Polyunsaturated Fatty Acids and Microbiota Relationship: Implications in Cancer Onset and Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fatty Acid Diets: Regulation of Gut Microbiota Composition and Obesity and Its Related Metabolic Dysbiosis
International Journal of Molecular Sciences Review Fatty Acid Diets: Regulation of Gut Microbiota Composition and Obesity and Its Related Metabolic Dysbiosis David Johane Machate 1, Priscila Silva Figueiredo 2 , Gabriela Marcelino 2 , Rita de Cássia Avellaneda Guimarães 2,*, Priscila Aiko Hiane 2 , Danielle Bogo 2, Verônica Assalin Zorgetto Pinheiro 2, Lincoln Carlos Silva de Oliveira 3 and Arnildo Pott 1 1 Graduate Program in Biotechnology and Biodiversity in the Central-West Region of Brazil, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; [email protected] (D.J.M.); [email protected] (A.P.) 2 Graduate Program in Health and Development in the Central-West Region of Brazil, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; pri.fi[email protected] (P.S.F.); [email protected] (G.M.); [email protected] (P.A.H.); [email protected] (D.B.); [email protected] (V.A.Z.P.) 3 Chemistry Institute, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; [email protected] * Correspondence: [email protected]; Tel.: +55-67-3345-7416 Received: 9 March 2020; Accepted: 27 March 2020; Published: 8 June 2020 Abstract: Long-term high-fat dietary intake plays a crucial role in the composition of gut microbiota in animal models and human subjects, which affect directly short-chain fatty acid (SCFA) production and host health. This review aims to highlight the interplay of fatty acid (FA) intake and gut microbiota composition and its interaction with hosts in health promotion and obesity prevention and its related metabolic dysbiosis. -

Omega-3 Eicosapentaenoic Acid (EPA)
nutrients Article Omega-3 Eicosapentaenoic Acid (EPA) Rich Extract from the Microalga Nannochloropsis Decreases Cholesterol in Healthy Individuals: A Double-Blind, Randomized, Placebo-Controlled, Three-Month Supplementation Study Amanda Rao 1,2 , David Briskey 1,3, Jakob O Nalley 4 and Eneko Ganuza 4,* 1 RDC Clinical, Brisbane 4006, Australia; [email protected] (A.R.); [email protected] (D.B.) 2 School of Medicine, University of Sydney, Sydney, NSW 2006, Australia 3 School of Human Movement and Nutrition Sciences, The University of Queensland, Brisbane, QLD 4067, Australia 4 Qualitas Health, Houston, TX 77056, USA; [email protected] * Correspondence: [email protected] Received: 26 May 2020; Accepted: 20 June 2020; Published: 23 June 2020 Abstract: The aim of this trial is to assess the effect of Almega®PL on improving the Omega-3 Index, cardio-metabolic parameters, and other biomarkers in generally healthy individuals. The benefits of long-chain omega-3 fatty acids for cardiovascular health are primarily built upon mixtures of docosahexaenoic (DHA) and eicosapentaenoic acids (EPA). Highly purified EPA therapy has proven to be particularly effective in the treatment of cardiovascular disease, but less is known about the benefits of EPA-only supplementation for the general healthy population. Almega®PL is a polar rich oil (>15%) derived from the microalga Nannochloropsis that contains EPA (>25%) with no DHA. Participants (n = 120) were given a capsule of 1 g/day of either Almega®PL or placebo for 12 weeks. Differences in the Omega-3 Index, cardiometabolic markers, and other general health indicators were measured at the baseline, six, and 12 weeks. -

