and are you develop after a fall or injury, or if you’re experiencing stiffness and disability which unable to move your arm, such as being in E: [email protected] has worsened over time? Have you been a sling or following stroke or mastectomy. W: www.coastlinechiropractic.com.au diagnosed with a frozen shoulder? Not using it may be a greater problem than overuse. This makes healthy use — and NEW SERVICE AND EXTENDED TIMES Frozen shoulder, also known as adhesive a healthy life — important for possible capsulitis, is common. It tends to strike OPEN NOW − 89 Bold Street Laurieton prevention and recovery. between the ages of 40–60 years, more so We welcome Dr Brett Clacher to our team in women and people with certain underlying WHAT SHOULD I DO ABOUT IT? illness. And it can hurt! While sharp pain is If you have been diagnosed with frozen OUR CHIROPRACTORS experienced with extremes of motion, the shoulder, it's important to understand Dr Darren J Gray usual pain is described as dull and aching. its natural progression; how long it will Chiropractor, Certified Rehab Therapist WHAT IS FROZEN SHOULDER AND take to recuperate. Recovery can take BSc, MChiro, MClinRehabNeuro (MCAA, ClinFellAAFN) HOW DOES IT PROGRESS? several years, so a tailored treatment plan is essential. -

The Art and Science of Kinesiology Taping 17
CONTENTS 3 3 Super Supplements for Massage Therapists 5 Immunity-Boosting Essential Oils 6 Mini-Meals on the Run 5 Secrets of Better Body Mechanics 5 8 10 Master the Art of Slowing Down 13 6 Ways to Roll Away Pain & Tightness 17 The Art and Science of Kinesiology Taping 22 Hot and Cold Stones for Back and Neck 13 Self-Care 23 Journal to Enhance Intuition and Retrain Your Inner Critic 17 25 Top 10 Tips for Career Longevity 27 Everyone has a story. This is ours 2 SUPER SUPPLEMENTS FOR MASSAGE THERAPISTS by Stacey Littlefield ietary supplements can nourish and Dprotect you, helping your mind and body adjust to the repeated, daily stresses ASHWAGANDHA (Withania somnifera) of your work as a massage therapist. has roots in ayurvedic medicine, where RHODIOLA ROSEA, also known as it is used to prolong life, stimulate the golden root, has been used as a traditional mind and enhance vigor. Ashwagandha is medicine for centuries. In Russia, calming, effective at addressing anxiety, Scandinavia and Asian countries, its roots stress-induced sleep problems and have been used to increase physical fatigue. The authors of review studies on endurance, work capacity and productivity, ashwagandha published in 2014 in the and to treat fatigue and depression. Journal of Alternative and Complementary Rhodiola rosea also increases mental Medicine wrote, “All five studies concluded performance, especially concentration, and that [withania somnifera] intervention prevents stress-induced burnout, a claim resulted in greater score improvements supported by research including “Rhodiola (significantly in most cases) than placebo rosea for mental and physical fatigue in in outcomes on anxiety or stress scales.” nursing students: a randomized controlled trial,” published by PLOS ONE in 2014. -

Platelet-Rich Plasma (PRP) - Orthoinfo - AAOS
9/18/2020 Platelet-Rich Plasma (PRP) - OrthoInfo - AAOS Ballard Office 5350 Tallman Ave NW, Suite 500 Seattle, WA 98107 www.seattlehandandelbow.com Wallingford Office 2409 45th Street, Seattle, WA 98103 TREATMENT Platelet-Rich Plasma (PRP) During the past several years, much has been written about a preparation called platelet-rich plasma (PRP) and its potential effectiveness in the treatment of injuries. Many famous athletes — Tiger Woods, tennis star Rafael Nadal, and several others — have received PRP for various problems, such as sprained knees and chronic tendon injuries. These types of conditions have typically been treated with medications, physical therapy, or even surgery. Some athletes have credited PRP with their being able to return more quickly to competition. Even though PRP has received extensive publicity, there are still lingering questions about it, such as: What exactly is platelet-rich plasma? How does it work? What conditions are being treated with PRP? Is PRP treatment effective? What Is Platelet-rich Plasma (PRP)? Although blood is mainly a liquid (called plasma), it also contains small solid components (red cells, white cells, and platelets.) The platelets are best known for their importance in clotting blood. However, platelets also contain hundreds of proteins called growth factors which are very important in the healing of injuries. PRP is plasma with many more platelets than what is typically found in blood. The concentration of platelets — and, thereby, the concentration of growth factors — can be 5 to 10 times greater (or richer) than usual. To develop a PRP preparation, blood must first be drawn from a patient. -

