Methicillin-Resistant Staphylococcus Aureus: a Public Health Issue with Economic Consequences
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Film Reference Guide
REFERENCE GUIDE THIS LIST IS FOR YOUR REFERENCE ONLY. WE CANNOT PROVIDE DVDs OF THESE FILMS, AS THEY ARE NOT PART OF OUR OFFICIAL PROGRAMME. HOWEVER, WE HOPE YOU’LL EXPLORE THESE PAGES AND CHECK THEM OUT ON YOUR OWN. DRAMA 1:54 AVOIR 16 ANS / TO BE SIXTEEN 2016 / Director-Writer: Yan England / 106 min / 1979 / Director: Jean Pierre Lefebvre / Writers: Claude French / 14A Paquette, Jean Pierre Lefebvre / 125 min / French / NR Tim (Antoine Olivier Pilon) is a smart and athletic 16-year- An austere and moving study of youthful dissent and old dealing with personal tragedy and a school bully in this institutional repression told from the point of view of a honest coming-of-age sports movie from actor-turned- rebellious 16-year-old (Yves Benoît). filmmaker England. Also starring Sophie Nélisse. BACKROADS (BEARWALKER) 1:54 ACROSS THE LINE 2000 / Director-Writer: Shirley Cheechoo / 83 min / 2016 / Director: Director X / Writer: Floyd Kane / 87 min / English / NR English / 14A On a fictional Canadian reserve, a mysterious evil known as A hockey player in Atlantic Canada considers going pro, but “the Bearwalker” begins stalking the community. Meanwhile, the colour of his skin and the racial strife in his community police prejudice and racial injustice strike fear in the hearts become a sticking point for his hopes and dreams. Starring of four sisters. Stephan James, Sarah Jeffery and Shamier Anderson. BEEBA BOYS ACT OF THE HEART 2015 / Director-Writer: Deepa Mehta / 103 min / 1970 / Director-Writer: Paul Almond / 103 min / English / 14A English / PG Gang violence and a maelstrom of crime rock Vancouver ADORATION A deeply religious woman’s piety is tested when a in this flashy, dangerous thriller about the Indo-Canadian charismatic Augustinian monk becomes the guest underworld. -

Press of Ireland
Technical specifications 78 mins/ colour/ 2 :35/ 5.1 PRODUCED BY DANIEL MORIN DIRECTED BY ALAIN VÉZINA ÉDITH CÔTÉ DEMERS, ALEXANDRE LANDRY AND RAYMOND BOUCHARD FILMOPTION INTERNATIONAL PRESENTS A BORÉAL PRODUCTION DEATH DIVE PRODUCER DANIEL MORIN LINE PRODUCER DANIELLE LACHANCE WRITTEN AND DIRECTED BY ALAIN VÉZINA WITH ÉDITH CÔTÉ DEMERS, ALEXANDRE LANDRY, BÉATRICE PICARD, JEAN-GUY BOUCHARD, LUC PILON, PIERRE MAILLOUX, ÉRIC GAGNÉ AND RAYMOND BOUCHARD DIRECTOR OF PHOTOGRAPHY JEAN KAVANAGH ART DIRECTOR GUILLAUME COUTURE COSTUME DESIGNER CLAIRE NADON MAKE-UP AND SPECIAL EFFECTS DESIGNER MARIO SOUCY EDITOR MARC PLANA AND ALAIN BARIL SOUNDEDITOR AND SOUND DESIGNER ORIGINAL SCORE JEAN-FRANÇOIS ROY REJEAN DOYON PRODUIT AVEC LA PARTICIPATION FINANCIÈRE DE ET EN PARTENARIAT AVEC CrCréditédit d'impd'impôtôt pour production cincinématographiqueématographique ou magnmagnétoscopiqueétoscopique canadienne DEATH DIVE > 2 DEATH DIVE A ghost ship with its crew massacred is discovered along the Gaspé coast… Quebec’s first zombie-slasher film. Synopsis A salvage ship found adrift with its crew massacred off the Gaspé coast sets off a mysterious quest to find the culprit! An ambitious journalist, who elicits the help of a shy, sedentary young museum archivist, comes to believe that a shady collector of maritime objects may well be linked to the tragic events. Thus begins a race to discover the identity of the mysterious dark hand murdering everything in its path while recovering priceless artifacts from the century old wreck of the “Princess of the North” that took the lives of so many... Distribution Alexandre Landry – Alexandre Archivist and curator employed by the Baie-du-Nord Sea Museum, he harbours resentment towards Sauvageau, whom he portraits as an unfair competitor. -
DP LCEA VA.Pdf
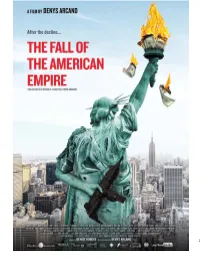