Eicosapentaenoic Acid (EPA) Reduces Cardiovascular Events: Relationship with the EPA/Arachidonic Acid Ratio
Advance Publication Journal of AtherosclerosisJournal and Thrombosis of Atherosclerosis Vol.20, No.● and Thrombosis1 Review Accepted for publication: June 17, 2013 Published online: September 18, 2013 Eicosapentaenoic Acid (EPA) Reduces Cardiovascular Events: Relationship with the EPA/Arachidonic Acid Ratio Haruo Ohnishi1 and Yasushi Saito2 1Mochida Pharmaceutical Co. Ltd., Tokyo, Japan 2Chiba University Graduate School of Medicine, Chiba, Japan The clinical efficacy of fish oil and high-purity eicosapentaenoic acid ethyl ester (hp-EPA-E) for treat- ing cardiovascular disease (CVD) has been reported. Fish oil contains saturated and monounsatu- rated fatty acids that have pharmacological effects opposite to those of ω3 fatty acids (ω3). Moreover, ω3, such as EPA and docosahexaenoic acid (DHA), do not necessarily have the same metabolic and biological actions. This has obscured the clinical efficacy of ω3. Recently, the Japan EPA Lipid Inter- vention Study (JELIS) of hp-EPA-E established the clinical efficacy of EPA for CVD, and higher lev- els of blood EPA, not DHA, were found to be associated with a lower incidence of major coronary events. A significant reduction in the risk of coronary events was observed when the ratio of EPA to arachidonic acid (AA) (EPA/AA) was >0.75. Furthermore, the ratio of prostaglandin (PG) I3 and PGI2 to thromboxane A2 (TXA2) ([PGI2+PGI3]/TXA2) was determined to have a linear relationship with the EPA/AA ratio as follows: (PGI2+PGI3)/TXA2 =λ+π* (EPA/AA). Like PGI2, PGI3 not only inhib- its platelet aggregation and vasoconstriction, but also is assumed to reduce cardiac ischemic injury and arteriosclerosis and promote angiogenesis. -

Enriched in Eicosapentaenoic Acid
Immunology 1982 46 819 Enhanced production of IgE and IgG antibodies associated with a diet enriched in eicosapentaenoic acid J. D. PRICKETT, D. R. ROBINSON & K. J. BLOCH Department ofMedicine, Harvard Medical School, and the Arthritis, Clinical Immunology and Allergy Units of the Medical Services, Massachusetts General Hospital, Boston, Massachusetts, U.S.A. Acceptedfor publication 15 February 1982 Summary. Eicosapentaenoic acid (EPA), a polyunsa- Passive inflammatory reactions, as evaluated by pas- turated fatty acid analog of arachidonic acid, alters sive cutaneous anaphylaxis elicited with IgE antibody, certain platelet functions controlled by prostaglandins and by the intradermal injection of aggregated IgG, and thromboxanes, probably by inhibiting the syn- were not significantly different between the two thesis of these molecules from arachidonic acid. This groups. EPA constituted 7-3% offatty acid in the livers study reports the effects of a diet enriched in EPA of FFD rats, v. 0 3% in BFD rats (P<0 01). These (fish-fat diet, FFD) as compared with a diet lacking data demonstrate enhanced levels of IgE and IgG EPA (beef-fat diet, BFD) upon certain immunological antibody in FFD rats, with subsequent increased and inflammatory responses in outbred Sprague Daw- active inflammatory reactivity in these animals. These ley rats. Induction of antibody formation to egg alterations may be secondary to enrichment of tissue albumin (EA) produced four- to eight-fold greater lipids with EPA, although effects due to changes in titres of IgE (P < 002) and IgG (P < 003) anti-EA other fatty acids have not been excluded. antibodies in FFD rats v. BFD rats. -

Compounds with Anti-Aging Activities
(19) TZZ ZZ_T (11) EP 2 862 600 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 22.04.2015 Bulletin 2015/17 A61Q 19/08 (2006.01) A61K 8/49 (2006.01) A61K 8/36 (2006.01) A61K 8/44 (2006.01) (2006.01) (2006.01) (21) Application number: 14196664.8 A61K 8/63 A61K 8/64 A61K 8/33 (2006.01) A61K 8/60 (2006.01) (2006.01) (2006.01) (22) Date of filing: 20.12.2011 A61Q 17/04 A61K 8/42 A61Q 1/02 (2006.01) A61Q 19/00 (2006.01) A61Q 19/02 (2006.01) A61Q 19/04 (2006.01) A61Q 19/10 (2006.01) A61K 31/11 (2006.01) A61K 31/197 (2006.01) A61K 31/202 (2006.01) A61K 31/343 (2006.01) A61K 31/353 (2006.01) A61K 31/704 (2006.01) (84) Designated Contracting States: • Mavon, Alain Robert Pierre AL AT BE BG CH CY CZ DE DK EE ES FI FR GB 11264 Stockholm (SE) GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO • Duracher, Lucie PL PT RO RS SE SI SK SM TR 11761 Stockholm (SE) Designated Extension States: • Klack, Anke BA ME 11244 Stockholm (SE) • Cattley, Kevin (62) Document number(s) of the earlier application(s) in Wexford (IE) accordance with Art. 76 EPC: 11797020.2 / 2 729 220 (74) Representative: Moore, Michael Richard et al Keltie LLP (71) Applicant: Oriflame Research and Development No.1 London Bridge Ltd. London SE1 9BA (GB) Bray, Co. Wicklow (IE) Remarks: (72) Inventors: This application was filed on 05-12-2014 as a • Gillbro, Johanna Maria divisional application to the application mentioned 11736 Stockholm (SE) under INID code 62. -