Regenerative Medicine Educational Brochure
REGENERATIVE MEDICINE Tapping into the body’s ability to heal itself Ryan Woods, MD Dr. Ryan Woods is a non-operative sports medicine physician. He earned his medical degree at the Michigan State University College of Human Medicine in East Lansing, Michigan. He completed his residency in physical medicine and rehabilitation at the Mayo Clinic and a fellowship in physical medicine and rehabilitation sports medicine at the Mayo Clinic School of Graduate Medical Education, both in Rochester, Minnesota. He is board certified by the American Board of Physical Medicine and Rehabilitation in physical medicine and rehabilitation, and in sports medicine. baycare.net/ortho 920-288-5555 • 877-884-8796 baycare.net/ortho 920-288-5555 • 877-884-8796 WHAT IS REGENERATIVE MEDICINE? What is PRP? Platelet-rich plasma, or PRP, is made from the patient’s blood, which is processed to isolate Regenerative medicine taps into the body’s ability plasma and platelets. Plasma is rich in platelets, to heal itself. and platelets are rich in proteins that help The two primary regenerative medicine heal the body and control inflammation. PRP treatments are platelet-rich plasma (PRP) and has a higher concentration of platelets than bone marrow aspirate concentrate (BMAC). what is typically found in blood. This higher Each of those treatments uses natural material concentration speeds the healing process. drawn from the body, prepared to maximize What can PRP treat? possible benefits, then reintroduced to the body to help restore injured tissue, ease pain and Research studies have found platelet-rich plasma restore function. to be most effective in treating arthritis in the knee. -
ACL Reconstruction Rehabilitation Protocol
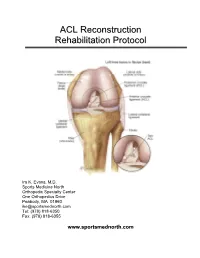
AACCLL RReeccoonnssttrruuccttiioonn RReehhaabbiilliittaattiioonn PPrroottooccooll Ira K. Evans, M.D. Sports Medicine North Orthopedic Specialty Center One Orthopedics Drive Peabody, MA 01960 [email protected] Tel: (978) 818-6350 Fax: (978) 818-6355 www.sportsmednorth.com ACL Reconstruction Rehabilitation Protocol Table of Contents Preoperative Rehabilitation Phase ...................................................................................... 3 Postoperative Days 1-7 ....................................................................................................... 9 Postoperative Days 8-10 ................................................................................................... 14 Postoperative Week 2 ....................................................................................................... 15 Postoperative Weeks 3-4 .................................................................................................. 17 Postoperative Weeks 4-6 .................................................................................................. 18 Postoperative Weeks 6-12 ................................................................................................ 19 Postoperative Weeks 12 - 20 ............................................................................................ 19 24 Weeks Postoperative (6 months) ................................................................................. 20 Medication Regimen ........................................................................................................ -

REHAB for RAPID RECOVERY of PULLED HAMSTRING SPOTLIGHT the Hamstring Muscles, Located at the Back of the Thigh, Are Comprised of Three Muscle Groups
5 Locations to Serve You! Berlin: 814.267.4393 Ebensburg: 814.472.9070 Richland: 814.269.9606 Somerset: 814.445.7727 Westmont: 814.255.6814 REHAB FOR RAPID RECOVERY OF PULLED HAMSTRING SPOTLIGHT The hamstring muscles, located at the back of the thigh, are comprised of three muscle groups. Injuries to this muscle are common in athletes participating in sports such as football or basketball. They are also common in 'weekend warriors' and individuals who participate in walking, jogging or running without a period of adequate warm up and stretching. This muscle group allows your knee to bend, and plays a critical role in every activity involving the lower body. Your hamstrings are contracting every single time you take a step, climb a flight of stairs or get in and out of Tammie Basala, PT your car. BS: Physical Therapy, West Virginia University The anatomy of this muscle group Certificates: NDT Treatment of The three muscle groups that comprise the hamstrings Children with Cerebral Palsy – include the biceps femoris, semi-membranosus and semi- Neurodevelopment tendinosus. A partial or complete tear of either of these Therapy Association muscles is a likely possibility in hamstring injuries. Certified Therapeutic Riding Instructor – PA Council on Cause of hamstring muscle injury Therapeutic Horsemanship A sudden, excessive stress on this muscle group is a common cause of injury. An Certified: Graston Technique individual with a previous history of hamstring injuries is more likely to get re-injured. Hamstring muscle tightness and inadequate warm-up can also cause injuries. A native of Somerset County, Tammie has considerable The Role of The Physical Therapist experience in treating a wide variety of orthopedic and The role of the physical therapist is extremely important neurological conditions. -
Pulled-Hamstring-Part-2-Essential
essential skills BY BEN E. BENJAMIN 94 massage & bodywork november/december 2011 088-107 MNB ND 11.indd 94 9/23/11 2:02 PM PULLED HAMSTRING, PART 2 In Part 1 of this article, we The entire healing process should take between 1–6 weeks, began our discussion of the depending on the severity of the injury. If self-treatment does not hamstrings by taking a look help within two weeks, professional treatment should be sought. at the anatomy, how and why Friction TheRaPy these muscles are frequently These treatments are very effective for reducing adhesive scar tissue and injured, and how to assess inhibiting re-formation of poorly formed scar tissue. I will describe precisely where the various friction massage for the three most Semimembranosis injured areas: the muscle belly, the common tendon at or near the ischial hamstring injuries occur in the Semitendinosis tuberosity, and the distal portion of Biceps Femoris posterior thigh. Now, in Part 2, the hamstrings behind the knee. we’ll cover the specific friction Friction therapy to the muscle belly. When treating the muscle belly, there therapy treatment techniques is often a broad area of adhesive scar tissue that requires treatment. With and rehabilitation exercises. the client lying prone, the practitioner stands facing the injured thigh. Depending on the size of the area that TREATMENT CHOICES needs to be worked, the practitioner Self-TReaTmenT may use just a few fingers to friction Whenever possible, it is important Sobotta: Atlas der Anatomie des Menschen the injured portion of the muscle or to avoid activities that create pain. -