1 The Fall of the American Empire After the decline… the fall. We are all subjects of the American Empire. The moral rot of the Empire has started to infect us. Money’s omnipotence is but one of the symptoms. Will we find antibiotics powerful enough to fight the gangrene? - Denys Arcand Synopsis Pierre-Paul Daoust, 36, an intellectual with a PhD in philosophy is forced to work as a deliveryman to afford a decent living. One day, while delivering a parcel, he gets caught in a hold up gone terribly wrong: two dead and millions in money bags laying on the ground. Pierre-Paul is confronted with a dilemma leave empty handed, or take the money and run? This new Denys Arcand film takes a witty yet touching look at, as only Arcand knows how, the predominance of money in a society where all other values seem to have crumbled. 1 Denys Arcand Director & screenwriter An Academy Award winning director, Denys Arcand's films have won over 100 prestigious awards around the world. In 2003, he wrote and directed The Barbarian Invasions which was nominated for Best Original Screenplay and won the Oscar for Best Foreign Language Film. In France, it won three César – Best Film, Best Screenplay and Best Director; in Italy, the Donatello for Best Foreign Language Film; at the Cannes Film Festival, the Best Actress and Best Screenplay awards, amongst many. In 1989, Denys Arcand directed the powerful Jesus of Montreal which won the Jury’s Grand Prize and the Ecumenical Prize in Cannes. The film also earned 12 Genie Awards in addition of being nominated for the Oscar in the Best Foreign Language Film category. -

26 Years of French Film in BC
PRESS RELEASE #RVCQF2020 FOR IMMEDIATE RELEASE Vancouver January 28, 2020 26 years of French film in BC The film LE DERNIER NATAQ (The Last Nataq) by Lisette Marcotte will open the 26th Edition of Rendez-vous du cinéma québécois et francophone de Vancouver, on February 5, 2020 at 6:00 pm at SFUW. Richard Desjardins wrote a masterpiece– Nataq. In this documentary, Lisette Marcotte goes in quest of the spirit of the place where they were both born. The film is built on the breadcrumb trail of the mural created in tribute to the poetry of Desjardins in Rouyn-Noranda. Twenty years after L’erreur boréale, he shares his thoughts on the major environmental issues and his love for his homeland. Produced by Les Productions La vie devant soi Inc. The closing night at Auditorium Jules-Verne features VAILLANCOURT REGARDE SI C’EST BEAU (Vaillancourt: Isn’t beautiful?) a documentary by John Blouin His monumental sculptures, often constructed as public performance, paved the way for contemporary art in Quebec. Born in 1929, Armand Vaillancourt is a towering figure of rebellion. A revolutionary and a tireless militant for the dream of a Quebec nation, Vaillancourt is also one of our pioneering ecologists, whose works explore the visceral connection between nature and creation. Treated with kid gloves by a deeply sympathetic documentarian, Vaillancourt has never been more voluble, sharing his love of materials and his astonishingly sharp, modern take on things. A portrait of a legendary force of nature. The film will be screened at Jules Verne Auditorium on Sunday, February 16 at 7:30 pm, preceded by a Master Class by Armand Vaillancourt at 6:30 pm. -

LES PRIX ÉCRANS CANADIENS 2014 Nominations Dans Les
LES PRIX ÉCRANS CANADIENS 2014 Nominations dans les catégories en Cinéma TORONTO | MONTRÉAL, 13 janvier 2014 BEST MOTION PICTURE / MEILLEUR FILM Sponsor / Commanditaire | William F. White International and Comweb Group LE DÉMANTÈLEMENT / THE AUCTION – Bernadette Payeur, Marc Daigle EMPIRE OF DIRT – Jennifer Podemski, Geoff Ewart, Heather K. Dahlstrom ENEMY – Kim McCraw, Luc Déry, Miguel A. Faura, Niv Fichman, Sari Friedland THE F-WORD – Andre Rouleau, David Gross, Macdara Kelleher GABRIELLE – Kim McCraw, Luc Déry THE GRAND SEDUCTION – Roger Frappier, Barbara Doran MAÏNA – Karine Martin, Michel Poulette, Yves Fortin TOM À LA FERME / TOM AT THE FARM – Charles Gillibert, Nathanaël Karmitz, Xavier Dolan ACHIEVEMENT IN ART DIRECTION/PRODUCTION DESIGN / MEILLEURE DIRECTION ARTISTIQUE MARIO HERVIEUX – Le Démantèlement / The Auction PATRICE VERMETTE – Enemy MICHEL PROULX – Louis Cyr, l’homme le plus