Fatty Acids: Structures and Introductory Article Properties Article Contents
Fatty Acids: Structures and Introductory article Properties Article Contents . Introduction Arild C Rustan, University of Oslo, Oslo, Norway . Overview of Fatty Acid Structure . Major Fatty Acids Christian A Drevon, University of Oslo, Oslo, Norway . Metabolism of Fatty Acids . Properties of Fatty Acids Fatty acids play a key role in metabolism: as a metabolic fuel, as a necessary component of . Requirements for and Uses of Fatty Acids in Human all membranes, and as a gene regulator. In addition, fatty acids have a number of industrial Nutrition uses. Uses of Fatty Acids in the Pharmaceutical/Personal Hygiene Industries Introduction doi: 10.1038/npg.els.0003894 Fatty acids, both free and as part of complex lipids, play a number of key roles in metabolism – major metabolic fuel (storage and transport of energy), as essential components subsequent one the b carbon. The letter n is also often used of all membranes, and as gene regulators (Table 1). In ad- instead of the Greek o to indicate the position of the double dition, dietary lipids provide polyunsaturated fatty acids bond closest to the methyl end. The systematic nomencla- (PUFAs) that are precursors of powerful locally acting ture for fatty acids may also indicate the location of double metabolites, i.e. the eicosanoids. As part of complex lipids, bonds with reference to the carboxyl group (D). Figure 2 fatty acids are also important for thermal and electrical outlines the structures of different types of naturally insulation, and for mechanical protection. Moreover, free occurring fatty acids. fatty acids and their salts may function as detergents and soaps owing to their amphipathic properties and the for- Saturated fatty acids mation of micelles. -
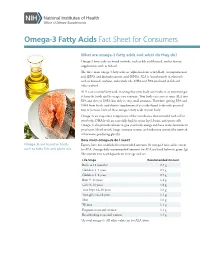
Omega-3 Fatty Acids Fact Sheet for Consumers
Omega-3 Fatty Acids Fact Sheet for Consumers What are omega-3 fatty acids and what do they do? Omega-3 fatty acids are found in foods, such as fish and flaxseed, and in dietary supplements, such as fish oil. The three main omega-3 fatty acids are alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA is found mainly in plant oils such as flaxseed, soybean, and canola oils. DHA and EPA are found in fish and other seafood. ALA is an essential fatty acid, meaning that your body can’t make it, so you must get it from the foods and beverages you consume. Your body can convert some ALA into EPA and then to DHA, but only in very small amounts. Therefore, getting EPA and DHA from foods (and dietary supplements if you take them) is the only practical way to increase levels of these omega-3 fatty acids in your body. Omega-3s are important components of the membranes that surround each cell in your body. DHA levels are especially high in retina (eye), brain, and sperm cells. Omega-3s also provide calories to give your body energy and have many functions in your heart, blood vessels, lungs, immune system, and endocrine system (the network of hormone-producing glands). How much omega-3s do I need? Omega-3s are found in foods Experts have not established recommended amounts for omega-3 fatty acids, except such as fatty fish and plant oils. for ALA. Average daily recommended amounts for ALA are listed below in grams (g). -