Topical Pain Relief April.LN G__Layout 1 14/04/2015 11:39 Page 1 Education
OTC_topical pain relief_april.LN_G__Layout 1 14/04/2015 11:39 Page 1 education Supporting Training Initiatives the otc exce ing lle in n a c r e t • in Quality Seal IG treatment clinic a s 2015 C so th ciation wi Common conditions and their treatment options This module has been endorsed with the NPA’s Training Seal as suitable for use by medicines counter assistants as part of their ongoing learning. Complete the questions at the end to include in your self-development portfolio module 216 Welcome to TM’s OTC topical pain relief Treatment Clinic series. This handy, four-page section is specially designed so that author: Jane Feely, PhD you can detach it from the magazine and keep it for future reference. for this module Each month, TM covers a different OTC treatment area OBJECTIVES: After studying this module, assistants will: to help you keep up-to-date • Be familiar with the common causes of musculoskeletal pain with the latest product • Be able to advise on the OTC products available to help relieve common symptoms developments. In this issue, • Know when to recommend cold or heat therapy we focus on topical pain • Know which customers to refer to the pharmacist relief. At the end of the • Be able to offer self care tips to prevent injury. module there are multiple choice questions for you to complete, so your progress Countless charity campaigns and awareness weeks pain according to its origin. Here, we mainly focus can be monitored by your promote the importance of living a healthy, active on musculoskeletal pain, which is pain, soreness or pharmacist. -

The Art and Science of Kinesiology Taping, Part 2
MASSAGE Magazine http://www.massagemag.com The Art and Science of Kinesiology Taping, Part 2 This is the second installment of a two-part series on kinesiology taping. Click here to read “The Art and Science of Kinesiology Taping, Part 1.” How tape works Considering that the skin contains more mechanoreceptors than any other part of our body, it should come as no surprise how combining manual therapy with a tactile feedback mechanism like kinesiology tape can have incredible results that last long after our clients leave our treatment tables. When taping athletes, I can literally invoke movement re-education—think posture correction, patterning corrections, and muscle activation; reduce pain and inflammation; and increase sports performance and recovery, all while reinforcing the work done during manual therapy. All of this can be accomplished without restricting range of motion, and in about five minutes or less. Common ailments we see in our offices, such as rotator cuff injuries, whiplash, shin splints, knee issues, low back pain, upper trapezius pain and plantar fasciitis all can benefit from kinesiology taping. We all want solid research and evidence to support a treatment modality before we go experimenting on our clients. Paul Coker, P.T., medical director for RockTape, based in the United Kingdom, offers key scientific points for the role of kinesiology tape in treatment. According to him, the decompressive properties of tape provide three key effects to consider: the fluid effect, the mechanical effect and the neurological effect. Fluid effect The fluid effect is induced by the elastic properties of the tape, which produce a vertical lift of skin from the underlying tissue, thus decompressing the space between skin and muscle. -

Sprains, Strains & Sports Injuries
Emergency Conditions / First Aid Sprains, Strains & Sports Injuries Common Sports Injuries Shoulder joint separation Rotator cuff tear or Fractured collar bone tendinitis (back side of shoulder) Tennis elbow (pain on Side stitch (sharp pain the outside of forearm) felt underneath rib cage) Strained finger Low back strain (lower back) Knee injury (to ligament or cartilage) Pulled hamstring Shinsplint Muscle cramp Stress fracture (microfracture, usually Achilles tendon pain (stretch, in the bones in the feet, ankles, or tear, or irritation to the tendon legs, caused by sudden increase in the that connects the calf muscle to amount of weight bearing exercise) the back of the heel) Plantar fasciitis (irritation of ligaments Blisters (sores from friction) and tissues in the foot arch) Signs & Symptoms For Sprains A sprain happens when you overstretch or tear a ligament. (This is fibrous tissue that connects bones.) A joint is affected, but there is no dislocation or fracture. Symptoms are rapid pain, swelling, bruising, and a warm feeling at the injured site. For Strains A strain is an injury to the muscles or tendons. (These are tissues that connect muscles to bones.) Symptoms are pain, tenderness, swelling, and bruising. © American Institute for Preventive Medicine. All rights reserved. www.HealthyLife.com Emergencies & First Aid Sprains, Strains & Sports Injuries, Continued For Sports Injuries Are any of these signs present? Sports injury symptoms depend on the injury. • A bone sticks out or bones in the They include pain, tenderness, swelling, and injured part make a grating sound. bruising. Bones may be broken or dislocated. (See • An injured body part looks bent, Common Sports Injuries on previous page.) shortened, or misshaped.