Neurologic Disease and Common Sleep Comorbidities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Status Epilepticus Clinical Pathway
JOHNS HOPKINS ALL CHILDREN’S HOSPITAL Status Epilepticus Clinical Pathway 1 Johns Hopkins All Children's Hospital Status Epilepticus Clinical Pathway Table of Contents 1. Rationale 2. Background 3. Diagnosis 4. Labs 5. Radiologic Studies 6. General Management 7. Status Epilepticus Pathway 8. Pharmacologic Management 9. Therapeutic Drug Monitoring 10. Inpatient Status Admission Criteria a. Admission Pathway 11. Outcome Measures 12. References Last updated: July 7, 2019 Owners: Danielle Hirsch, MD, Emergency Medicine; Jennifer Avallone, DO, Neurology This pathway is intended as a guide for physicians, physician assistants, nurse practitioners and other healthcare providers. It should be adapted to the care of specific patient based on the patient’s individualized circumstances and the practitioner’s professional judgment. 2 Johns Hopkins All Children's Hospital Status Epilepticus Clinical Pathway Rationale This clinical pathway was developed by a consensus group of JHACH neurologists/epileptologists, emergency physicians, advanced practice providers, hospitalists, intensivists, nurses, and pharmacists to standardize the management of children treated for status epilepticus. The following clinical issues are addressed: ● When to evaluate for status epilepticus ● When to consider admission for further evaluation and treatment of status epilepticus ● When to consult Neurology, Hospitalists, or Critical Care Team for further management of status epilepticus ● When to obtain further neuroimaging for status epilepticus ● What ongoing therapy patients should receive for status epilepticus Background: Status epilepticus (SE) is the most common neurological emergency in children1 and has the potential to cause substantial morbidity and mortality. Incidence among children ranges from 17 to 23 per 100,000 annually.2 Prevalence is highest in pediatric patients from zero to four years of age.3 Ng3 acknowledges the most current definition of SE as a continuous seizure lasting more than five minutes or two or more distinct seizures without regaining awareness in between. -

Central Periodic Breathing During Sleep in 74 Patients with Acute Ischemic Stroke - Neurogenic and Cardiogenic Factors
Siccoli, M M; Valko, P O; Hermann, D M; Bassetti, C L (2008). Central periodic breathing during sleep in 74 patients with acute ischemic stroke - Neurogenic and cardiogenic factors. Journal of Neurology, 255(11):1687-1692. Postprint available at: http://www.zora.uzh.ch University of Zurich Posted at the Zurich Open Repository and Archive, University of Zurich. Zurich Open Repository and Archive http://www.zora.uzh.ch Originally published at: Journal of Neurology 2008, 255(11):1687-1692. Winterthurerstr. 190 CH-8057 Zurich http://www.zora.uzh.ch Year: 2008 Central periodic breathing during sleep in 74 patients with acute ischemic stroke - Neurogenic and cardiogenic factors Siccoli, M M; Valko, P O; Hermann, D M; Bassetti, C L Siccoli, M M; Valko, P O; Hermann, D M; Bassetti, C L (2008). Central periodic breathing during sleep in 74 patients with acute ischemic stroke - Neurogenic and cardiogenic factors. Journal of Neurology, 255(11):1687-1692. Postprint available at: http://www.zora.uzh.ch Posted at the Zurich Open Repository and Archive, University of Zurich. http://www.zora.uzh.ch Originally published at: Journal of Neurology 2008, 255(11):1687-1692. CENTRAL PERIODIC BREATHING IN 74 PATIENTS WITH ACUTE ISCHEMIC STROKE - NEUROGENIC VERSUS CARDIOGENIC FACTORS Massimiliano M. Siccoli, MD Philipp O. Valko, MD Dirk M. Hermann, MD Claudio L. Bassetti, MD Department of Neurology, University Hospital of Zurich, Switzerland Correspondence: Prof. Claudio L. Bassetti Department of Neurology University Hospital of Zurich Frauenklinikstrasse 26 -