Revealing the Role of Short Chain and Polyunsaturated Fatty Acids As
Southern Illinois University Carbondale OpenSIUC Honors Theses University Honors Program 2019 Revealing the Role of Short Chain and Polyunsaturated Fatty Acids as Regulators of Metabolic Activity and Gene Expression in Ovarian Cancer Abigayle Ochs [email protected] Follow this and additional works at: https://opensiuc.lib.siu.edu/uhp_theses Recommended Citation Ochs, Abigayle, "Revealing the Role of Short Chain and Polyunsaturated Fatty Acids as Regulators of Metabolic Activity and Gene Expression in Ovarian Cancer" (2019). Honors Theses. 461. https://opensiuc.lib.siu.edu/uhp_theses/461 This Dissertation/Thesis is brought to you for free and open access by the University Honors Program at OpenSIUC. It has been accepted for inclusion in Honors Theses by an authorized administrator of OpenSIUC. For more information, please contact [email protected]. REVEALING THE ROLE OF SHORT CHAIN AND POLYUNSATURATED FATTY ACIDS AS REGULATORS OF METABOLIC ACTIVITY AND GENE EXPRESSION IN OVARIAN CANCER Abigayle Ochs A thesis submitted to the University Honors Program in partial fulfillment of the requirements for the Honors Certificate with Thesis Southern Illinois University Carbondale May 2019 Ochs 2 I. Abstract Previous research using the chicken model has provided evidence that a flaxseed- supplemented diet decreases both the severity and the incidence of ovarian cancer. Flaxseed is a source of omega-3 (OM3) polyunsaturated fatty acids (PUFA), particularly α-linolenic acid (ALA). ALA is converted into longer chain OM3s, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which inhibit prostaglandins, thereby inhibiting oxidative stress, inflammation, angiogenesis, and proliferation. The dietary fiber component of flaxseed can be fermented in the gut to produce short chain fatty acids (SCFA). -

Eicosapentaenoic Acid (EPA)
2500, Parc-Technologique Blvd Quebec City (Quebec) G1P 4S6 CANADA Tel.: +1 418 874.0054 / Fax: +1 418 874.0355 Toll Free: +1 877 745.4292 (North America Only) Email: [email protected] Product Information Eicosapentaenoic acid (EPA) Identification Product Number EPA-GP-xxx CAS Number 10417-94-4 EN Number N/A Common Name Eicosapentaenoic acid Systematic Name cis-5,8,11,14,17-Eicosapentaenoic acid 20:5(n-3); Icosapentaenoic acid; Alternative Names Timnodonic acid Storage Temperature -80°C or lower Characteristics Specifications Molecular Formula C20H30O2 Purity ≥ 99 % Molecular Weight 302.45 g/mol Form Liquid above -54°C Melting Point -54 to -53°C Color Clear, colorless Density 0.943 g/mL at 25°C (lit.) Precautions & Disclaimer For laboratory use only. Not for use on humans. Not for drug, household or other uses. Handling & Preparation Instructions This purified fatty acid is liquid at room temperature (oil) and not soluble in water. It can be solubilized in undiluted serum or in ethanol or DMSO. Essential fatty acids are also soluble in chloroform or ether, however it is not recommended with the use of cells. After reconstitution, the product can be aliquoted and stored at -80°C. We recommend adding the essential fatty acids cocktail to the medium the day of use. The concentration to add to the culture is to be determined by the user. As a starting point, we provide some references from the literature. Chen et al. treated primary microglial cells with 20 µM of EPA [1]. Hampel et al. treated human epithelial cells with 100 µM of EPA [2]. -

Therapeutic Effects of Specialized Pro-Resolving Lipids Mediators On
antioxidants Review Therapeutic Effects of Specialized Pro-Resolving Lipids Mediators on Cardiac Fibrosis via NRF2 Activation 1, 1,2, 2, Gyeoung Jin Kang y, Eun Ji Kim y and Chang Hoon Lee * 1 Lillehei Heart Institute, University of Minnesota, Minneapolis, MN 55455, USA; [email protected] (G.J.K.); [email protected] (E.J.K.) 2 College of Pharmacy, Dongguk University, Seoul 04620, Korea * Correspondence: [email protected]; Tel.: +82-31-961-5213 Equally contributed. y Received: 11 November 2020; Accepted: 9 December 2020; Published: 10 December 2020 Abstract: Heart disease is the number one mortality disease in the world. In particular, cardiac fibrosis is considered as a major factor causing myocardial infarction and heart failure. In particular, oxidative stress is a major cause of heart fibrosis. In order to control such oxidative stress, the importance of nuclear factor erythropoietin 2 related factor 2 (NRF2) has recently been highlighted. In this review, we will discuss the activation of NRF2 by docosahexanoic acid (DHA), eicosapentaenoic acid (EPA), and the specialized pro-resolving lipid mediators (SPMs) derived from polyunsaturated lipids, including DHA and EPA. Additionally, we will discuss their effects on cardiac fibrosis via NRF2 activation. Keywords: cardiac fibrosis; NRF2; lipoxins; resolvins; maresins; neuroprotectins 1. Introduction Cardiovascular disease is the leading cause of death worldwide [1]. Cardiac fibrosis is a major factor leading to the progression of myocardial infarction and heart failure [2]. Cardiac fibrosis is characterized by the net accumulation of extracellular matrix proteins in the cardiac stroma and ultimately impairs cardiac function [3]. Therefore, interest in substances with cardioprotective activity continues. -