fort du monde / Louis Cyr: The Strongest Man in the World JEAN BÉCOTTE – Maïna ANTHONY IANNI, FRANÇOIS SEGUIN – The Mortal Instruments: City of Bones ACHIEVEMENT IN COSTUME DESIGN / MEILLEURS COSTUMES LEA CARLSON – The Colony CARMEN ALIE – Louis Cyr, l’homme le plus fort du monde / Louis Cyr: The Strongest Man in the World VÉRONIQUE MARCHESSAULT – Maïna SARAH MILLMAN – Molly Maxwell GERSHA PHILLIPS – The Mortal Instruments: City of Bones ACHIEVEMENT IN CINEMATOGRAPHY / MEILLEURES IMAGES NICOLAS BOLDUC CSC – Enemy ALLEN SMITH – Maïna ANTONIO RIESTRA – Mama FRANÇOIS DELISLE – Le Météore / The Meteor PIERRE GILL, CSC – Upside Down ACHIEVEMENT IN DIRECTION -
LYRIQ BENT Winner on Canada’S Talent
Fall 2016 Inaugural TIFF issue! LYRIQ BENTThe Canadian Screen Award winner on why this country is becoming a global production power player What do Canadians want (to watch)? We have the answers inside And the nominees are… Check out who’s up for the 2016 CMPA Feature Film Producer Awards at TIFF Q&As with Canada’s talent 31 Q&A: Kim Todd Service stereotypes and IP ownership 40 Q&A: David Way Why authenticity matters 50 Q&A: Jay Bennett Brave new worlds 64 Q&A: Mike Volpe Laughing all the way 74 Q&A: Jillianne Reinseth Engaging children (and parents) 8 Cover feature The Canadian Screen Award Page 11 Page 42 LYRIQ BENT winner on Canada’s talent Features Page 55 Page 83 2 Reynolds Mastin 48 Taken A letter from the President Tackling a tough topic and CEO of the CMPA with empathy 11 Canadian Film Pictured (top to bottom): Black Code, Giants of Africa, Nelly Pictured (top to bottom): X Quinientos, Maudie, Maliglutit (Searchers) Pictured (top to bottom): Mean Dreams, Anatomy of Violence, Pays 4 The Big Picture 61 Feeling the Love! 32 Foreign Location · A look at TV, film and media A data-driven case for Service Production Film across Canada made-in-Canada content 41 Canadian THE 6 And the Nominees Are… 62 Behind the Scenes Documentary Film Leads negotiations with unions, broadcasters and funders The CMPA Feature Film A photographic look at filming Producer Awards and production across Canada Explores new digital and international business models 51 Canadian TV ∙ Builds opportunities for established and emerging content creators 72 Changing the Channel Drama CMPA Women in production 65 Canadian TV ∙ 86 The Indiescreen Listicle Comedy Through international delegations, best-in-class professional development, mentorship programs and more, Which Canadian film are you? the CMPA advances the interests of Canada’s indie producers. -
150 Canadian Films
150 CANADIAN FILMS MESSAGE FROM THE PRIME MINISTER OF CANADA Dear Friends: I am delighted to extend my warmest greetings to Canadians on National Canadian Film Day, a Canada 150 Signature Project, presented by REEL CANADA. This one-day event connects Canadians from sea to sea to celebrate the achievements of Canadian filmmakers. The film festival is one of many cultural projects during the Sesquicentennial year that will help build a sense of pride in and attachment to everything our remarkable country represents. National Canadian Film Day focuses on discovery, with opportunities to view culturally diverse Canadian films on television, online and in theatres large and small across the country. I would like to commend REEL CANADA for coordinating this exciting celebration of homegrown film excellence and I encourage everyone to get involved. With so many works to choose from, and an audience eager to explore the best of Canada’s rich film history, National Canadian Film Day is sure to be a resounding success. On behalf of the Government of Canada, I offer my best wishes for an enjoyable and memorable experience. Justin P.J. Trudeau Prime Minister of Canada The Rt. Hon. Justin P.J. Trudeau, P.C., M.P. Prime Minister of Canada MESSAGE FROM THE MINISTER OF CANADIAN HERITAGE As we kick off the 150th anniversary of Confederation, we want to support projects that inspire national pride and strengthen the bonds between citizens from coast to coast to coast. This is why we are pleased to support REEL CANADA and its National Canadian Film Day 150. -