Non-Epileptic Seizures a Short Guide for Patients and Families
Non-epileptic seizures a short guide for patients and families Department of Neurology Information for patients Royal Hallamshire Hospital What are non-epileptic seizures? In a seizure people lose control of their body, often causing shaking or other movements of arms and legs, blacking out, or both. Seizures can happen for different reasons. During epileptic seizures, the brain produces electrical impulses, which stop it from working normally. Non-epileptic seizures look a little like epileptic seizures, but are not caused by abnormal electrical activity in the brain. Non-epileptic seizures happen because of problems with handling thoughts, memories, emotions or sensations in the brain. Such problems are sometimes related to stress. However, they can also occur in people who seem calm and relaxed. Often people do not understand why they have developed non-epileptic seizures. Are non-epileptic seizures rare? For every 100,000 people, between 15 and 30 have non- epileptic seizures. Nearly half of all people brought in to hospital with suspected serious epilepsy turn out to have non- epileptic seizures instead. One of the reasons why you may not have heard of non- epileptic seizures is that there are several other names for the same problem. Non-epileptic seizures are also known as pseudoseizures, psychogenic, dissociative or functional seizures. Sometimes people who have non-epileptic seizures are told that they suffer from non-epileptic attack disorder (NEAD). How can I be sure that this is the right diagnosis? Non-epileptic seizures often look like epileptic seizures to friends, family members and even doctors. Like epilepsy, non- epileptic seizures can cause injuries and loss of control over bladder function. -

Sleep Apnea Sleep Apnea
Health and Safety Guidelines 1 Sleep Apnea Sleep Apnea Normally while sleeping, air is moved at a regular rhythm through the throat and in and out the lungs. When someone has sleep apnea, air movement becomes decreased or stops altogether. Sleep apnea can affect long term health. Types of sleep apnea: 1. Obstructive sleep apnea (narrowing or closure of the throat during sleep) which is seen most commonly, and, 2. Central sleep apnea (the brain is causing a change in breathing control and rhythm) Obstructive sleep apnea (OSA) About 25% of all adults are at risk for sleep apnea of some degree. Men are more commonly affected than women. Other risk factors include: 1. Middle and older age 2. Being overweight 3. Having a small mouth and throat Down syndrome Because of soft tissue and skeletal alterations that lead to upper airway obstruction, people with Down syndrome have an increased risk of obstructive sleep apnea. Statistics show that obstructive sleep apnea occurs in at least 30 to 75% of people with Down syndrome, including those who are not obese. In over half of person’s with Down syndrome whose parents reported no sleep problems, sleep studies showed abnormal results. Sleep apnea causing lowered oxygen levels often contributes to mental impairment. How does obstructive sleep apnea occur? The throat is surrounded by muscles that are active controlling the airway during talking, swallowing and breathing. During sleep, these muscles are much less active. They can fall back into the throat, causing narrowing. In most people this doesn’t affect breathing. However in some the narrowing can cause snoring. -

The Migraine-Epilepsy Syndrome
medigraphic Artemisaen línea Arch Neurocien (Mex) Vol 11, No. 4: 282-287, 2006 The Migraine- Epilepsy Syndrome Arch Neurocien (Mex) Vol. 11, No. 4: 282-287, 2006 Artículo de revisión ©INNN, 2006 de caso The migraine-epilepsy syndrome Enrique Otero Siliceo†, Fernando Zermeño EL SINDROME MIGRAÑA-EPILEPSIA represent a neural exitation. Since that the glutamate has in important rol in both patologys depending of the part of the brain more affected the symptoms might RESUMEN vary from visual to abdominal phemomena. La migraña y la epilepsia tienen varios puntos en común Key words: migraine epilepsy, EEG abnormalities, sintomática clínica y genéticamente lo que ha sido glutamate, diagnosis. postulado por más de cien años. El fenómeno referido como migraña-epilepsia sugiere que exista una he first steps of a practical, approach by patofisiología común. El síndrome de migraña o physicians in recognizing and treating neuro- epilepsia tiene fenómenos comunes de dolor adominal T logic diseases are to recognithat there are jaqueca anormalidades del EE y respuesta a droga various overlaps between migraine and epilepsy. antiepilépticas. En ocasiones el paciente puede tener Epileptic seizures and classic migraine episodes may un ataque migrañoso o una convulsión o en otras occur in the same patient. Migraine and epilepsy share ambas. La comorbilidad puede explicarse por estados several genetic, clinical, evolutive and neurophysio- de hiperrexcitabilidad neural. Alteraciones electroen- logic features. A relationship between epilepsy and cefalográficas son comunes en estos estados. En migraine has been postulated for over a hundred years apariencia el glutamato tiene un papel importante tanto and the syndrome of Migraine-Epilepsy illustrates this en la migraña como en la epilepsia. -