(EPA), Exerts Anti-Inflammatory Properties In
nutrients Article N-Eicosapentaenoyl Dopamine, A Conjugate of Dopamine and Eicosapentaenoic Acid (EPA), Exerts Anti-inflammatory Properties in Mouse and Human Macrophages 1, 1, 1 1, Giuseppina Augimeri y, Pierluigi Plastina y , Giulia Gionfriddo , Daniela Rovito z, Cinzia Giordano 1, Alessia Fazio 1, Ines Barone 1, Stefania Catalano 1, Sebastiano Andò 1, Daniela Bonofiglio 1,* , Jocelijn Meijerink 2 and Renger Witkamp 2,* 1 Department of Pharmacy, Health and Nutritional Sciences, University of Calabria, 87036 Arcavacata di Rende (CS), Italy; [email protected] (G.A.); [email protected] (P.P); [email protected] (G.G.); [email protected] (D.R.); [email protected] (C.G.); [email protected] (A.F.); [email protected] (I.B.); [email protected] (S.C.); [email protected] (S.A.) 2 Division of Human Nutrition and Health, Wageningen University, 6700 AA Wageningen, The Netherlands; [email protected] * Correspondence: daniela.bonofi[email protected] (D.B.); [email protected] (R.W.); Tel.: +39-0984-496208 (D.B.); +31-0317-485136 (R.W.) These authors contributed equally to this work. y Present address: Department of Functional Genomics and Cancer, Institut de Génétique et de Biologie z Moléculaire et Cellulaire, 67404 Illkirch-Graffenstaden, France. Received: 23 July 2019; Accepted: 16 September 2019; Published: 18 September 2019 Abstract: A large body of evidence suggests that dietary n-3 polyunsaturated fatty acids (PUFAs), including eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), contribute to a reduced inflammatory tone thereby lowering the risk for several chronic and degenerative diseases. Different mechanisms have been proposed to explain these anti-inflammatory effects, including those involving endocannabinoids and endocannabinoid-like molecules. -

Omega-3, Omega-6 and Omega-9 Fatty Acids
Johnson and Bradford, J Glycomics Lipidomics 2014, 4:4 DOI: 0.4172/2153-0637.1000123 Journal of Glycomics & Lipidomics Review Article Open Access Omega-3, Omega-6 and Omega-9 Fatty Acids: Implications for Cardiovascular and Other Diseases Melissa Johnson1* and Chastity Bradford2 1College of Agriculture, Environment and Nutrition Sciences, Tuskegee University, Tuskegee, Alabama, USA 2Department of Biology, Tuskegee University, Tuskegee, Alabama, USA Abstract The relationship between diet and disease has long been established, with epidemiological and clinical evidence affirming the role of certain dietary fatty acid classes in disease pathogenesis. Within the same class, different fatty acids may exhibit beneficial or deleterious effects, with implications on disease progression or prevention. In conjunction with other fatty acids and lipids, the omega-3, -6 and -9 fatty acids make up the lipidome, and with the conversion and storage of excess carbohydrates into fats, transcendence of the glycome into the lipidome occurs. The essential omega-3 fatty acids are typically associated with initiating anti-inflammatory responses, while omega-6 fatty acids are associated with pro-inflammatory responses. Non-essential, omega-9 fatty acids serve as necessary components for other metabolic pathways, which may affect disease risk. These fatty acids which act as independent, yet synergistic lipid moieties that interact with other biomolecules within the cellular ecosystem epitomize the critical role of these fatty acids in homeostasis and overall health. This review focuses on the functional roles and potential mechanisms of omega-3, omega-6 and omega-9 fatty acids in regard to inflammation and disease pathogenesis. A particular emphasis is placed on cardiovascular disease, the leading cause of morbidity and mortality in the United States.