Speech by Carolle Brabant, APA 2013
Talent First Annual Report 2012-2013 Address by Carolle Brabant, Executive Director, delivered at Telefilm’s Annual Public Meeting, held at the PHI Centre in Montreal on Wednesday, December 11, 2013, 10 a.m. “Creativity, expertise, partnerships and promotion are key to our film industry’s future.” Carolle Brabant Thank you, Mr. Roy. Good morning Ladies and Gentlemen, dear clients and colleagues. It’s my turn also to thank Phoebe Greenberg for her warm welcome. I appreciate Phoebe’s work very much. She isn’t afraid of challenges, or of change. She’s a true creative spirit. Thank you Phoebe. Three years ago, together with our clients and partners, we decided to foster Canadian cultural success. How? By highlighting the value of Canadian talent, everywhere across the country. I’m now in my fourth year as Telefilm’s Executive Director, and I can tell you that I’m as enthusiastic and convinced as ever that this approach is the right one. Let me tell you why in six key words: stories, expertise, platforms, audiences, partnerships and promotion. Good stories Let’s start with “good stories.” And let me tell you, there’s no shortage of creative talent in our country who can tell a good story. Our cinema is fascinating and appealing. Our creators explore subjects that are very much of our time—love, old age, immigration, family strife, solitude, the will to succeed, intolerance or social inequality. Our filmmakers tell stories that are serious, that are often very moving—but that can also make us laugh and smile. There are characters and images that stay with us for a long time. -

Dossier De Presse
GABRIELLE scénario et réalisation Louise Archambault avec Gabrielle Marion-Rivard, Alexandre Landry, Mélissa Désormeaux-Poulin Vincent-Guillaume Otis, Benoit Gouin, Sébastien Ricard Isabelle Vincent, Marie Gignac, Véronique Beaudet et avec la participation de Robert Charlebois, Gregory Charles les étudiants de l’École Les Muses et la Gang à Rambrou musique originale et arrangements : François Lafontaine chef de chœur et arrangements chorale : Hélène-Élise Blais producteurs Luc Déry et Kim McCraw DOSSIER DE PRESSE relations de presse IXION Communications (514) 495.8176 [email protected] résumé Gabrielle est une jeune femme atteinte du syndrome de Williams qui possède une joie de vivre contagieuse et un don exceptionnel pour la musique. Elle a rencontré son amoureux Martin au centre de loisirs où ils font partie d’une chorale et depuis, ils sont inséparables. Mais en raison de leur différence, leur entourage ne leur permet pas de vivre cet amour comme ils l'entendent. Au moment où le groupe se prépare pour un important festival de musique, Gabrielle fait tout pour prouver son autonomie et gagner son indépendance. Déterminée, elle devra affronter les préjugés et ses propres limites pour espérer vivre avec Martin une histoire d'amour qui n’a rien d’ordinaire. GABRIELLE | Dossier de presse | 2013 1 liste des comédiens Gabrielle Gabrielle MARION-RIVARD Sophie Mélissa DÉSORMEAUX-POULIN Martin Alexandre LANDRY Rémi Vincent-Guillaume OTIS Laurent Benoit GOUIN Raphaël Sébastien RICARD Mère de Gabrielle Isabelle VINCENT Mère -
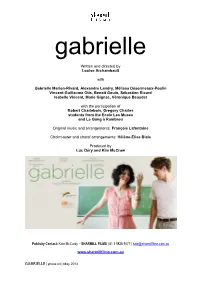
Written and Directed by Louise Archambault with Gabrielle Marion
gabrielle Written and directed by Louise Archambault with Gabrielle Marion-Rivard, Alexandre Landry, Mélissa Désormeaux-Poulin Vincent-Guillaume Otis, Benoit Gouin, Sébastien Ricard Isabelle Vincent, Marie Gignac, Véronique Beaudet with the participation of Robert Charlebois, Gregory Charles students from the École Les Muses and Le Gang à Rambrou Original music and arrangements: François Lafontaine Choirmaster and choral arrangements: Hélène-Élise Blais Produced by Luc Déry and Kim McCraw Publicity Contact: Kate McCurdy – SHARMILL FILMS | 61 3 9826 9077 | [email protected] www.sharmillfilms.com.au GABRIELLE | press kit | May 2014 synopsis Gabrielle is