A Clinical Guide to Epileptic Syndromes and Their Treatment
Published August 13, 2008 as 10.3174/ajnr.A1231 dures and principles of treatment. These chapters are particu- BOOK REVIEW larly important for readers unfamiliar with the overall clinical presentation of the epilepsies and their diagnostic evaluation. A Clinical Guide to Epileptic Omitting these topics was a certain pitfall that has been Syndromes and Their Treatment, avoided. Basic techniques used in the evaluation of patients with of epilepsy, including anatomic and functional neuroim- 2nd ed. aging, are also included. The discussion of the relative value of C.P. Panayiotopoulos, ed. London, UK: Springer-Verlag; 2007, 578 EEG and its problems is particularly valuable. pages, 100 illustrations, $99.00. Subsequent chapters are devoted to the meat of the book, the epilepsy syndromes. These are presented in age-based he syndromic classification of epileptic seizures has been chronologic order, beginning with syndromes in the neonate evolving for more than a quarter century. Piggy-backed T and infant and continuing through syndromes in adults. onto major advances in neurophysiology and neuroimaging, Complete coverage of reflex seizures and reflex epilepsies in the current nomenclature of specific clinical epilepsy syn- chapter 16 is particularly welcome. Chapter 17 covers a group dromes now supersedes earlier seizure classifications based of disorders that are associated with epileptic seizures. The exclusively on seizure types. The practice of epilepsy has thus chapter gives excellent coverage of these disorders but makes joined mainstream medicine through its newfound ability to no pretenses at being comprehensive. For example, coverage link the signs and symptoms of epilepsy with specific under- of important disorders with epilepsy such as the Wolf- lying disorders. -

Migraine Triggered Seizures and Epilepsy Triggered Headache and Migraine Attacks: a Need for Re-Assessment
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central J Headache Pain (2011) 12:287–288 DOI 10.1007/s10194-011-0344-2 COMMENTARY Migraine triggered seizures and epilepsy triggered headache and migraine attacks: a need for re-assessment Paul T. G. Davies • C. P. Panayiotopoulos Received: 5 April 2011 / Accepted: 8 April 2011 / Published online: 24 April 2011 Ó The Author(s) 2011. This article is published with open access at Springerlink.com In this issue of the Journal, Belcastro and associates review Migralepsy terminology and classification issues for migralepsy, hem- icrania epileptica, post-ictal and ictal headache [1]. They According to the ICHD-II 1.5.5, ‘‘migraine-triggered sei- raise key points such as ictal headache and visual seizures zure (sometimes referred to as migralepsy)’’ denotes an are often misdiagnosed as migraine, ‘‘migralepsy’’ is unli- epileptic seizure that occurs ‘‘during or within one hour kely to exist and an ‘‘epilepsy-migraine sequence’’ is much after a migraine aura’’ [3]. However, the evidence of this more common and well documented than the dominant ‘‘migraine-seizure’’ sequence is weak and the proposed view of a ‘‘migraine-epilepsy sequence’’. Their relevant criterion of 1 h gap between the end of the ‘‘aura’’ and the proposals need appropriate attention by the committee of start of an epileptic seizure is entirely arbitrary the international classification of headache disorders Migralepsy is an old term derived from migra(ine) and (ICHD) as well as the physicians in their clinical practice (epi)lepsy, coined by Dr Douglas Davidson, but mainly because of the consequences that misdiagnosis may have on attributed to Lennox and Lennox, which we quote, ‘‘a patients. -

Myoclonic Status Epilepticus in Juvenile Myoclonic Epilepsy
Original article Epileptic Disord 2009; 11 (4): 309-14 Myoclonic status epilepticus in juvenile myoclonic epilepsy Julia Larch, Iris Unterberger, Gerhard Bauer, Johannes Reichsoellner, Giorgi Kuchukhidze, Eugen Trinka Department of Neurology, Medical University of Innsbruck, Austria Received April 9, 2009; Accepted November 18, 2009 ABSTRACT – Background. Myoclonic status epilepticus (MSE) is rarely found in juvenile myoclonic epilepsy (JME) and its clinical features are not well described. We aimed to analyze MSE incidence, precipitating factors and clini- cal course by studying patients with JME from a large outpatient epilepsy clinic. Methods. We retrospectively screened all patients with JME treated at the Department of Neurology, Medical University of Innsbruck, Austria between 1970 and 2007 for a history of MSE. We analyzed age, sex, age at seizure onset, seizure types, EEG, MRI/CT findings and response to antiepileptic drugs. Results. Seven patients (five women, two men; median age at time of MSE 31 years; range 17-73) with MSE out of a total of 247 patients with JME were identi- fied. The median follow-up time was seven years (range 0-35), the incidence was 3.2/1,000 patient years. Median duration of epilepsy before MSE was 26 years (range 10-58). We identified three subtypes: 1) MSE with myoclonic seizures only in two patients, 2) MSE with generalized tonic clonic seizures in three, and 3) generalized tonic clonic seizures with myoclonic absence status in two patients. All patients responded promptly to benzodiazepines. One patient had repeated episodes of MSE. Precipitating events were identified in all but one patient. Drug withdrawal was identified in four patients, one of whom had additional sleep deprivation and alcohol intake. -
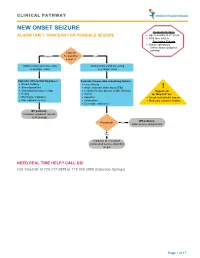
Seizure, New Onset
CLINICAL PATHWAY NEW ONSET SEIZURE Inclusion Criteria ALGORITHM 1. CONCERN FOR POSSIBLE SEIZURE • Age 6 months to 21 years • First-time seizure Exclusion Criteria • Status epilepticus (refer to status epilepticus pathway) Concern Unsure for possible Yes seizure? Obtain history and screening Obtain history and screening neurologic exam neurologic exam Consider differential diagnoses: Evaluate for possible provoking factors: • Breath holding • Fever/illness • Stereotypies/tics • Acute traumatic brain injury (TBI) ! • Vasovagal/syncope/vertigo • Central nervous system (CNS) infection Urgent call • Reflux • Tumor to ‘OneCall’ for: • Electrolyte imbalance • Ingestion • Suspected infantile spasm • Non epileptic seizure • Intoxication • Medically complex children • Electrolyte imbalance Off pathway: Consider outpatient referral to Neurology Off pathway: Provoked? Yes Address provoking factors No Continue to new onset unprovoked seizure algorithm on p.2 NEED REAL TIME HELP? CALL US! Call ‘OneCall’ at 720-777-3999 or 719-305-3999 (Colorado Springs) Page 1 of 17 CLINICAL PATHWAY ALGORITHM 2. NEW ONSET UNPROVOKED SEIZURE Inclusion Criteria • Age 6 months to 21 years New onset unprovoked • First-time unprovoked seizure seizure • Newly recognized seizure or epilepsy syndrome Exclusion Criteria • Provoked seizure: any seizure as a symptom of fever/illness, acute traumatic brain injury (TBI), Has central nervous system (CNS) infection, tumor, patient returned ingestion, intoxication, or electrolyte imbalance Consult inpatient • to baseline within No -

Respiratory Assist Device Appendices a and B
DRAFT Appendix A Clinical Indications for the Use of Respiratory Assist Device (RAD) Therapy Indications for use of a RAD is divided into four categories: • Restrictive thoracic disorders, e.g., neuromuscular disorders such as amyotrophic lateral sclerosis; • Severe chronic obstructive pulmonary disease (COPD); o Use of a RAD in COPD patients requires, . A facility-based polysomnogram to rule out obstructive sleep apnea in order to initiate Medicare coverage, . A prerequisite trial of noninvasive ventilation without a backup rate, and . Treatment with continuous positive airway pressure devices. • Central sleep apnea, i.e., apnea not due to airway obstruction; and • Obstructive sleep apnea (OSA). Initial Coverage (First 3 Months of Therapy) Medical record must document symptoms characteristic of sleep-associated hypoventilation, e.g.: • Daytime hypersomnolence; • Excessive fatigue; • Morning headache; • Cognitive dysfunction; • Dyspnea, etc.; and • Beneficiary has one (1) of the disorders listed in the Documentation Verification Procedures section below and meets all coverage criteria for that disorder. Continued Coverage (Beyond First 3 Months of Therapy) - E0470 or E0471 Medical records document the beneficiary was re-evaluated on/after the 61st day of therapy demonstrating: • Progress of relevant symptoms; and • Beneficiary usage of the device (average 4 hours per 24 hours) Documentation in supplier’s records includes the following: • Signed and dated physician statement completed no sooner than 61 days after initiating use of the -