a young woman with Williams syndrome who has a contagious joie de vivre and an exceptional musical gift. Since she met her boyfriend Martin, at the recreation centre where they are choir members, they have been inseparable. However, because they are “different,” their loved ones are fearful of their relationship. As the choir prepare for an important music festival, Gabrielle does everything she can to gain her independence. As determined as she is, Gabrielle must still confront other people’s prejudices as well as her own limitations in the hope of experiencing an extraordinary love with Martin. GABRIELLE | press kit | May 2014 cast Gabrielle Gabrielle MARION-RIVARD Sophie Mélissa DÉSORMEAUX-POULIN Martin Alexandre LANDRY Rémi Vincent-Guillaume OTIS Laurent Benoit GOUIN Raphaël Sébastien RICARD Gabrielle’s mother Isabelle VINCENT Martin’s mother Marie GIGNAC Recreation centre worker -

Paris, Le 7 Avril 2005
42, rue René Boulanger | 75010 | Paris R.C.S. de Paris : B 481 518 405 (2005B05959) SIRET : 481 518 405 00024 T.V.A. : FR 90 481 518 405 PHONE: + 33 1 42 40 12 84 FAX: + 33 9 57 73 07 66 MOBILE: + 33 6 14 45 62 78 SKYPE: matteolovadina EMAIL: [email protected] WEB: www.reelsuspects.com PRINTER FRIENDLY LOVE IN THE TIME OF CIVIL WAR A film by Rodrigue JEAN 120 min, CANADA, 2014 Colour, 2:35, HD & DCP SHORT SYNOPSIS Alex is a young addict who sells his body in Montreal. He's flanked by Bruno, Simon, Jeanne, Eric and Velma, all of them caught in the same spiral of compulsion. Hostage to society's market logic, they are the fallen angels of a dark and violent time. LONG SYNOPSIS Alex's days are completely organized around doing drugs or getting the money to buy them through hustling, running errands for dealers, or committing petty crimes (most often muggings of potential johns). He shuffles from one dingy, depressing apartment to the next, sometimes on his own, sometimes in the company of fellow addicts from whom he hopes to cop a fix — though he frequently ends up getting ripped off himself. These shooting-up sessions usually involve sex as part of the package, but the sex itself seems less a matter of pleasure than a brief coming up for air before plunging back into the depths of the fix. In the hermetically sealed existence that Alex and his associates have made for themselves, the outside world is alien terrain: when Alex is forced to leave an apartment and walk down the street, he might as well be walking on the moon. -

Texte Intégral (PDF)
Document généré le 1 oct. 2021 11:30 Revue d'histoire de l'Amérique française Index K à O Index des volumes XI-XX (juin 1957 - mars 1967) Index, 1967 URI : https://id.erudit.org/iderudit/305696ar DOI : https://doi.org/10.7202/305696ar Aller au sommaire du numéro Éditeur(s) Institut d'histoire de l'Amérique française ISSN 0035-2357 (imprimé) 1492-1383 (numérique) Découvrir la revue Citer ce document (1967). Index K à O. Revue d'histoire de l'Amérique française, 195–275. https://doi.org/10.7202/305696ar Tous droits réservés © Institut d'histoire de l'Amérique française, 1967 Ce document est protégé par la loi sur le droit d’auteur. L’utilisation des services d’Érudit (y compris la reproduction) est assujettie à sa politique d’utilisation que vous pouvez consulter en ligne. https://apropos.erudit.org/fr/usagers/politique-dutilisation/ Cet article est diffusé et préservé par Érudit. Érudit est un consortium interuniversitaire sans but lucratif composé de l’Université de Montréal, l’Université Laval et l’Université du Québec à Montréal. Il a pour mission la promotion et la valorisation de la recherche. https://www.erudit.org/fr/ INDEXXI-XX 195 K KAGE, Joseph, thèse, XX: 521. XVI: 508, 522; XVIII: 591; ses KALM, Pierre, botaniste, XI: 242, bals, XI: 500. 262; XIII: 179, 517, 524; XIV: KENDALL, Edward A., et la tradition 31, 32, 217; XV: 334, 609; XVII: du débarquement de Miguel Corte- 9; XVIII: 608; XX: 424; son Real au Mass., XIX: 344. voyage au Canada, XIV: 122-125; KENRICK, Peter R., archevêque ce qu'il dit des Canadiennes en de St.