Principles of Practice Parameters for The
ERJ Express. Published on July 28, 2016 as doi: 10.1183/13993003.01975-2015 TASK FORCE REPORT IN PRESS | CORRECTED PROOF Principles of practice parameters for the treatment of sleep disordered breathing in the elderly and frail elderly: the consensus of the International Geriatric Sleep Medicine Task Force Nikolaus C. Netzer (Chair)1,2, Sonia Ancoli-Israel (Co-chair)3, Donald L. Bliwise4, Stephany Fulda5, Christine Roffe6, Fernanda Almeida7, Hakki Onen8, Fannie Onen9, Friedhart Raschke10, Miguel Angel Martinez Garcia11 and Helmut Frohnhofen12 Affiliations: 1Hermann Buhl Institute for Hypoxia and Sleep Medicine Research, Dept of Sports Science, Faculty of Psychology and Sports Science, University Innsbruck, Austria. 2Division of Sports Medicine and Rehabilitation, Dept of Medicine, University Hospitals Ulm, Ulm, Germany. 3Depts of Psychiatry and Medicine, University of California, San Diego, CA, USA. 4Sleep Program, Dept of Neurology, Emory University, Atlanta, GA, USA. 5Sleep and Epilepsy Center, Neurocenter of Southern Switzerland, Lugano, Switzerland. 6Institute for Science and Technology in Medicine, Keele University, Keele, UK. 7Dental Medical School, University of British Colombia, Vancouver, BC, Canada. 8Geriatric Sleep Center, Edouard Herriot University Hospital, HCL, Lyon, France. 9Dept of Geriatrics, Bichat University Hospital, APHP and INSERM U669, Paris, France. 10Institute for Rehabiltation Research, Hospital Norderney, Norderney, Germany. 11Respiratory Dept, La Fe University and Polytechnic Hospital, Valencia, Spain. 12Dept of Geriatric Medicine, Kliniken Essen Mitte, Essen, Germany. Correspondence: Nikolaus C Netzer, Hermann Buhl Institute for Hypoxia and Sleep Medicine Research, Ghersburg Clinic for Geriatric Rehabilitation, Ghersburgstr. 9, 83043 Bad Aibling, Germany. Email: [email protected] ABSTRACT Sleep disordered breathing (SDB) is a leading cause of morbidity worldwide. -

The Relationship Between the Components of Idiopathic Focal Epilepsy
Journal of Pediatrics and Neonatal Care Review Article Open Access The relationship between the components of idiopathic focal epilepsy Abstract Volume 8 Issue 3 - 2018 The classification of epileptic syndromes in children is not a simple duty, it requires Cesar Ramon Romero Leguizamon a great clinical ability as well as some degree of experience. Until today there is no Department of Drug Design and Pharmacology, University of international consensus regarding the different diseases that are part of the Idiopathic Copenhagen, Denmark Focal Epilepsies However, these diseases are the most prevalent in children suffering from some type of epilepsy, for this reason it is important to know more about these, Correspondence: Cesar Ramon Romero Leguizamon their clinical characteristics, pathological findings in studies such as encephalogram, M.D., Department of Drug Design and Pharmacology Faculty resonance, polysomnography and others. In the same way, to explore the possible of Health and Medical Science, University of Copenhagen, genetic origins of many of these pathologies, that have been little explored and Denmark, Jagtev 160, 2100 Copenhagen, Denmark, become an important therapeutic goal. A description of the most relevant aspects of Email [email protected] atypical benign partial epilepsy, Landau-Kleffner syndrome, benign epilepsy with centrotemporal spikes, electrical status epilepticus during sleep and Panayiotopoulos Received: February 17, 2018 | Published: May 14, 2018 syndrome is presented in this review, Allowing physicians and family members of children suffering from these diseases to have a better understanding and establish in this way a better diagnosis and treatment in patients, as well as promote in the scientific community the interest to investigate more about these relevant pathologies in childhood.